Abstract
Background
Reverse total shoulder arthroplasty has been used to treat rotator cuff tear arthropathy, proximal humeral fractures and for failed conventional total shoulder prostheses. It has been suggested that polyethylene wear is potentially higher in reverse shoulder replacements than in conventional shoulder replacements. The modes and degree of polyethylene wear have not been completely elucidated. The purpose of this study was to evaluate polyethylene wear patterns in seven specimens retrieved at revision arthroplasty and identify factors that may be associated with increased wear.
Methods
Reverse total shoulder components were retrieved from 7 patients during revision arthroplasty for loosening and/or pain. Pre-operative glenoid tilt and placement, and scapular notching were evaluated using pre-operative radiographs. Polyethylene wear was evaluated using microCT and optical microscopy.
Results
Wear on the rim of the polyethylene humeral cup, was identified on all retrieved components. The extent of rim wear varied from a penetration depth of 0.1 to 4.7 mm. We could not demonstrate a correlation between scapular notching and rim wear. However, rim wear was more extensive when the inferior screw had made contact with the liner. Metal on metal wear between the humeral component and the inferior screw of one component was also observed. Wear of the intended bearing surface was minimal.
Discussion
Rim damage was the predominant cause of polyethylene wear in our retrieved specimens. Direct contact between the humeral component and inferior metaglene screws is concerning because this could lead to accelerated UHMWPE wear and also induce mechanical loosening of the glenoid component.
Keywords: Reverse Total Shoulder Arthroplasty, UHMWPE, Impingement, Scapular Notching, Wear, Retrieval
Introduction
Reverse total shoulder arthroplasty was developed specifically for the treatment of rotator cuff tear arthropathy but has also been used for the treatment of proximal humeral fractures and their sequelae and for failed conventional total shoulder prostheses. In short term studies, favorable results have been reported with respect to pain and function2,3,8,9,11,23,24,26,30. The potential for ultra high molecular weight polyethylene (hereafter referred to as polyethylene) wear is substantial, given the relatively large surface area of contact. However, studies defining the type and extent of polyethylene wear are sparse. Recently, Nam and colleagues reported on 14 retrieved specimens and noted that inferior quadrant wear was most common 18. However, no distinction was made between wear on the articulating surface versus the component rim. Scapular notching was present in 6 of 14 specimens and was correlated with inferior component deformation but was not correlated with inferior component abrasive wear. Scapular notching describes bone loss along the scapular neck, most commonly inferiorly, that is thought to be caused by mechanical impingement between the ultra-high molecular weight polyethylene (hereafter referred to as polyethylene) liner of the humeral implant and the scapula 15,20,30. However, more severe grades of scapular notching may occur via two processes: (1) the mechanical impingement described above in concert with (2) an osteolytic reaction brought on by the presence of polyethylene wear debris within the joint space 2,9,15,20,21,30.
Impingement has been a source of concern in other joint replacements such as the hip or spine, as well as in conventional total shoulder replacement. In the hip, impingement of the neck of the femoral component against the rim of the acetabular liner gives rise to concerns about rim fracture, particularly in highly crosslinked polyethylenes 5,12. In the spine, Kurtz and colleagues found that impingement led to higher oxidation on the rims of Charité cores 13. In a recent study by Nho, et al., impingement, as evidenced by abrasion on the inferior rim of polyethylene glenoid components, was present in 37% of retrieved unconstrained total shoulder replacements. In conforming total shoulder designs, this led to severe polyethylene wear and was thought to play a possible role in observed radiolucencies 19.
In addition to any wear debris generated by impingement, reverse total shoulder replacement designs are expected to produce greater amounts of polyethylene wear at the bearing surface than their conventional counterparts, largely because of the increased surface area of contact 27. While the clinical significance and prevalence of polyethylene wear at the bearing surface and/or impingement in reverse total shoulder replacement remains unclear, both are potential areas of concern because of the potential association between polyethylene wear debris and aseptic component loosening. Polyethylene impingement against the scapula may be of particular concern because of the possibility of accelerated polyethylene wear and progressive osteolysis or notching. Although polyethylene wear debris is considered a possible culprit in severe scapular notching and component loosening, there is little literature describing the extent, prevalence, or sources of polyethylene wear in reverse total shoulder replacement.
