Abstract
Background
Currently, neither well-defined nor standardized measurement techniques exist for assessing deformity of extra-articular scapular fractures. To properly evaluate these injuries, compare observations across studies, and make clinical decisions, a validated measurement protocol for evaluating scapular fractures is needed.
Questions/purposes
We describe techniques to quantitatively characterize extra-articular scapular fracture deformity; evaluate the reliability of these characterizations in plain film radiographs and CT scans; and determine potential differences in the characterization of the deformity between the two imaging modalities.
Patients and Methods
We evaluated injury radiographs and three-dimensional CT images of 45 patients with extra-articular scapular fracture. Techniques for measuring medial/lateral displacement, angulation, translation, glenopolar angle, and glenoid version were established and utilized in two trials, performed 6 weeks apart, by three observers. We determined descriptive statistics for each measurement parameter.
Results
Interobserver reliability based upon interclass correlation coefficients ranged from 0.36 to 0.76 for radiographs and from 0.48 to 0.87 for three-dimensional CT. Intraobserver reliability using Pearson r coefficient ranged from 0.60 to 0.75 for radiographs and 0.64 to 0.89 for three-dimensional CT. Both individual and pooled measurements for angulation and glenopolar angle were higher on three-dimensional CT versus radiographs.
Conclusions
Our data suggest three-dimensional CT is more reliable than plain radiography in the assessment of scapula fracture displacement. Therefore, we believe this modality should be utilized if fracture deformity warrants surgical consideration and to adequately compare data across studies.
Level of Evidence
Level IV, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The diagnosis and characterization of scapular fractures can be difficult, resulting in missed or delayed diagnosis of this injury [4, 14, 17, 25, 27], thus leading potentially to malunion and persistent shoulder symptoms or loss of arm function [7, 8, 20, 22, 23]. There is controversy based on limited clinical evidence typically from small retrospective series for nonoperative [9, 20, 22, 28] versus operative [1, 5, 13, 15, 21] treatment of displaced scapular fractures. Further confusion exists from inconclusive definitions of shoulder instability, lack of defined operative criteria, and a poor understanding of risk factors for progressive fracture displacement. However, it is most obviously a lack of consensus on definitions of displacement and angular deformity that confounds communication and consensus regarding protocols for studying this injury and for clinical decision-making. Even if operative criteria and risk factors for scapula fracture instability were accepted, there are no well-defined measurement techniques for medialization, lateralization, translation, or angular deformity. Additionally, a variety of scapula fracture classification systems have been proposed [1, 10, 13], resulting in confusion on how best to describe scapula fractures. No one system is universally accepted and definitions and guidelines in the evaluation of these fractures are clearly needed.
We therefore (1) present techniques to characterize extra-articular scapular fracture deformity using five defined measurement parameters; (2) evaluate the reliability of these measurement techniques in two imaging modalities, plain film radiography and CT scan, using inter- and intraobserver reliability analyses; and (3) determine whether there was a difference in the readings of the deformity measurements between imaging modalities using comparative statistics where possible. If validated, these standardized measurements would provide clear definitions for future study and communication regarding this injury.
Patients and Methods
We selected 45 patients with extra-articular scapular fractures from an operative database to form the study cohort. All patients had scapular fractures involving the lateral border (scapula neck and/or body) and also had available for analysis complete preoperative radiographs and three-dimensional (3D) reconstructed CT scans (GE LightSpeed 16- to 64-slice CT [GE Healthcare, Waukesha, WI]; 2.5-mm slice thickness; reconstructed using TeraRecon 3D reconstruction software [TeraRecon, Inc, Foster City, CA]). Patients with intra-articular fractures were excluded to avoid adding a confounding variable to radiographic interpretation. We retrospectively analyzed AP scapula and lateral (scapula Y) radiographs and 3D CT scans of these 45 patients for deformity with regard to medial/lateral (M/L) displacement, translation, angulation, and glenopolar angle (GPA). Axial views of two-dimensional (2D) CT scans were used to measure glenoid version. Anatomic landmarks and measurement techniques were specifically defined for all five parameters. The study complied with all guidelines of the appropriate Institutional Review Board.
