Abstract
Objective:
This pilot study explored whether learning style–tailored education materials, “information prescriptions,” are effective in increasing hypertension knowledge in emergency room patients.
Methods:
In a randomized trial, hypertensive emergency medicine patients received either standard care discharge instructions or discharge instructions in combination with an information prescription individualized to each patient's learning-style preference. Two weeks post-visit, the study team assessed changes in hypertension knowledge via a survey.
Results:
No significant difference was observed for changes in quiz scores on the hypertension knowledge assessment, though patients receiving the tailored information prescriptions reported higher levels of satisfaction with intervention materials.
Conclusion:
The study demonstrated the workflow feasibility of implementing a learning-style approach to patient education in the emergency department setting. Further research is needed to develop more robust measures of high blood pressure knowledge among the emergency department patient population. This work will contribute to establishing a framework for developing customized information prescriptions that can be broadly adapted for use in varied settings and with varied health care conditions.
Highlights.
The effect of an information prescription tailored to a patient's learning-style preference may depend on level of education and information-seeking behaviors.
Measuring patient awareness of issues related to high blood pressure requires the use of robust instruments that can adequately capture variations in knowledge.
The emergency department workflow can accommodate the implementation of a tailored information prescription strategy for providing educational patient information.
Implications.
This pilot study provides a framework for developing customized information prescriptions that can be broadly adapted for use across various health care settings and health care conditions.
Future information prescription studies can leverage this approach and further refine implementation details and outcome measures.
INTRODUCTION
Hypertension poses a significant public health burden in the United States despite being a modifiable risk factor for cardiovascular health outcomes. Affecting nearly 31% of the population over 20 years of age, high blood pressure increases risk of neurovascular, cardiovascular, and renal disease [1–4]. Diagnosing and managing hypertension is particularly challenging because as many as 25% of patients with high blood pressure are unaware that they have the condition [1]. Of those who know they have hypertension, only 65% are being treated with antihypertensive medications [5]. Racial disparities in disease prevalence rates further contribute to the public health challenge of hypertension. African Americans and individuals living below the poverty level have the highest rates of high blood pressure and are more likely to develop the condition and acquire it at earlier ages [1, 3].
Hypertension and its sequelae, whether as primary complaints or secondary findings, represent significant challenges in the emergency department (ED). Approximately 25% of emergency room patients have hypertension [6], and those groups at highest risk are also disproportionately represented in national ED utilization estimates [6, 7]. Elevated blood pressure in the ED may predict chronic hypertensive disease status [8–10], yet little literature addresses long-term success in managing these patients once they are discharged from the ED.
Lifestyle modification plays a large role in reducing negative outcomes among hypertensive patients, and knowledge is a critical factor to informed patient decision making [4]. Unfortunately, the often chaotic ED environment poses patient-provider communication challenges that affect information delivery and patient comprehension. Up to 78% of ED patients do not understand information provided to them in the ED setting, thus resulting in a decrease in their ability to properly seek care and adhere to care recommendations [11–13]. The development and provision of educational material specifically tailored to each patient may provide a promising mechanism for information delivery.
In 1998, with seed money received from the Vanderbilt Medical Group, the Eskind Biomedical Library (EBL) implemented the Patient Informatics Consult Service, which provides targeted information to patients and their families [14]. Applying an information prescription model, the service utilizes prescription pads (analogous to medication prescription pads), which allow clinicians to prescribe medical information to patients. Patients who are prescribed health information receive materials selected specifically for their care based on accuracy, authority, and currency criteria. To close the communication loop, the patient's health care provider also receives the compiled packet. The EBL team's long-standing experience in patient education has provided a clear understanding of health literacy issues that affect consumer interpretation of health information. A key insight has been the recognition that adapting information to patients' learning styles may play an important role in acquiring health literacy.
The relationship between individual learning preferences and their influence on patient health communication is minimally explored in the biomedical literature. The objective of this pilot study was to investigate whether learning style–tailored information prescriptions can increase ED patients' knowledge of issues related to hypertension. Results from this work will inform the team's future research efforts to investigate the impact of tailored education materials.
METHODS
Population
Emergency medicine patients aged eighteen or older, able to speak and read English, and able to provide telephone contact information were eligible for the study. In addition, eligible patients were to have two or more blood pressure measurements during the ED visit that met criteria for stage I or stage II hypertension with thresholds determined by the Joint National Committee on Prevention, Detection, and Evaluation and Treatment of High Blood Pressure [15]. The prospective collection of blood pressure measurements aids the ED in identifying asymptomatic high blood pressure patients and provides a larger patient recruitment pool than relying solely on data gleaned from the medical chart on the patient's hypertensive status. Patients were not eligible for the study if they exhibited any of the following exclusion criteria: (1) had an emergency severity index of 1, (2) were currently imprisoned, (3) showed evidence of cognitive impairment, (4) presented a psychiatric chief complaint, (5) left the ED without being seen by a physician, (6) left the ED against medical advice, or (7) were enrolled in the study during a previous ED encounter.