The purposes of this study were to evaluate polyethylene wear patterns in seven consecutive specimens retrieved at the time of revision arthroplasty. Radiographic parameters, such as scapular notching and glenoid component positioning, were examined in order to identify factors that may be associated with increased polyethylene wear. We hypothesized that, because of bony impingement, wear would be much greater at the rim of the component as opposed the intended bearing surface. We also hypothesized that the degree of notching seen in radiographs would correlate to the amount of impingement and polyethylene wear that was evident in the retrieved devices.
Methods
At each authors’ respective institution, an Institutional Review Board (IRB) reviewed and approved the protocol for this study. Specimens were obtained by three trained shoulder surgeons (GRW, CLG, MLR). Retrieval analysis was conducted at a university retrieval laboratory (Implant Research Center, Drexel University).
Seven (7) reverse total joint replacements were consecutively retrieved after revision surgery at a single institution under an IRB approved protocol. These devices were all revised for pain and/or loosening (Table 1). Three patients had both humeral and glenoid loosening. Two patients had loosening of only the humeral component. One patient was revised for impingement of the greater tuberosity on the acromion. One patient was revised for extreme deltoid based pain, presumed to be from partial axillary nerve palsy and deltoid over tensioning. For the purposes of this study, loosening was defined as the presence of gross motion, visible to the naked eye, between the component and bone at the time of revision surgery. (Table 1).
Table 1.
Clinical information for the 7 retrieved devices.
| Patient | Age at Implantation | Gender | Primary Diagnosis | Revision Diagnosis | Implantation Time (years) | Glenosphere Position* | Glenosphere Tilt | Notching Score |
|---|---|---|---|---|---|---|---|---|
| 3 | 57 | F | Failed Hemi post Fracture | Humeral and Glenoid Loosening | 1.6 | Low | Neutral | 1 |
| 8 | 75 | F | Failed Hemi post Fracture | Humeral Loosening | 1.8 | Low | Neutral | 0 |
| 23 | 68 | M | Rotator Cuff Arthropathy | Humeral and Glenoid Loosening | 3.3 | ** N/A | ** N/A | ** N/A |
| 25 | 80 | F | Failed Hemi post Fracture | Humeral Loosening | 2.3 | Low | 10° Inferior | 2 |
| 26 | 59 | M | Rotator Cuff Arthropathy | Pain/Impingement | 1.8 | Low | Neutral | 1 |
| 29 | 83 | F | Rotator Cuff Arthropathy | Humeral and Glenoid Loosening | 2.7 | ** N/A | ** N/A | ** N/A |
| 32 | 73 | F | Malunion/Cuff Tear | Pain/Deltoid overlengthening | 1.3 | Low | 10° Inferior | 1 |
Low glenosphere position is the recommended position.
N/A = Not Available due to catastrophic glenoid failure or poor radiograph quality.
The initial surgical approach was deltopectoral in all cases. Six of the seven patients underwent reverse shoulder replacement for revision from a painful hemiarthroplasty. Three hemiarthroplasties were placed for proximal humerus fractures and three for rotator cuff tear arthropathy. One patient under went the reverse replacement for malunion of a three part proximal humerus fracture. Patient demographics (i.e. age, handedness, etc.) were obtained from available patient records.
Infection or presumed infection was present in two patients. All patients had pre-operative white blood cell count, sedimentation rate, and C-reactive protein for screening. No patient underwent aspiration. Operative cultures were held for seven to ten days. Patient number 29, who had a catastrophic failure, had normal pre-operative infection workup and normal appearing intra-operative tissue but grew out Propionibacterterium acnes from the intra-operative cultures. The patient was treated with six weeks of intravenous vancomycin. Patient number 23 had normal infection workup but abnormal appearing fluid at the time of retrieval. An antibiotic spacer was placed for presumptive treatment of infection. Intra-operative cultures were negative. The patient received six weeks of antibiotics and was reimplanted three months after removal of the original prosthesis.
Radiographic Review
Pre-revision radiographs were available for review for all patients. The extent and presence of scapular notching was assessed by two surgeons (GW and CG). Scapular notching was graded on a scale from 0 to 4 according to the Nérot method originally described by Valenti29. A score of 0 indicates no notching; 1 describes a small notch where the defect only concerns the pillar. A score of 2 describes a notch that has become stable, whereas a score of 3 is given when there is a progressing notch that begins erosion of the inferior screw. Grade 4 is given when there is extension of the notch under the baseplate and glenoid loosening from notching first begins. In one case, there was a complete catastrophic failure of the glenoid, which made scoring that patient impossible. In another, the pre-operative films were of too poor of quality to assess notching.
