Abstract
A few reports have shown that cardiac valve repair may improve central sleep apnea (CSA) in patients with valvular heart disease. It has been suggested that such improvements are associated with the improvement of cardiac function. We report the case of a 67-year-old man with mitral regurgitation, whose CSA converted to predominant obstructive sleep apnea following mitral valvuloplasty in association with a shortening of lung-to-finger circulation time.
Citation:
Takahashi M; Kasai T; Dohi T; Maeno K; Kasagi S; Kawana F; Ishiwata S; Narui K. Conversion from predominant central sleep apnea to obstructive sleep apnea following valvuloplasty in a patient with mitral regurgitation. J Clin Sleep Med 2011;7(5):523-525.
Keywords: Sleep apnea, mitral regurgitation, valvuloplasty
It has been reported that in heart failure (HF) patients, central sleep apnea (CSA) may be improved by the initiation of specific therapy for HF.1,2 Similarly, several reports have suggested that valve repair may improve CSA in patients with valvular heart disease.3,4 Here we describe a case involving a patient with severe mitral regurgitation (MR), who after valvuloplasty converted from a predominantly central to a predominantly obstructive sleep apnea (OSA) phenotype.
REPORT OF CASE
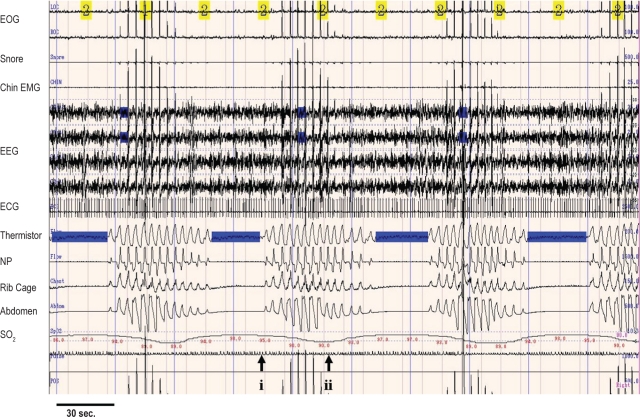
A 67-year-old man with atrial fibrillation and severe MR was diagnosed as having severe CSA in association with a prolonged lung-to-finger circulation time (LFCT) (Figure 1A). He also had moderate-to-severe tricuspid regurgitation (TR) and a markedly dilated left atrium (LA), with preserved left ventricular ejection fraction (LVEF) (73%). The patient's plasma brain natriuretic peptide (BNP) level was 473 pg/mL, and he had New York Heart Association (NYHA) class II symptoms and moderate-to-severe bilateral leg edema.
Figure 1A.
Comparison between before and after before mitral valvuloplasty
Diagnostic sleep study: Note 4 central apneas and subsequent waxing and waning hyperventilation. During central apneas, movements of the ribcage and abdomen are absent. Duration from the onset of the first breath terminating the apnea (i) to the nadir of the subsequent dip in SpO2 measured at the finger (ii) indicates the lung-to-finger circulation time, which is considerably long (average of 10 consecutive apnea-hyperpnea cycles during the first episode of stage 2 sleep, 30 sec). Total AHI in this study was 36.3/h (central AHI, 34.4/h and obstructive AHI, 1.9/h), and distributions of slow wave sleep and REM sleep were 6.0% and 19.2% of total sleep time, respectively. EOG, electroculogram; EMG, submental electromyogram; EEG, electroencephalogram; NP, nasal pressure; SpO2, oxyhemoglobin saturation; AHI, apnea-hypopnea index.
Before surgery for MR, continuous positive airway pressure (CPAP) therapy was initiated for treatment of CSA. Although CPAP provided only slight improvement in AHI (32.9/h) and no improvement of MR, it did slightly alleviate the patient's daytime tiredness, so he continued to use CPAP. A mitral valvuloplasty was later performed to alleviate worsening HF symptoms.
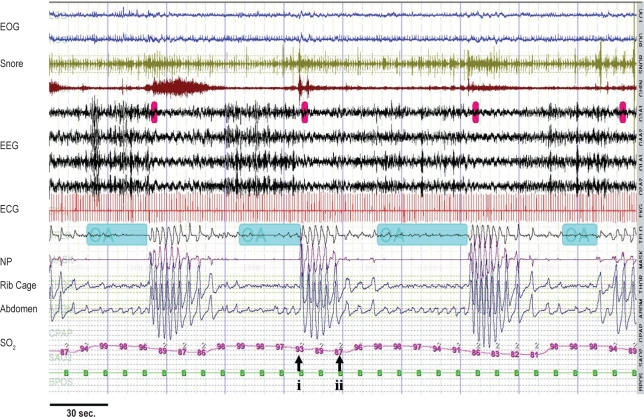
After mitral valvuloplasty combined with Maze procedure and tricuspid annuloplasty, reductions of NYHA class (class I) and body weight (−3 kg) were observed in association with corrections of MR and TR accompanied by marked reductions in LA dimension and plasma BNP (66.9 pg/mL) and conversion to sinus rhythm. However, he still had mild bilateral leg edema and severe sleep disordered breathing (SDB), but his CSA had converted to predominant OSA in association with shorter LFCT (Figure 1B). Additionally, his OSA responded well to CPAP (AHI, 5.7/h on CPAP)
Figure 1B.