The study was conducted in the Vanderbilt University Medical Center ED, a level 1 trauma center with more than 56,000 patient visits each year. All recruitment activities and patient interactions were conducted by knowledge management information specialists trained in human subjects research. Three information specialists, working in rotating teams of two, daily reviewed the institution's electronic medical record system, the electronic triage and patient tracking application, and information obtained from ED clinical staff to determine patient eligibility. After confirming eligibility, information specialists approached patients to obtain informed consent. Telephone surveys were conducted two weeks after each patient's ED visit to obtain follow-up data. The study was approved by the Vanderbilt University Institutional Review Board.
Baseline assessment
After determining study eligibility and informed consent, the study team of information specialists collected baseline data on all participants. Current and historical medical information about the ED visit and each patient's hypertensive status was collected from the electronic medical record and from a short questionnaire. Demographic information collected included age, gender, race or ethnicity, highest level of education completed, insurance status, employment status, individual and family past medical history of hypertension, high blood pressure medications, smoking status, comorbidities, chief complaint, and pain score on a one-to-ten visual analog scale.
Each study participant also completed two additional assessments at baseline: hypertension knowledge and learning-style questionnaires. To assess hypertension knowledge, participants completed the “Check Your High Blood Pressure IQ” quiz developed by the National Heart, Lung, and Blood Institute (NHLBI) [16], a 12-item true/false response option quiz. Each question received an equal point value, and answers were scored on a 0–100 scale, based on the percentage of questions answered correctly. To assess individual learning preferences, patients completed the Visual, Aural, Read/Write, Kinesthetic (VARK) questionnaire, a 16-item multiple-choice survey [17]. Questionnaires were either completed by the patient or recorded by the information specialists when patients were incapacitated by medical devices (e.g., intravenous lines in hands and/or arms). When patients needed clarification regarding the instrument questions, information specialists reiterated the questions and instructions to study participants and directed the patients to select the most appropriate answers based on their personal experience and opinions. The study team's interactions were conducted during participants' waiting times during their ED stay. The intervention did not add to the overall ED visit length.
Randomization
Following baseline assessment, participants were randomized into two groups: (a) to receive standard care discharge instructions (printed instruction sheet) or (b) to receive discharge instructions and an information prescription tailored to their specific learning-style preferences. Randomization was conducted using a permuted block design with random block sizes of 2, 4, and 6. Randomization sequences were manually generated by one of the study authors (Koonce) using a random numbers table; placed in consecutively numbered, sealed, opaque envelopes; and opened after obtaining each patient's consent to participate in the study.
Intervention
Standard care
Following baseline assessment, participants randomized to the standard care group received regular discharge instructions from ED clinical staff at the completion of their visits. Discharge instructions were typically one to two pages of text providing patients with details on how to follow up on care regarding the ED diagnosis, as well as reasons to return to the ED. The discharge instructions often contained a short section with educational information concerning each patient's diagnosis in addition to specific follow-up care instructions. Information on high blood pressure is included in the discharge materials when it is the primary reason for the ED visit.
Information prescription
The study team of information specialists provided the intervention group with an information prescription tailored to the patient's individual learning style. The customization of content to specifically match a patient's learning style represents an evolution of the Patient Informatics Consult Service model. Learning objectives for the information prescription content were created that were consistent with facets covered in the NHLBI hypertension quiz (e.g., diagnosis, risk factors, and prevention and treatment principles). Content was selected via review of existing hypertension education materials from government agencies and national associations, with selection based on aspects of currency, authority, and accuracy in alignment with established guidelines [18, 19]. All print materials for each information prescription were designed to target an eighth-grade reading level.
Each patient's baseline score on the VARK questionnaire was used to inform the format of the information prescription received. The VARK questionnaire results categorize individuals into one of several preferred learning modalities: visual, read/write, aural, and kinesthetic learners. Individuals with preferences for visual learning modalities favor information depicted via pictures, charts, graphs, diagrams, and so on. Read/write learners place emphasis on words and ideally benefit from the use of lists, bullets, and text presented in hierarchies. Aural learners' primary inputs come from what others say; written words have less importance than information communicated verbally. Kinesthetic learners benefit from doing and trying things for themselves, especially via concrete experiences [17]. The study team leveraged the VARK developers' recommendations for formats that best match each learning-modality preference to guide the formation of each information prescription. Four different formats were used for the study intervention with each designed to match a patient's learning-style preference.
Visual learners: The study team developed three printed handouts for visual learners, one handout each to provide overview information on hypertension, explanation of risk factors, and prevention and treatment options with emphasis on lifestyle modifications. Content for the handouts was largely drawn from materials in the NHLBI's National High Blood Pressure Education Program [20]. Each handout incorporated a variety of graphic images to enhance the text. To ensure that each individual understood what was being provided, information specialists spent approximately five minutes reviewing content on the handouts with each visual learner patient in the intervention group.