Independent measurements for these five parameters were performed by three observers at two separate readings, 6 weeks apart. These included a board-certified orthopaedic surgeon specializing in orthopaedic trauma (STG), an orthopaedic surgery resident (GK), and a clinical research fellow (JA). Each observer was blinded to the others’ readings. Radiographic views and CT scan images were preselected for all 45 patients to make certain all three observers were taking measurements from the same images. Each technique performed for the five measurement parameters was repeated in the same manner for both imaging modalities, radiography and 3D CT.
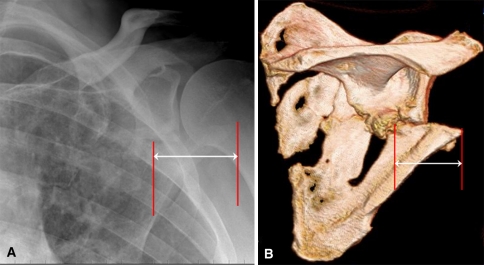
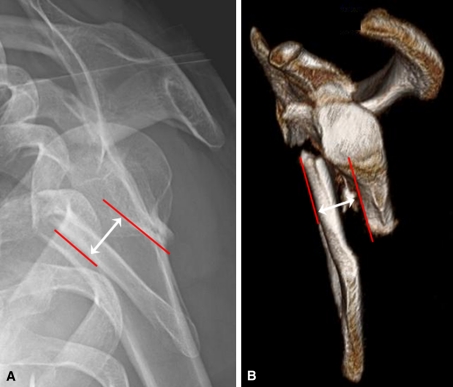
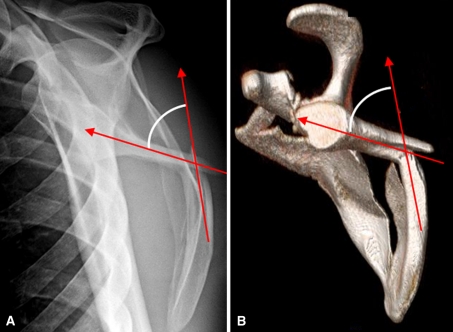
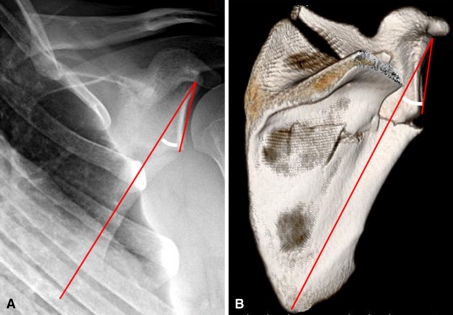
M/L displacement was measured on the AP scapula radiograph and the posteroanterior (PA) 3D CT scan image. The 3D CT image chosen was the rotational view with the longest lateral to medial scapular distance. This image frame could be thought of as the frame perpendicular to the beam of the xray. A vertical line was drawn down from the lateral-most extent of the proximal (superior) fragment. A second vertical line was drawn down from the lateral-most extent of the distal (inferior) fragment. The distance between the two vertical lines represented the M/L displacement as described previously by Armitage et al. [3] (Fig. 1). Translation was measured from the lateral (scapular Y) radiograph and the corresponding 3D CT image. A horizontal line was drawn, representing the displacement (translation) between the anterior (or posterior) cortices of superior and inferior fragments at the level of the fracture (Fig. 2). For the purpose of standardization, the 3D CT image chosen was always looking at the lateral side of the scapula with humerus subtracted from the image. Angulation was also measured on the lateral (scapular Y) radiographs and 3D CT images of the scapula. A line was drawn midway between and parallel to the anterior and posterior cortices of the proximal (superior) fragment. A second line was then drawn in the same fashion with regard to the distal (inferior) fragment. The angle formed by these two intersecting lines represented the angular deformity (Fig. 3). GPA, as described by Bestard et al. [6], was measured on the AP scapula radiograph and PA 3D CT scan image. A line was drawn beginning from the inferior to the superior pole of the glenoid fossa. From the superior pole, a second line was drawn straight to the apex of the inferior angle of the scapula body. The angle formed by these lines represented the GPA (Fig. 4). Axial 2D CT images were used to assess glenoid version since this is difficult to do with 3D CT accurately. The image depicting the largest diameter of the glenoid was preselected for the analysis. A line on the articular surface connecting the anterior and posterior glenoid rim was drawn. A second line was drawn perpendicular to this line. A third line was drawn through the midline of the displaced scapula body. The angle formed between the intersection of Lines 2 and 3 represented glenoid version (Fig. 5). Anteversion (+) and retroversion (−) were indicated.