Comparison between before and after before mitral valvuloplasty
Reassessment sleep study following mitral valvuloplasty: Note 3 obstructive apneas. During obstructive apneas, out-of-phase movements of the ribcage and abdomen are observed. Duration from the onset of the first breath terminating the apnea (i) to the nadir of the subsequent dip in SpO2 measured at the finger (ii) indicates the lung-to-finger circulation time, which is shorter than that before surgery (average of 10 consecutive apnea-hyperpnea cycles during the first episode of stage 2 sleep, 15 sec). Total AHI in this study was 49.8/h (central AHI, 4.1/h and obstructive AHI, 44.7/h), and distributions of slow wave sleep and REM sleep were 0% and 6.3% of total sleep time, respectively. EOG, electroculogram; EMG, submental electromyogram; EEG, electroencephalogram; NP, nasal pressure; SpO2, oxyhemoglobin saturation; AHI, apnea-hypopnea index.
DISCUSSION
Yasuma and colleagues have reported that the frequency of SDB diminished with the resolution of periodic breathing following mitral valve repair in a patient with severe MR.3 However, in their report, there were no specific descriptions regarding a shift in the type of SDB. Rubin and colleagues showed complete elimination of CSA by mitral valvuloplasty in association with a shortening of circulation time, signifying an improvement in cardiac output.4 The findings of our case are consistent with these reports. However, our case showed no improvements in total AHI; rather increases in obstructive events were observed, despite a marked improvement in central events.
There are several possible mechanisms that may explain such a shift from CSA to predominantly OSA. An increase in the sleeping time while supine or during REM sleep may be an explanation; however, neither sleeping time while supine nor during REM sleep increased in our case. A report from the recent clinical trial demonstrated a spontaneous conversion from predominantly CSA to OSA in 18% of a control group in association with a LVEF improvement.5 Another study showed that improvement in cardiac function following cardiac transplantation in HF patients was accompanied by complete resolution of CSA or conversion to predominantly OSA.2 The observations from both these reports, as well as our case, raise the possibility that, in patients with cardiac dysfunction, OSA and CSA may be part of the spectrum of periodic breathing, the predominant type of which can transform over time in response to alterations in cardiac function. The mechanisms involved in this transformation may include alteration of ventilatory drive, which is elevated in association with pulmonary congestion and increased chemosensitivity. With the improvement in cardiac dysfunction, these inciting factors may be relieved, leading to a shortened circulation time and alleviation of CSA. The patient in our report may have previously had an obstructive respiratory physiology that was masked by the effects of elevated ventilatory drive, the amelioration of which unmasked the obstructive phenotype. However, we do not have any data about chemosensitivity or any information regarding his prior SDB. These are limitations of our report. Alteration of volume status and rostral fluid redistribution over the night in relation to the improvement in cardiac function may take part in these mechanisms,6 although these were not specifically evaluated in our case. Changes in medication may also contribute to such a shift of SDB phenotype. Nevertheless, such shifts alter the responsiveness to the therapy for SDB. In our case, we tried CPAP before surgery; however, it failed to alleviate the CSA. After surgery, the OSA of our case was easily treated by CPAP.
Although the underlying mechanisms remain unclear, the present report highlights the existence of a relationship between the alteration of cardiac function and conversion in type of SDB in a patient with severe MR.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Tamura A, Kawano Y, Naono S, Kotoku M, Kadota J, et al. Relationship between beta-blocker treatment and the severity of central sleep apnea in chronic heart failure. Chest. 2007;131:130–5. doi: 10.1378/chest.06-0919. [DOI] [PubMed] [Google Scholar]
- 2.Mansfield DR, Solin P, Roebuck T, Bergin P, Kaye DM, Naughton MT, et al. The effect of successful heart transplant treatment of heart failure on central sleep apnea. Chest. 2003;124:1675–81. doi: 10.1378/chest.124.5.1675. [DOI] [PubMed] [Google Scholar]
- 3.Yasuma F, Hayashi H, Noda S, Tsuzuki M, Tanaka M, Okada T, et al. A case of mitral regurgitation whose nocturnal periodic breathing was improved after mitral valve replacement. Jpn Heart J. 1995;36:267–72. doi: 10.1536/ihj.36.267. [DOI] [PubMed] [Google Scholar]
- 4.Rubin AE, Gottlieb SH, Gold AR, Schwartz AR, Smith PL, et al. Elimination of central sleep apnoea by mitral valvuloplasty: the role of feedback delay in periodic breathing. Thorax. 2004;59:174–6. doi: 10.1136/thorax.2003.007799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ryan CM, Floras JS, Logan AG, et al. Shift in sleep apnoea type in heart failure patients in the CANPAP trial. Eur Respir J. 2010;35:592–7. doi: 10.1183/09031936.00070509. [DOI] [PubMed] [Google Scholar]
- 6.Yumino D, Redolfi S, Ruttanaumpawan P, et al. Nocturnal rostral fluid shift: a unifying concept for the pathogenesis of obstructive and central sleep apnea in men with heart failure. Circulation. 2010;121:1598–605. doi: 10.1161/CIRCULATIONAHA.109.902452. [DOI] [PubMed] [Google Scholar]