Read/write learners: Patients with read/write learning preferences were also provided three printed handouts, each covering the same content provided for visual learners. The materials for patients with read/write preferences emphasized the printed word and used strategies such as bolded headers, bulleted lists, and color coding to communicate specifics of hypertension diagnosis, risk, and prevention and treatment. The review of this content with each read/write learner in the intervention group also took approximately five minutes.
Aural learners: To optimize information delivery for those in the intervention group with aural learning preferences, the study team provided a modified version of a hypertension mp3 file podcast created by the NHLBI [21]. The original thirty-three-minute-long podcast was abbreviated to seven minutes by the study team using freely available audio file–manipulation software [22]. Cross-referencing the podcast transcript with the information on each printed handout allowed the team to match details about hypertension across formats for consistency. The abbreviated podcast presented overview information on hypertension, discussed risk factors, and covered prevention and treatment principles with a particular focus on lifestyle modifications. Patients randomized to the intervention group with aural learning preferences listened to the podcast on a study team–provided laptop. Study team personnel remained present, depending on patient preference. Afterward, they received a copy of the podcast on CD to take home.
Kinesthetic learners: Strategies to promote active participant engagement are ideal for kinesthetic learners. The information prescription for these study participants consisted of an interactive, web-based application from the American Heart Association, “High Blood Pressure Health Risk Calculator” [23]. Using established guidelines in combination with patient-entered data (e.g., blood pressure measurements) that were consistent with other information prescription formats, the module presents overview information on high blood pressure, details the individual's specific health risks for high blood pressure, and describes the effects of lifestyle changes. The module took approximately fifteen minutes to complete and was conducted by each patient using a study team–provided laptop. Afterward, they received a handout with the uniform resource locator (URL) of the online module to take home.
Multimodal learners
In addition to the four learning modalities, the VARK also accounts for respondents who may be deemed multimodal learners. For purposes of the pilot study, when a patient's response resulted in a multimodal categorization, study information professionals requested that the patient select a single preferential mode for the study intervention.
Follow up and outcome assessment
The primary outcome variable for the study was difference in hypertension knowledge scores between the 2 groups 2 weeks after the ED visit. Two weeks post-discharge, study participants were contacted via telephone to retake the NHLBI hypertension quiz. Questions were asked in a randomly selected order that differed from the first administration to reduce the likelihood of a test practice effect. All telephone interviews were conducted by the same study team member using a predetermined script. In addition to the NHBLI quiz, each patient also completed a set of internally developed questions to measure understanding of and satisfaction with provided materials. Patients were asked to indicate their level of agreement or disagreement with 6 statements using response options on a 1–5 Likert scale. After completing the study, each participant received a $20 gift card to a local grocery store.
Statistical analysis
Sample size for the study was planned to detect a minimum 10% mean difference in the primary outcome of hypertension knowledge score between the 2 groups and calculated to establish a margin of error with 0.95 confidence, given that no previously available standard deviation data were available for the NHLBI questionnaire. DuPont's PS: Power and Sample Size Calculation software was used to determine a minimum sample size of 25 patients in each arm, based on the narrow margin of error parameters [24]. To allow for a planned high drop-out rate, study enrollment was targeted to include 38 patients per arm.
Baseline characteristics of the intervention and control groups were analyzed for imbalance using chi-square tests for categorical data and 2-sample t tests for continuous data. The primary outcome measure of the difference in hypertension knowledge quiz scores between the 2 groups was analyzed using the 2-sample t test. Statistical analysis was conducted with Small Stata 11.0. Descriptive statistics were used to characterize all data observations other than the primary outcome variable.