Fig. 1A–B.
Measurement of M/L displacement on (A) an AP radiograph and (B) a PA 3D CT scan of the shoulder is demonstrated. M/L = mediolateral; PA = posterior–anterior; 3D = three-dimensional.
Fig. 2A–B.
Measurement of translation on (A) a transcapular Y radiograph and (B) a 3D CT scan is demonstrated. This represents the displacement marked by the distance between the anterior cortex of the proximal fragment and the anterior cortex of the distal fragment. 3D = three-dimensional.
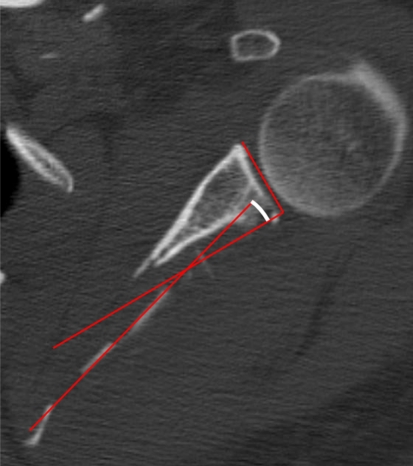
Fig. 3A–B.
Measurement of angulation on (A) a transcapular Y radiograph and (B) a 3D CT scan is demonstrated. A line is drawn through the proximal fragment in parallel with the cortices just proximal to the fracture. A second line is drawn through the distal fragment in parallel with the cortices just distal to the fracture. The angle formed by these two intersecting lines represents the angulation Note, even though the inferior teardrop forms a concave surface over the rib cage, it is the more proximal straight portion of the intramedullary canal that is used for the measurement (a critical distinction in measuring angular deformity so as not to overcall the angulation). 3D = three-dimensional.
Fig. 4A–B.
Measurement of the GPA on (A) a true AP radiograph and (B) a PA 3D CT scan of the shoulder is demonstrated. A line is drawn from the inferior pole of the glenoid fossa up to the superior pole. Another line is drawn from the superior pole of the glenoid fossa down through the inferior-most angle of the scapula body. The angle formed by these two intersecting lines represents the GPA. Normal GPAs range from 30° to 45° [6]. GPA = glenopolar angle; 3D = three-dimensional.
Fig. 5.
Measurement of glenoid version on an axial CT scan image is demonstrated. A line is drawn connecting the anterior and posterior glenoid rim. A second line is drawn perpendicular to this line. A third line is drawn through the midline of the displaced scapula body. The angle formed between the intersection of Lines 2 and 3 represents glenoid version. In this case, the glenoid is retroverted, which is an uncommon finding as the glenoid is usually anteverted after fracture.
One conference was held, including all readers, before the initiation of the first trial to uniformly educate the readers on the measurement methodology. No additional training sessions were provided between Trial 1 and Trial 2. Interobserver reliability was computed among all three observers on the five measurement parameters for deformity on radiographs and CT scans. Interobserver reliability for the three observers was computed separately for each parameter for each trial (Trials 1 and 2) and was summarized with the intraclass correlation coefficient (ICC) designated by Shrout and Fleiss [24] as ICC(2,1). Intraobserver reliability was computed separately for each parameter pooling all observers for Trial 1 versus Trial 2 and was summarized using the Pearson r coefficient [2]. In all analyses, the corresponding 95% confidence interval (CI) was calculated and recorded.
With regard to angulation and GPA, the individual measurements taken on radiographs were compared to those taken on 3D CT scan for the 45 patients by each observer for both trials and the difference was calculated. Next, the mean measurements pooled across the 45 patients for each observer and the means pooled across all three observers were compared and the differences were calculated for both trials. A mixed-effects model, F(1,44), which examined the effect of judge and modality (radiograph or 3D CT), was used to effectively pool all data for each trial and treat the judge and modality as within-subjects factors. Paired t tests comparing radiographs and 3D CT scans for angulation and GPA were utilized separately for each observer for both trials. These comparative statistics were not possible for M/L displacement and translation because displacement for these parameters was measured in millimeters on radiographs and pixels on 3D CT scan, whereas for angulation and GPA, both were measured in degrees of angular deformity.