All available films prior to the retrieval surgery were reviewed to assess placement of the glenoid baseplate and glenosphere component by two fellowship trained shoulder surgeons (GRW, CLG). One patient presented with catastrophic failure and with no immediate post implantation films available. One patient had inadequate films to assess glenoid baseplate position.
Retrieval Analysis
Following removal, the retrieved components were cleaned and disinfected by gently brushing the components in a bleach solution followed by 60 minutes in an ultrasonicator to remove any loose debris prior to analysis.
The polyethylene components were inspected using optical microscopy. The extent and presence of wear on the articulating surface was assessed using a modified Hood technique10. The polyethylene inserts were graded for seven different modes of wear (burnishing, scratching, embedded debris, pitting, surface deformation, abrasion and delamination) on a scale from 0 to 3. A score of 0 was given where evidence of the wear mode was not present, a score of 1 was given when the wear was present on less than 10% of the surface, a score of 2 was given when the wear mode was observed on 10–50% of the surface, and a score of 3 was given when the damage was severe and covered more than 50% of the surface.
Rim damage was assessed by determining the extent of the rim circumference that exhibited rim damage. High-resolution micrographs were taken of each liner. Straight lines were drawn from the each edge of the region of rim damage to the center of the humeral liner. The angle formed by the two intersecting lines was measured using publically available image analysis software (NIH Image J).
MicroCT Analysis
The wear and damage to the polyethylene components were also assessed using microcomputed tomography (microCT). The components were scanned at 0.05 mm isotropic resolution (μCT80, Scanco Medical, Switzerland), to produce a full three-dimensional reconstruction of the polyethylene component. To assess wear on the intended articulating surface, an idealized 3-Dimensional sphere was registered with polyethylene surface as was originally described by Bowden 4. The extent of wear can then be determined by calculating the volume of polyethylene missing. Rim wear was assessed by calculating the depth of rim loss. The depth of rim damage in millimeters was calculated by counting the amount of micro-CT slices in which damage was apparent and multiplying this by the slice thickness or resolution (0.05 mm).
Results
Five of the devices were manufactured by Depuy (Delta III), one was manufactured by Zimmer (Inverse/Reverse Anatomical Shoulder), and one by Tornier. All of the devices employ a medialized center of rotation located on the native glenoid surface. The devices were implanted for an average of 1.9 years (Range: 1.3–3.3 y). The average age at implantation was 71 years (Range: 57–83 y) and five (71%) of the patients were female. They were implanted on the patient’s dominant side in 3/7 (43%) of the cases. Scapular notching could be scored radiographically for 5/7 (71%) patients. Of these, 1/5 was Grade 0, 3/5 were Grade 1, 1/5 was Grade 2, and 0/5 were Grade 3 (Table 1). Two patients could not be scored radiographically due to catastrophic glenoid failure or poor radiograph quality.
The position of the glenoid baseplate on the glenoid was appropriately low in the five patients with available films (Figure 1). Two patients (2/5) had a slight inferior tilt to the glenoid component and three (3/5) had no tilt.
Figure 1.
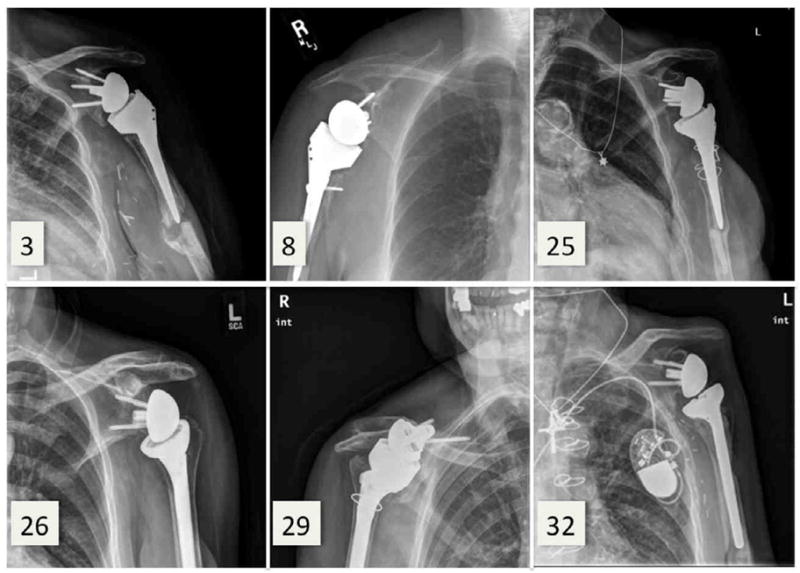
Preoperative revision radiographs. Note the catastrophic glenoid failure in Patient 29. Radiographs from Patient 23 are omitted due to poor radiographic quality.