RESULTS
Study participants
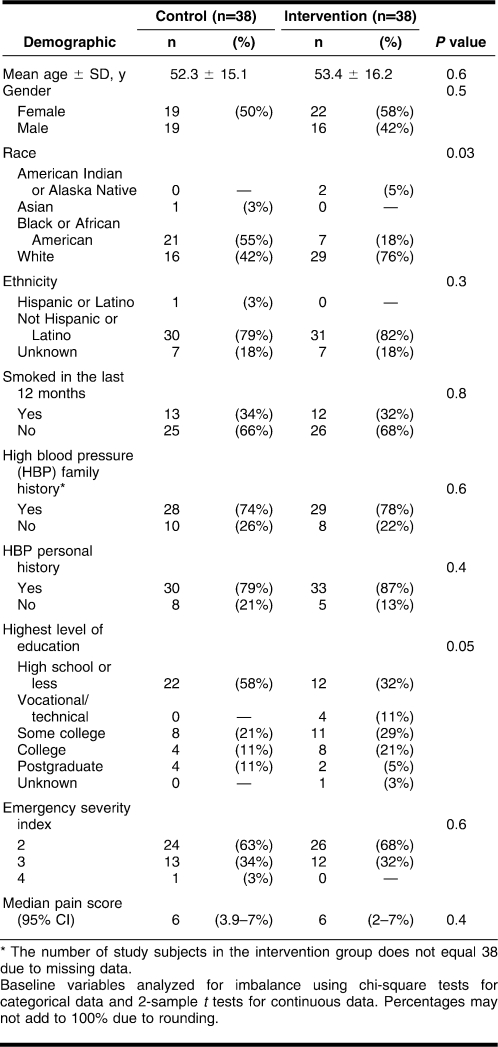
A total of 185 patients were initially identified for study inclusion (Figure 1). Of these, 109 patients were excluded for not meeting all inclusion criteria (n = 36), refusal to participate (n = 38), and other reasons, such as being discharged before the study team had an opportunity to approach the patient and being out of the ED for tests (n = 35). After patient exclusions, 76 patients were randomized to either the control or intervention groups. Seven patients in each arm were unable to be reached for follow up despite multiple contact attempts. Primary outcome data were collected for 31 patients in each study group. All patients were recruited from November 17, 2009–December 10, 2009. Follow-up telephone calls to patients were conducted between December 1, 2009, and December 29, 2009, with a median of follow up at 15 days post-discharge from the ED.
Figure 1.
Participant flow chart
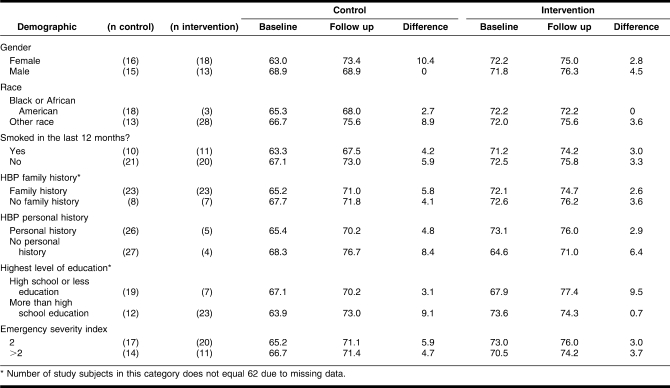
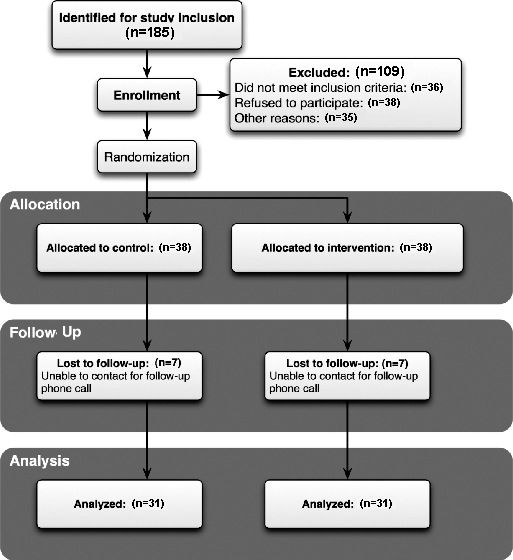
The demographic characteristics of the study participants are summarized in Table 1. Patients in each study group were similar in age, gender, ethnicity, median pain scores, and emergency severity index values. There were no differences between groups in self-reported individual and family history of hypertension. Both groups reported similar rates of smoking status over the previous 12 months, though the overall prevalence of smoking in the study population was 33%, slightly higher than the general 20% nationwide smoking prevalence rates. An imbalance in the proportion of African American study participants was observed between groups: 55% (n = 21) of the patients in the control group were African American, compared to 18% (n = 7) in the intervention group. Highest reported level of education was also unbalanced among groups in 1 category: high school education or less (58% (n = 22) in the control group vs. 32% (n = 12) in the intervention group). Only one patient visited the ED due to a chief complaint related to hypertension.
Table 1.
Patient demographics
Learning style distribution
The distribution of learning styles among the pilot study's patient population largely paralleled learning-style distributions among the general population (Figure 2, online only). Percentages of visual, read/write, and kinesthetic learners were most similar to the general population of 50,000 respondents for the online VARK questionnaire [17]. The percentage of aural learners among study participants was more than double the general population (18.0% vs. 7.2%), while the percentage of multimodal learners was lower than the general population (45.0% vs. 59.6%).
Figure 2.
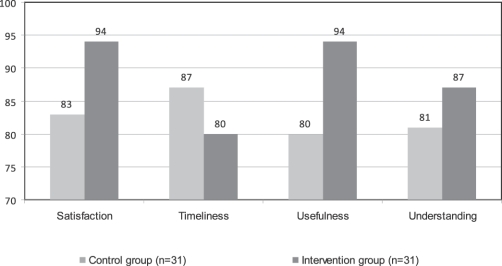
Patient feedback as study follow up*
* Proportion of respondents answering “Agree” or “Strongly agree” (4 or 5 respectively) on a 1–5 Likert scale.