Results
The descriptive statistics for each of the five measurement parameters performed on the 45 patients included in the study cohort are summarized (Table 1). The mean for each parameter is pooled across all three readers for each trial.
Table 1.
Descriptive statistics for five measurement parameters
| Measurement parameter | Radiograph | 3D CT/2D CT* | ||||||
|---|---|---|---|---|---|---|---|---|
| Trial 1† | Trial 2 | Trial 1 | Trial 2 | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| M/L displacement‡ | 25.1 | 10.3 | 22.6 | 10.8 | 47.1 | 30.0 | 43.0 | 30.9 |
| Translation‡ | 12.8 | 7.9 | 14.0 | 6.8 | 21.6 | 16.5 | 22.4 | 14.2 |
| Angulation (°) | 12.5 | 10.3 | 11.6 | 11.0 | 19.4 | 11.2 | 17.7 | 12.7 |
| GPA (°) | 28.2 | 6.8 | 27.1 | 6.6 | 34.1 | 5.5 | 34.1 | 5.6 |
| Glenoid version (°) | NA | NA | NA | NA | 8.0 | 9.8 | 8.4 | 9.5 |
* M/L displacement, translation, angulation and GPA were measured on 3D CT; glenoid version was measured on 2D CT; †three observers’ readings were pooled for each trial; ‡linear units for M/L displacement and translation were millimeters for radiographs and pixels for 3D CT; 3D = three-dimensional; 2D = two-dimensional; M/L = medial/lateral; GPA = glenopolar angle; NA = not applicable.
Interobserver reliability ICCs ranged from 0.36 to 0.76 for radiographs and ranged from 0.48 to 0.87 for 3D CT (Table 2). Since each observer obtained measurements from the same patients’ films on two occasions (Trials 1 and 2) separated by 6 weeks, it was possible to assess the intraobserver reliability for each of the five measurement parameters as well. Intraobserver reliability Pearson r coefficients ranged from 0.60 to 0.75 for radiographs and 0.64 to 0.89 for 3D CT (Table 3). In regard to both inter- and intraobserver reliability, glenoid version cannot be measured on radiographs.
Table 2.
Interobserver reliability of three observers’ ratings for five measurement parameters
| Measurement parameter | Radiograph | 3D CT/2D CT* | ||||||
|---|---|---|---|---|---|---|---|---|
| Trial 1 | Trial 2 | Trial 1 | Trial 2 | |||||
| ICC | 95% CI | ICC | 95% CI | ICC | 95% CI | ICC | 95% CI | |
| M/L displacement | 0.49 | 0.17–0.71 | 0.36 | 0.04–0.62 | 0.48 | 0.13–0.71 | 0.51 | 0.23–0.71 |
| Translation | 0.68 | 0.54–0.79 | 0.53 | 0.36–0.68 | 0.80 | 0.70–0.88 | 0.60 | 0.44–0.74 |
| Angulation | 0.59 | 0.42–0.73 | 0.57 | 0.41–0.72 | 0.66 | 0.48–0.79 | 0.80 | 0.70–0.88 |
| GPA | 0.76 | 0.64–0.85 | 0.55 | 0.38–0.70 | 0.83 | 0.74–0.90 | 0.87 | 0.80–0.92 |
| Glenoid version | NA | NA | NA | NA | 0.84 | 0.75–0.91 | 0.74 | 0.62–0.84 |
* M/L displacement, translation, angulation and GPA were measured on 3D CT; glenoid version was measured on 2D CT; 3D = three-dimensional; 2D = two-dimensional; ICC = interclass correlation coefficient; CI = confidence interval; M/L = medial/lateral; GPA = glenopolar angle; NA = not applicable.
Table 3.
Intraobserver reliability of three observers’ ratings in Trial 1 versus Trial 2 for five measurement parameters
| Measurement parameter | Radiograph | 3D CT/2D CT* | ||
|---|---|---|---|---|
| r | 95% CI | r | 95% CI | |
| M/L displacement | 0.75 | 0.67–0.82 | 0.72 | 0.63–0.79 |
| Translation | 0.60 | 0.48–0.70 | 0.64 | 0.53–0.73 |
| Angulation | 0.66 | 0.55–0.74 | 0.79 | 0.71–0.84 |
| GPA | 0.62 | 0.50–0.71 | 0.89 | 0.85–0.92 |
| Glenoid version | NA | NA | 0.83 | 0.77–0.88 |
* M/L displacement, translation, angulation and GPA were measured on 3D CT; glenoid version was measured on 2D CT; 3D = three-dimensional; 2D = two-dimensional; r = Pearson r coefficient; CI = confidence interval; M/L = medial/lateral; GPA = glenopolar angle; NA = not applicable.