Microscopic inspection of the articulating surface revealed that machining marks were visible on portions of the articulating surface, indicating low amounts of wear. Inspection of the registered micro-CT confirmed that little to no wear occurred at the articulating surface (Figure 2). Although only small amounts of wear were observed on the intended articulating surface, the dominant modes of observed articulating surface wear were burnishing, multidirectional scratching, and pitting (cumulative Hood score = 14, 13, 13, respectively). There was evidence of articulating surface abrasion in 3 of the devices (cumulative Hood score = 7) and 1 component that had slight evidence of delamination (cumulative Hood score = 1) on the articulating surface.
Figure 2.
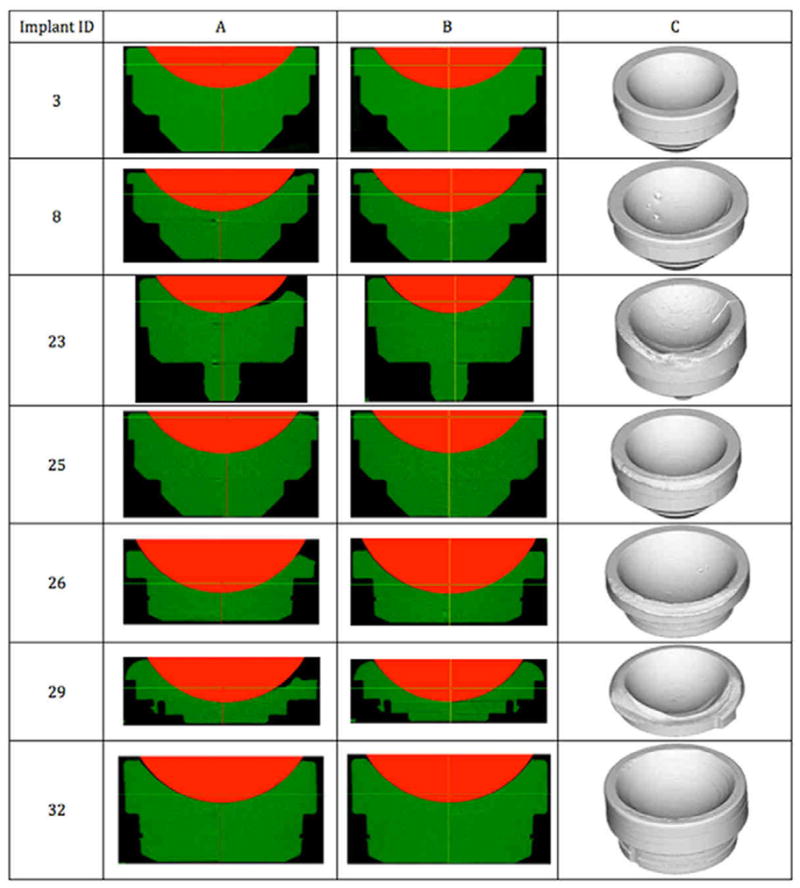
MicroCT data registered with idealized head (columns A and B) for all of the reverse shoulder arthroplasty retrievals. Column A is coronal plane from the middle of the implant while column B is the frontal plane. Column C is the three dimensional reconstruction of the microCT dataset.
All of the rims of the polyethylene components showed evidence of bony impingement with the scapula. However, the extent and depth of the impingement varied between the devices. The impingement region ranged from 87 – 226° (average: 136°) of the circumference of the rim. The depth of the impingement scar ranged from 0.1 mm to as much as 4.7 mm (average: 2.1 mm). We could discern no correlation between notching scores and the extent or depth of impingement at the rim. However, the most severe cases of rim wear were seen in the two specimens that demonstrated evidence of contact with the inferior locking screw.
As mentioned, two cases of extreme rim wear were observed. Both implants exhibited wear depths exceeding 4 mm and there was evidence of contact with the inferior screw. In the first case, the polyethylene rim wore all the way through to the metal baseplate. Grooves within the remaining polyethylene suggest that the rim was worn away by a combination of the scapula and subsequently the inferior screw. Inspection of the humeral metallic cup and inferior screw revealed metal on metal wear at this surface (Figure 3). In the second case, the rim appeared to be worn by the scapula and inferior screw, as in the first case. However, the inferior screw fractured (Figure 4) and the broken screw then became a new wear surface that created abrasive wear on intended bearing surface (Figure 4).