Hypertension knowledge differences
Hypertension knowledge scores two weeks post-ED-discharge did not differ between the control and intervention groups. The difference in mean knowledge score in the control group was 5.3 versus 3.3 in the intervention group (P = 0.5, 95% confidence interval −4.2–8.5). Mean baseline hypertension knowledge scores were higher in the intervention group (72.0, SD = 10.9) than the control group (65.9, SD = 9.0), and mean follow-up scores for the intervention group (75.3, SD = 9.0) were higher than mean baseline scores in the control group (71.2, SD = 11.1).
The sample size calculation for this pilot study was powered to detect significant differences in the primary outcome variable only. Thus, descriptive statistics, rather than tests of statistical significance, were used to explore additional outcomes. These statistics revealed that among those patients reporting their highest level of education as high school or less, the difference in mean knowledge scores between baseline and follow up for the control group (Table 2) was 6.4 points lower than the difference in mean knowledge scores for the intervention group (3.1 vs. 9.5). The opposite trend was observed for those with more than high school education (9.1 vs. 0.7). Differences related to gender were also observed (Table 2). For male study participants, the difference in mean hypertension knowledge scores at follow up was 4.5 points higher in the intervention group than the control group (0 vs. 4.5). Contrasting results were observed in female study participants, with females in the control group demonstrating an increase in knowledge scores 8.1 points higher at follow up than the intervention group (10.4 vs. 2.3).
Table 2.
High blood pressure quiz score outcomes by demographic variables (n = 62)
Analysis of questions asked on the hypertension quiz at baseline data collection (Table 3, online only) showed that 5 of the 12 questions were frequently answered correctly by the 76 study participants, and 7 were answered correctly at baseline by over 80% of the participants. The statement “High blood pressure has no cure,” showed the greatest increase in quiz scores post-intervention. Among those who completed the follow-up quiz, 10 control group participants answered correctly during final data collection, up from 7 at baseline, and in the intervention group, 16 participants answered correctly 2 weeks post-visit, up from 6 at baseline. The statement, “Stress causes high blood pressure,” showed a decrease in the number of participants answering correctly from baseline to follow up (5 vs. 1, respectively).
Participant feedback
During the follow-up survey, additional data were collected from each study participant to assess the impact of the information prescription on their understanding of and satisfaction with provided materials. Figure 3 summarizes the proportions of respondents answering “Agree” or “Strongly agree” to each of the statements associated with 4 impact areas: satisfaction, timeliness of information provision, usefulness, and ability of the information to increase understanding. Participants who received the intervention materials reported satisfaction agreement 94% (29/31) of the time compared to 84% (26/31) for the control group receiving standard care discharge instructions alone. More participants in the intervention group (87%, n = 27) than the control group (84%, n = 26) answered “Agree” or “Strongly agree,” when asked to rate their level of agreement that the received information was easy to understand.
All patients were asked to indicate the extent to which provided recommendations were being followed. Eighty percent of the control group participants answered “Agree” or “Strongly agree,” when asked if they were following the recommendations in the ED discharge materials; 58% of participants in the intervention group reported “Agree” or “Strongly agree,” when asked if they were following recommendations provided in the information prescription materials. When asked if the presented information was already known to them, 77% (n = 24) of control group members answered “Agree” or “Strongly agree” for the ED discharge information received and 61% (n = 19) of intervention group members answered the same for the received information prescription materials. Intervention group patients who answered “Agree” or “Strongly agree” that the information was already known to them had lower improvement in quiz scores at follow up than did patients who did not agree or strongly agree (3.1 vs. 3.5 point increase).
DISCUSSION
This pilot study allowed the research team to investigate the conceptual feasibility of a learning style–tailored information prescription. While prior hypertension educational intervention studies have focused largely on adapting materials to health literacy levels, few studies have incorporated learning-style preferences into health communication practices. In a survey of ninety-nine caregivers of asthmatic children, Dinakar et al. utilized the VARK questionnaire to characterize learning preferences to inform education activities [25]. Boyde et al. used the VARK to assess learning preferences of heart failure patients and provide recommendations for educational needs [26]. Carbone et al. piloted the use of tailored diabetes education activities, customized to individual literacy levels and learning styles, with ten Spanish-speaking adult patients with type-2 diabetes. Investigators used results from cognitive interviews to ascertain which learning activities were easiest or most difficult for study participants. Specific behavioral and clinical outcomes were not measured; however, their results contributed preliminary understanding of how this approach can inform patient education [27].
