Figure 2.
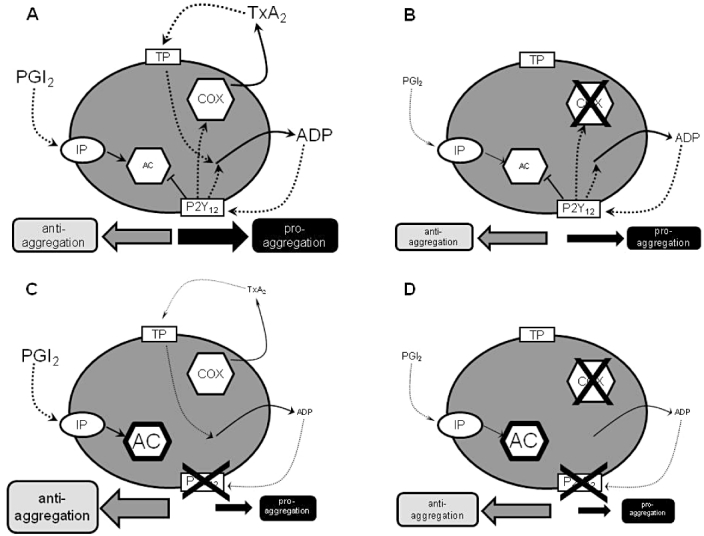
Schematic representation of effects of aspirin and P2Y12-receptor blockers on platelet pathways. (A) In physiological conditions there is balance between anti-aggregatory and pro-aggregatory influences on the platelet from the prostanoid and P2Y12 pathways. PGI2 formed by the blood vessel wall is anti-aggregatory through the stimulation of adenylyl cyclase (AC) secondary to activation of platelet PGI2 receptors (IP receptors). Thromboxane A2 (TXA2) produced by the activity of cyclooxygenase (COX) within the platelet is pro-aggregatory, acting through platelet TXA2 receptors (TP receptors). Activation of TP receptors also promotes the release of ADP from platelets which further drives aggregation. ADP produces its pro-aggregatory effects through activation of platelet ADP receptors (P2Y12 receptors) and inhibition of platelet AC. Activation of P2Y12 receptors drives more production of TXA2 and more release of ADP. (B) In the presence of aspirin, platelet COX is blocked and the TXA2 pathway of aggregation abolished. The P2Y12 pathway of platelet activation is unaffected. Overall, there is a lessening of pro-aggregatory drive. There is an accompanying lessening in anti-aggregatory influence, as aspirin will also reduce the production of PGI2 by the blood vessel wall. (C) In the presence of a blocker of P2Y12 receptors, AC inhibition is lessened and so the anti-aggregatory effects of PGI2 are enhanced. As the effects of the TXA2 pathway are amplified through the P2Y12 pathway, the pro-aggregatory effects of TXA2 are also lessened and TXA2 production is reduced. (D) When aspirin is added to a P2Y12-receptor blocker, there may be some small additional reduction in pro-aggregatory influences by the complete removal of TXA2 production; however, there is also a loss of PGI2 which might lead to an even greater reduction in anti-aggregatory influence