Figure 3.
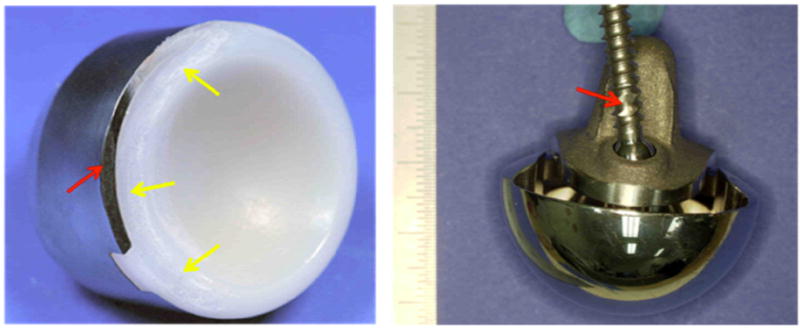
Retrieved reverse total shoulder implant that was implanted for 2.7 years. Note the extreme polyethylene wear at the rim (yellow arrows) as well as metal-on-metal contact (red arrows) (A). Note the metal wear on the inferior screw (B).
Figure 4.
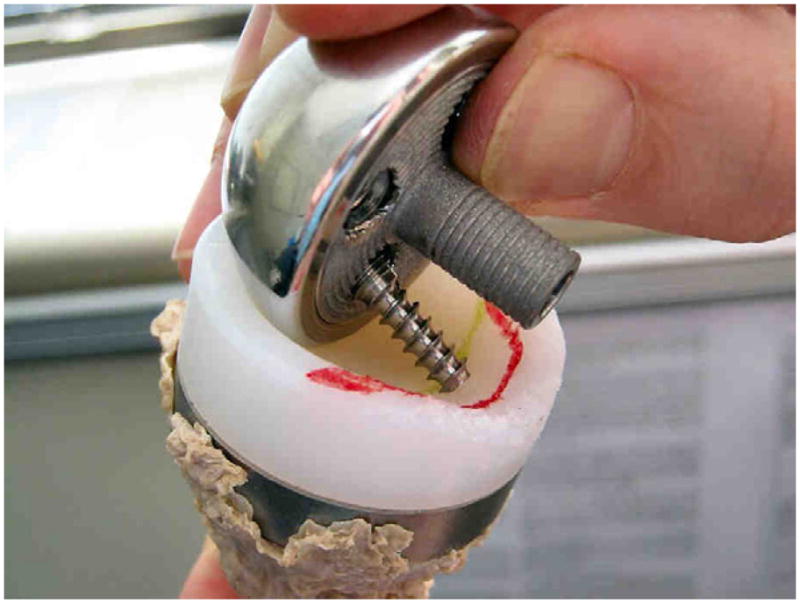
Retrieved reverse total shoulder implant that was implanted for 3.3 years with evidence of wear on the rim from the screw as well as abrasive wear on the intended bearing surface from the broken screw.
Discussion
Edge loading wear and impingement has been a cause for concern in many different forms of total joint replacement and may lead to rim fracture and the need for revision 1,12–14,28. Although impingement has been observed in conventional total shoulder replacements, there are only sporadic reports of evidence of impingement of the polyethylene glenoid of reverse shoulders with the exception of studies on scapular notching. Nam and colleagues recently reported on 14 retrieval specimens and noted inferior quadrant polyethylene wear was the most common wear pattern18. Although there was a strong correlation between scapular notching and inferior component deformation, there was no correlation between scapular notching and inferior component abrasive wear. They did not make a specific distinction between intended articulating surface and rim wear and did not note any association between inferior screw contact and severity of polyethylene wear. Their retrieved implants had been functioning for only 0.46 +/− .5 years. Additionally, their components were revised mainly for instability or infection, while the retrievals in our collection were revised primarily for loosening.