In the current study, results do not indicate a significant change between the intervention and control groups in knowledge of hypertension issues two weeks post-ED-visit, but descriptive analysis of patient subgroups provides useful indicators for which patients might best benefit from this customized learning approach. While a larger sample would be required for a definitive conclusion, the personalized information prescription content appears to have improved hypertension knowledge for persons with a high school education or less. This is not surprising as lower educational status, often a marker for lower socioeconomic status, is associated with increased hypertension prevalence rates and may signal a patient population with greater information needs [28, 29]. Additionally, the data suggest that the intervention had a greater effect on men than women. This might result from different information-seeking behaviors between the two groups. Anecdotal patient feedback and quiz results suggest that female participants in the control group might have researched hypertension information on their own prior to completing the follow-up survey. These results are in keeping with published research indicating women have higher rates of information-seeking behavior [30, 31]. A larger sample, which would permit a multiple regression analysis, would be useful to shed further light on potential interactions between these demographic variables and knowledge outcome scores. While not specified in the a priori statistical analysis plan, this technique may be employed in future studies using this intervention.
Mean baseline hypertension knowledge scores were high in both arms of the study, leaving little room for increase in scores at follow up. An analysis of responses on the hypertension quiz revealed that study participants knew the correct answers to many of the questions at baseline: Only three of the questions were answered incorrectly a majority of the time by both control and intervention participants. This finding can inform the future development of weighted scoring algorithms for calculating hypertension knowledge scores.
Response item analysis also sheds light on an additional component of the study process. Interestingly, quiz results for the statement regarding stress as a cause of high blood pressure showed a decrease in the number of correct responses among patients in the intervention group at follow up. NHLBI education materials given to patients discussed long-term stress as a contributor to high blood pressure, whereas the official NHLBI answer to the question, “Stress causes high blood pressure” (true/false), is “False.” The question posed to study participants did not make a distinction between short- versus long-term stress, thus it is understandable that patients would perceive stress as not only a contributor to but as a cause of high blood pressure. This perhaps explains the direction of the scores on this quiz item. In contrast, scores on the quiz item with the second-lowest baseline score, “High blood pressure has no cure,” showed the greatest improvement at follow up, thus creating optimism for improving hypertension knowledge. A future study design that will not only utilize a weighted scoring methodology to allow more importance for specific questions, but also include questions with increased complexity to provide more room for improvement in baseline scores.
Hypertension was previously diagnosed in 87% (27/31) of the intervention group members who completed the follow-up survey. At follow up, 61% (19/31) of these patients reported already knowing the information contained in the intervention materials. The gap between patients diagnosed with hypertension (n = 27) and the number reporting prior knowledge of the provided hypertension information (n = 19) further supports the need for increased patient education.
Limitations
Results from the item response analysis of the hypertension quiz suggest limitations in its ability to satisfactorily discriminate potential knowledge differences, because nine of twelve questions were answered correctly a majority of the time. Further research to develop a validated hypertension knowledge measurement instrument for the ED setting could potentially provide greater accuracy in determining knowledge changes.
Primary outcome results in hypertension knowledge scores differed by gender, with women in the control group demonstrating higher scores two weeks post visit than men. The follow-up interview did not include a question designed to ascertain information-seeking practices of participants, and therefore the study team was not able to directly compare self-reported behaviors against knowledge score outcomes. Modifications of the post-ED-visit survey to include this question will allow the team to independently assess the effect of external inquiring or searching behavior on follow-up outcomes.
Patients receiving intervention materials reported higher levels of satisfaction than those receiving standard discharge instructions. The higher scores may possibly be confounded by the method of delivery rather than the information itself, because control group participants received information in a more routine manner than the intervention group. However, since health communication exchanges between providers and patients can undoubtedly benefit from more personalized approaches, the intervention might positively affect patient perceptions of their overall health care team.
In this pilot study, the team provided the intervention via one learning mode, yet patients can exhibit multimodal learning preferences. Future efforts to use information delivery formats encompassing multimodal learning styles (e.g., combining kinesthetic with aural preferences or read/write with visual preferences) is likely to provide greater patient benefit. Additionally, an individual's ability to learn and act upon new information is undoubtedly influenced by a variety of factors other than specific learning-style preferences. However, addressing learning-style preferences eliminates one potential barrier in health communication practices.
CONCLUSION
With this investigation, the study team explored how to best provide health education materials to ED patients with high blood pressure. Overall, patients who received the learning style–tailored information were satisfied, perceived that the materials increased their understanding, and found them useful. The study's negative findings on knowledge outcomes may be especially attributable to high knowledge scores at baseline, and further research is needed to develop questionnaires that can adequately capture patients' understanding of high blood pressure concepts and management issues.
Practice implications
Using different learning styles could provide initial steps in establishing a framework for developing customized information prescriptions that can be broadly adapted for use across varied health care settings and with varied health care conditions. Informatics approaches may provide further opportunities to streamline and enhance delivery of information prescriptions in the clinical setting. Increasing patient awareness and knowledge via this customized strategy supports informed decision making and may ultimately translate to increased positive self-management behaviors and improved clinical outcomes. Further work may help to define best practices for the delivery and implementation of this model.
Electronic Content
Study participants Visual, Aural, Read/Write, Kinesthetic (VARK) learning style distributions*
Baseline item response analysis of the “Check Your High Blood Pressure IQ” quiz
Acknowledgments
The authors thank Karen Miller for coordinating activities in the Vanderbilt University Emergency Medicine Department; Sandra Martin, Jennifer Lyon, AHIP, and Pauline Alexander for their contributions to recruiting and interviewing patients in the emergency medicine department; Kelli Koonce for her assistance with data collection and database administration; and Patrick Arbogast and Lisa Kaltenbach for guidance with statistical analysis.
Footnotes
Supported by funding from the National Library of Medicine (National Institutes of Health [NIH] grant no. T15 LM007450-06). The REDCap database used for data collection is supported by funding from the National Center for Research Resources (NIH grant no. 1 UL1 RR024975).
This article has been approved for the Medical Library Association's Independent Reading Program <http://www.mlanet.org/education/irp/>
REFERENCES
- 1.National health and nutrition examination survey data [Internet] Centers for Disease Control and Prevention, National Center for Health Statistics. The Centers; 2009 [updated 21 Jul 2009; cited 26 Nov 2010]. < http://www.cdc.gov/nchs/nhanes/about_nhanes.htm>.
- 2.Lloyd-Jones D, Adams R.J, Brown T.M, Carnethon M, Dai S, De Simone G, Ferguson T.B, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho P.M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M.M, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger V.L, Rosamond W, Sacco R, Sorlie P, Roger V.L, Thom T, Wasserthiel-Smoller S, Wong N.D, Wylie-Rosett J American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010 Feb 23;121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 3.Yoon S.S, Ostchega Y, Louis T. Recent trends in the prevalence of high blood pressure and its treatment and control, 1999–2008. NCHS Data Brief. 2010 Oct. pp. 1–8. [PubMed]
- 4.Committee on Public Health Priorities to Reduce and Control Hypertension in the U.S. Population. A population-based policy and systems change approach to prevent and control hypertension [Internet] National Academies Press; 2010 [cited 26 Nov 2010]. < http://www.nap.edu/catalog.php?record_id=12819>. [PubMed] [Google Scholar]
- 5.Ong K.L, Cheung B.M. Response to nonpharmacological treatment of hypertension: impact on prevalence estimates. Hypertension. 2007;50:e2. doi: 10.1161/HYPERTENSIONAHA.107.091165. [DOI] [PubMed] [Google Scholar]
- 6.National Center for Health Statistics. Health data interactive [Internet] The Center; 2010 [cited 26 Nov 2010]. < http://www.cdc.gov/nchs/hdi.htm>. [Google Scholar]
- 7.Karras D.J, Kruus L.K, Cienki J.J, Wald M.M, Chiang W.K, Shayne P, Ufberg J.W, Harrigan R.A, Wald D.A, Heilpern K.L. Evaluation and treatment of patients with severely elevated blood pressure in academic emergency departments: a multicenter study. Ann Emerg Med. 2006 Mar;47(3):230–6. doi: 10.1016/j.annemergmed.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Backer H, Decker L, Ackerson L. Reproducibility of increased blood pressure during an emergency department or urgent care visit. Ann Emerg Med. 2003;41:507–12. doi: 10.1067/MEM.2003.151. [DOI] [PubMed] [Google Scholar]
- 9.Tanabe P, Persell S.D, Adams J.G, McCormick J.C, Martinovich Z, Baker D.W. Increased blood pressure in the emergency department: pain, anxiety, or undiagnosed hypertension. Ann Emerg Med. 2008 Mar;51(3):221–9. doi: 10.1016/j.annemergmed.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 10.Decker W.W, Godwin S.A, Hess E.P, Lenamond C.C, Jagoda A.S. Clinical policy: critical issues in the evaluation and management of adult patients with asymptomatic hypertension in the emergency department. Ann Emerg Med. 2006 Mar;47(3):47:237–49. doi: 10.1016/j.annemergmed.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Clarke C, Friedman S.M, Shi K, Arenovich T, Culligan C. Emergency department discharge instructions comprehension and compliance study. CJEM. 2005 Jan;7(1):7:5–11. doi: 10.1017/s1481803500012860. [DOI] [PubMed] [Google Scholar]
- 12.Spandorfer J, Karras D.J, Hughes L.A, Caputo C. Comprehension of discharge instructions by patients in an urban emergency department. Ann Emerg Med. 1995 Jan;25(1):71–4. doi: 10.1016/S0196-0644(95)70358-6. [DOI] [PubMed] [Google Scholar]