The predominant form of wear in our specimens was rim wear from impingement with the scapula and the inferior locking screw. There was almost no detectable wear on the bearing surface, even though the implants had been functioning for 1.9 years, on average (Range: 1.3–3.3 y). Therefore, our hypothesis that rim wear would be greater than articulating wear was correct. All of the polyethylene inserts in this study showed evidence of bony impingement at the rim. However the severity varied greatly and did not correlate with the scapular notching scores, contrary to our second hypothesis. This is likely because of the small number of cases and the relative lack of severe notching scores. However, we did note that the polyethylene rim wear was most severe in cases where the notch contacted the inferior screw. Rim damage has been mentioned in a handful of previous case reports, which mention that the polyethylene component of the retrieval displayed wear22. However, the majority of the studies do not report on the extent of rim wear in order to compare with our results 3,7,22. Nam and colleagues recently reported on 14 retrieved specimens in which inferior quadrant polyethylene wear was most common. However, wear on the intended articulating surface was grouped with rim wear when calculating the damage score, and therefore, separate analysis of rim and articulating surface wear was not included. Nyffeler et al. reported severe wear of the rim covering an arc of 120° and as deep as the metal tray 21 in a case study. Of particular concern are reported cases, as seen in our study, where there is evidence of wear between the inferior screw and the metal shell 15. This wear mechanism has the potential to release metal debris, which could have a negative clinical effect, especially in patients with metal hypersensitivity.
In addition to undesired metal on metal wear, the contact of the of the humeral component on the inferior locking screw may induce a moment on the glenoid component leading to distraction of the component at the superior glenoid as most inferior screws are locked to the baseplate. Assuming that the locking mechanism with the baseplate does not fail, contact between the inferior screw and the humerus could lead to premature mechanical loosening of the glenoid baseplate from a rocking mechanism or to a fatigue fracture of the inferior locking screw. The latter mechanism was observed in only one retrieval in our collection. The broken screw in this case subsequently created abrasive wear on the articulating surface of the humeral inlay (Figure 3).
There is currently debate in the literature about altering the glenoid component design and surgical technique to reduce scapular notching (and rim impingement). Factors that could potentially decrease impingement and notching include inferior placement of the glenoid sphere, decreased depth of the humeral cup, and lateralization of the glenoid center of rotation. Frankle et al., evaluated the Reverse Shoulder Prosthesis (Encore, DJO Surgical, Austin, Texas) and found zero incidence of scapular notching 8. However, Levy and Blum have recently described a case report where they observed scapular notching in the same design16. This design laterilizes the center of rotation 6 to 10 mm from the glenosphere. To date, our collection does not include any retrievals of this design to investigate the incidence of impingement. However, Nam and colleagues noted inferior quadrant wear in 5 implants of this type but a low incidence of radiographic notching. Despite the potential for decreased notching, some researchers are hesitant to adopt lateralization because of increases in the shear forces seen in the glenoid 3,6,17.
In designs where the center of rotation is medialized to the native glenoid surface (e.g. Delta III, Delta xtend, Tornier, etc.), scapular notching has been reported as occurring in anywhere from 25% to 96% of patients 2,3,9,11,15,23–26,30,31. The temporal progression of the severity of scapular notching still remains unclear. Previously, it was thought to occur rapidly and then become stable showing no progression 23–26,30. Recently, it has been suggested that the severity of the notch progresses with implantation time9,15. The clinical significance of scapular notching is also currently unknown, as studies have reported conflicting results with respect to correlating scapular notching scores with functional or pain scores 2,15,23,25,26,30
While we observed severe wear at the rim of some of our components, we did not observe an appreciable amount of wear on the intended articulating surface of the component. This was evident in the micro-CT analysis, as well as, in the observation that machining marks from manufacturing were still present on many of the articulating surfaces. In a finite element study by Terrier et al., it was predicted that reverse shoulders could generate as much as 5 times more wear than their anatomical shoulder counterparts27. Since we did not see significant wear on the intended articulating surface of our retrievals, it is possible that the loading paradigms used in these models do not apply to patients with reverse total shoulders.
We recognize that this study has several limitations, not the least of which is our small sample size. Although this limits the power for statistical testing, we were able to document evidence of impingement on all of our retrievals. Additionally, in two of our cases, the presence of contact between the inferior screw and the humeral component was either unrecognized or under appreciated on preoperative radiographs. This highlights the need for adequate, standardized pre-operative radiographs. Our observations are also limited to a population that was revised after a short term of implantation. Since reverse total shoulder arthroplasty has only been approved for use by the FDA since 2004, longer-term retrievals are, as of yet, unavailable at our institution. Future studies will allow for the assessment of the progression of impingement in mid to long-term implantation of reverse total shoulder replacement.
Conclusions
We have identified rim damage as the predominant source of polyethylene wear in a consecutive series of 7 retrieved reverse shoulders. Direct contact between the humeral component and inferior screws are of particular concern. Not only could this lead to the potential for accelerated wear of the polyethylene, but could also induce mechanical loosening of the glenoid component, especially in the presence of locking screws. In patients with scapular notching, true anteroposterior radiographs may help identify impingement between the inferior screw and the humeral component. Although we are unable to make clinical recommendations on the basis of this small study, removal of the inferior locking screw when notching is grade 2 or greater, especially in symptomatic patients, should at least be considered. Alterations in surgical technique (i.e. inferior glenoid component placement) and glenoid component design (offset glenoid spheres, variable angle locking screws, lateralization of the center of rotation) may lead to decreased contact between the humeral cup and the scapula or inferior glenoid screw. However, some of these alterations may have other negative consequences. Therefore, further studies are warranted to determine the clinical significance of this unintended wear mode of reverse total shoulder arthroplasty.
Footnotes
IRB: Each author certifies that all investigations were conducted in conformity with ethical principles of research and has been approved by the IRB boards at Drexel University (Project #: 1041261; Protocol # 16265) and the Rothman Institute at Jefferson University (NIH Control # 02F.387R).
Disclaimer: Institutional funding has been received from the National Institutes of Health (NIAMS) R01 AR47904 (JD, SM, MO, and SMK – Principle investigator). Dr. Gerald Williams is a consultant and receives royalties for Depuy and receives research support from Tornier. Dr. Charles Getz receives research support from Zimmer.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Birman MV, Noble PC, Conditt MA, Li S, Mathis KB. Cracking and impingement in ultra-high-molecular-weight polyethylene acetabular liners. J Arthroplasty. 2005;20:87–92. doi: 10.1016/j.arth.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15:527–40. doi: 10.1016/j.jse.2006.01.003. S1058-2746(06)00073-5 [pii] [DOI] [PubMed] [Google Scholar]
- 3.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14:147S–61S. doi: 10.1016/j.jse.2004.10.006. S1058274604002903 [pii] [DOI] [PubMed] [Google Scholar]
- 4.Bowden AE, Kurtz SM, Edidin AA. Validation of a micro-CT technique for measuring volumetric wear in retrieved acetabular liners. J Biomedical Materials Research. 2005;75:205–9. doi: 10.1002/jbm.b.30318. [DOI] [PubMed] [Google Scholar]
- 5.Currier BH, Currier JH, Mayor MB, Lyford KA, Collier JP, Van Citters DW. Evaluation of oxidation and fatigue damage of retrieved crossfire polyethylene acetabular cups. J Bone Joint Surg Am. 2007;89:2023–9. doi: 10.2106/JBJS.F.00336. [DOI] [PubMed] [Google Scholar]
- 6.De Wilde LF, Audenaert EA, Berghs BM. Shoulder prostheses treating cuff tear arthropathy: a comparative biomechanical study. J Orthop Res. 2004;22:1222–30. doi: 10.1016/j.orthres.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 7.ElMaraghy A, Devereaux M. Medial wear of the polyethylene component associated with heterotopic ossification after reverse shoulder arthroplasty. Can J Surg. 2008;51:E103–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The Reverse Shoulder Prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am. 2005;87:1697–705. doi: 10.2106/JBJS.D.02813. [DOI] [PubMed] [Google Scholar]
- 9.Grassi FA, Murena L, Valli F, Alberio R. Six-year experience with the Delta III reverse shoulder prosthesis. J Orthop Surg (Hong Kong) 2009;17:151–6. doi: 10.1177/230949900901700205. [DOI] [PubMed] [Google Scholar]
- 10.Hood RW, Wright TM, Burstein AH. Retrieval analysis of total knee prostheses: a method and its application to 48 total condylar prostheses. J Biomed Mater Res. 1983;17:829–42. doi: 10.1002/jbm.820170510. [DOI] [PubMed] [Google Scholar]
- 11.Kalouche I, Sevivas N, Wahegaonker A, Sauzieres P, Katz D, Valenti P. Reverse shoulder arthroplasty: does reduced medialisation improve radiological and clinical results? Acta Orthop Belg. 2009;75:158–66. [PubMed] [Google Scholar]