- 13.Engel K.G, Heisler M, Smith D.M, Robinson C.H, Forman J.H, Ubel P.A. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand. Ann Emerg Med. 2009 Apr;53(4):454–61. doi: 10.1016/J.ANNEMERGMED.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Williams M.D, Gish K.W, Giuse N.B, Sathe N.A, Carrell D.L. The Patient Informatics Consult Service (PICS): an approach for a patient-centered service. Bull Med Libr Assoc. 2001 Apr;89(2):185–93. [PMC free article] [PubMed] [Google Scholar]
- 15.Chobanian A.V, Bakris G.L, Black H.R, Cushman W.C, Green L.A, Izzo J.L, Jr, Jones D.W, Materson B.J, Oparil S, Wright J.T, Jr, Roccella E.J Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 16.National Heart Lung and Blood Institute. Check your high blood pressure I.Q. Bethesda, MD: US Government Printing Office; 1994. [Google Scholar]
- 17.Fleming N, Mills C. Not another inventory, rather a catalyst for reflection. To Improve Acad Resour Fac Instructional Organ Dev. 1992;11:137–49. [Google Scholar]
- 18.Medical Library Association. A user's guide to finding and evaluating health information on the web [Internet] The Association; 2010 [updated 4 Oct 2010; cited 26 Nov 2010]. < http://www.mlanet.org/resources/userguide.html>. [Google Scholar]
- 19.National Library of Medicine. MedlinePlus: quality guidelines [Internet] The Library [updated 9 Jul 2010; cited 26 Nov 2010]. < http://www.nlm.nih.gov/medlineplus/criteria.html>.
- 20.National Heart Lung and Blood Institute. National high blood pressure education program [Internet] The Institute; 2010 [cited 26 Nov 2010]. < http://www.nhlbi.nih.gov/about/nhbpep/>. [Google Scholar]
- 21.National Heart Lung and Blood Institute. DCI podcasts: high blood pressure [Internet] The Institute; 2010 [cited 26 Nov 2010]. < http://www.nhlbi.nih.gov/health/dci/pods/podcasts.html>. [Google Scholar]
- 22.Audacity. Audacity: free audio editor and recorder, version 1.3.1.1 [Internet] 2010 [cited 26 Nov 2010]. < http://www.audacity.sourceforge.net>.
- 23.American Heart Association. High blood pressure health risk calculator [Internet] The Association; 2010 [cited 26 Nov 2010]. < http://www.americanheart.org/downloadable/heart/flash/size_choice.htm>. [Google Scholar]
- 24.Dupont W, Plummer W.D. PS: power and sample size calculation software (version 3.0.10) [Internet] 2010 [cited 26 Nov 2010]. < http://biostat.mc.vanderbilt.edu/twiki/bin/view/Main/PowerSampleSize>.
- 25.Dinakar C, Adams C, Brimer A, Silva M.D. Learning preferences of caregivers of asthmatic children. J Asthma. 2005 Oct;42(8):683–7. doi: 10.1080/02770900500265157. [DOI] [PubMed] [Google Scholar]
- 26.Boyde M, Tuckett A, Peters R, Thompson D.R, Turner C, Stewart S. Learning style and learning needs of heart failure patients (The Need2Know-HF patient study) Eur J Cardiovasc Nurs. 2009 Dec;8(5):316–22. doi: 10.1016/J.EJCNURSE.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Carbone E, Lennon K, Torres M, Rosal M. Testing the feasibility of an interactive learning styles measure for U.S. Latino adults with type 2 diabetes and low literacy. Int Q Community Health Educ. 2005;25(4):315–35. doi: 10.2190/88J7-1432-2377-55K7. [DOI] [PubMed] [Google Scholar]
- 28.Conen D, Glynn R.J, Ridker P.M, Buring J.E, Albert M.A. Socioeconomic status, blood pressure progression, and incident hypertension in a prospective cohort of female health professionals. Eur Heart J. 2009 Jun;30(11):1378–84. doi: 10.1093/EURHEARTJ/EHP072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Albert M.A, Glynn R.J, Buring J, Ridker P.M. Impact of traditional and novel risk factors on the relationship between socioeconomic status and incident cardiovascular events. Circulation. 2006;114:2619–26. doi: 10.1161/CIRCULATIONAHA.106.660043. [DOI] [PubMed] [Google Scholar]
- 30.Fox S. Health information online [Internet] Pew Internet & American Life Project; 2005 [cited 26 Nov 2010]. < http://www.pewinternet.org/Reports/2005/Health-Information-Online.aspx?r=1>.
- 31.Atkinson N.L, Saperstein S.L, Pleis J. Using the Internet for health-related activities: findings from a national probability sample. J Med Internet Res. 11(1):e4. doi: 10.2196/JMIR.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Study participants Visual, Aural, Read/Write, Kinesthetic (VARK) learning style distributions*
Baseline item response analysis of the “Check Your High Blood Pressure IQ” quiz