- 12.Kurtz SM, Austin MS, Azzam K, Sharkey PF, MacDonald DW, Medel FJ, et al. Mechanical properties, oxidation, and clinical performance of retrieved highly cross-linked Crossfire liners after intermediate-term implantation. J Arthroplasty. 2010;25:614–23. e1-2. doi: 10.1016/j.arth.2009.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kurtz SM, MacDonald D, Ianuzzi A, van Ooij A, Isaza J, Ross ER, et al. The natural history of polyethylene oxidation in total disc replacement. Spine (Phila Pa 1976) 2009;34:2369–77. doi: 10.1097/BRS.0b013e3181b20230. [DOI] [PubMed] [Google Scholar]
- 14.Kurtz SM, van Ooij A, Ross R, de Waal Malefijt J, Peloza J, Ciccarelli L, et al. Polyethylene wear and rim fracture in total disc arthroplasty. Spine J. 2007;7:12–21. doi: 10.1016/j.spinee.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 15.Levigne C, Boileau P, Favard L, Garaud P, Mole D, Sirveaux F, et al. Scapular notching in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2008;17:925–35. doi: 10.1016/j.jse.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Levy J, Blum S. Inferior scapular notching following encore reverse shoulder prosthesis. Orthopedics. 2009;32 doi: 10.3928/01477447-20090818-23. [DOI] [PubMed] [Google Scholar]
- 17.Middernacht B, De Roo PJ, Van Maele G, De Wilde LF. Consequences of scapular anatomy for reversed total shoulder arthroplasty. Clin Orthop Relat Res. 2008;466:1410–8. doi: 10.1007/s11999-008-0187-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nam D, Kepler CK, Nho SJ, Craig EV, Warren RF, Wright TM. Observations on retrieved humeral polyethylene components from reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19:1003–12. doi: 10.1016/j.jse.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 19.Nho SJ, Ala OL, Dodson CC, Figgie MP, Wright TM, Craig EV, et al. Comparison of conforming and nonconforming retrieved glenoid components. J Shoulder Elbow Surg. 2008;17:914–20. doi: 10.1016/j.jse.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 20.Nyffeler RW, Werner CM, Gerber C. Biomechanical relevance of glenoid component positioning in the reverse Delta III total shoulder prosthesis. J Shoulder Elbow Surg. 2005;14:524–8. doi: 10.1016/j.jse.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Nyffeler RW, Werner CM, Simmen BR, Gerber C. Analysis of a retrieved delta III total shoulder prosthesis. J Bone Joint Surg Br. 2004;86:1187–91. doi: 10.1302/0301-620X.86B8.15228. [DOI] [PubMed] [Google Scholar]
- 22.Samuelson EM, Cordero GX, Fehringer EV. Fracture of a reverse total shoulder arthroplasty retentive liner. Orthopedics. 2009;32:211. [PubMed] [Google Scholar]
- 23.Sayana MK, Kakarala G, Bandi S, Wynn-Jones C. Medium term results of reverse total shoulder replacement in patients with rotator cuff arthropathy. Ir J Med Sci. 2009;178:147–50. doi: 10.1007/s11845-008-0262-8. [DOI] [PubMed] [Google Scholar]
- 24.Seebauer L, Walter W, Keyl W. Reverse total shoulder arthroplasty for the treatment of defect arthropathy. Oper Orthop Traumatol. 2005;17:1–24. doi: 10.1007/s00064-005-1119-1. [DOI] [PubMed] [Google Scholar]
- 25.Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007;89:588–600. doi: 10.2106/JBJS.F.00226. [DOI] [PubMed] [Google Scholar]
- 26.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388–95. doi: 10.1302/0301-620X.86B3.14024. [DOI] [PubMed] [Google Scholar]
- 27.Terrier A, Merlini F, Pioletti DP, Farron A. Comparison of polyethylene wear in anatomical and reversed shoulder prostheses. J Bone Joint Surg Br. 2009;91:977–82. doi: 10.1302/0301-620X.91B7.21999. [DOI] [PubMed] [Google Scholar]
- 28.Tower SS, Currier JH, Currier BH, Lyford KA, Van Citters DW, Mayor MB. Rim cracking of the cross-linked longevity polyethylene acetabular liner after total hip arthroplasty. J Bone Joint Surg Am. 2007;89:2212–7. doi: 10.2106/JBJS.F.00758. [DOI] [PubMed] [Google Scholar]
- 29.Valenti P, Boutens D, Nerot C. Delta 3 reversed prosthesis for osteoarthrits with massive rotator cuff tear: long term results (> 5 years). 2000 Shoulders Prostheses. In: Walch G, editor. Two to Ten years Follow-Up. Sauramps Medical; Montpellier: 2001. pp. 253–59. [Google Scholar]
- 30.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–86. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]
- 31.Wierks C, Skolasky RL, Ji JH, McFarland EG. Reverse total shoulder replacement: intraoperative and early postoperative complications. Clin Orthop Relat Res. 2009;467:225–34. doi: 10.1007/s11999-008-0406-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