Using the mean measurements for angulation and GPA pooled across 45 patients for all three observers in both trials, a difference was found in readings from radiographs versus 3D CT for GPA in both Trials 1 and 2 (p < 0.0001 and p = 0.0002), as well as for angulation (p < 0.0001 and p < 0.0001) (Table 4). In addition, in a comparison of the readings from the two different imaging modalities, we found, for Trial 1, angulation readings were greater on 3D CT scans than on radiographs in 28 of 45 (62%) readings for Observer 1, 33 of 45 (73%) readings for Observer 2, and 31 of 45 (69%) readings for Observer 3. For Trial 2, this was observed in 30 of 45 (67%) readings for Observer 1, 31 of 45 (69%) readings for Observer 2, and 32 of 45 (71%) readings for Observer 3. For Trial 1, GPA readings were greater on 3D CT scans than on radiographs in 39 of 45 (87%) readings for Observer 1, 33 of 45 (73%) readings for Observer 2, and 37 of 45 (82%) readings for Observer 3. For Trial 2, this was observed in 40 of 45 (89%) readings for Observer 1, 41 of 45 (91%) readings for Observer 2, and 41 of 45 (91%) readings for Observer 3.
Table 4.
Difference in mean angular measurements between radiographs and 3D CT
| Measurement parameter | Modality | Trial 1 | Trial 2 | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Angulation (°) | Radiograph | 12.5 | 10.3 | 11.6 | 11.0 |
| 3D CT | 19.4 | 11.2 | 17.7 | 12.7 | |
| Difference | 6.9 | 12.0 | 6.1 | 12.3 | |
| p value | < 0.0001 | 0.0002 | |||
| GPA (°) | Radiograph | 28.2 | 6.8 | 27.1 | 6.6 |
| 3D CT | 34.1 | 5.5 | 34.1 | 5.6 | |
| Difference | 6.0 | 6.7 | 7.0 | 6.0 | |
| p value | < 0.0001 | < 0.0001 | |||
3D = three-dimensional; GPA = glenopolar angle.
Discussion
Radiographic measurements of fracture displacement form the basis for data collection, outcome assessment, and clinical decision-making. Radiographic assessment of any fracture is best performed by adhering to standardized techniques and systematic guidelines. We presented techniques to characterize extra-articular scapular fractures using five defined measurement parameters, evaluated the reliability of these measurement techniques in two imaging modalities using inter- and intraobserver reliability analyses, and determined whether there was a difference in the deformity measurements between imaging modalities.
There were limitations to our study. First, the injury CT scan from which these measurements were performed was preselected. Had the observers each selected the images independently to read, inter- and intraobserver variability may have increased. However, we chose not to introduce a confounding variable to determine the effect of different readings on one radiograph versus one CT image. The authors believe clear guidelines for selection of the PA and lateral CT images (ie, the rotational view with the longest lateral to medial scapular distance) would be easily applied in the clinical setting. Second, we selected particular measures we believed important for evaluating these injuries. Other measures could have been selected or developed and the variability could have differed.
Ada and Miller [1] reported pain and weakness in patients with lateral border displacement of more than 1 cm and angulation of more than 40° and, therefore, recommended operative treatment in these cases. Romero et al. [23] and Bozkurt et al. [7] correlated pain and impaired function in patients with an abnormal GPA (< 20° [7]). However, these authors did not provide a detailed description as to how these parameters were measured. Accurate and validated guidelines for measuring fracture displacement are paramount and particularly so for a less common fracture that is not well studied by most clinicians.
Several authors have highlighted the importance of CT in the assessment of scapular fractures [11, 12, 16, 19, 20]. Some agree 3D CT is necessary to accurately understand scapular fractures due to the complex anatomy [11, 12, 19]. Data compiled by McAdams et al. [18] showed the amount of displacement and angulation of scapula neck fractures is difficult to assess reliably on plain shoulder radiographs and axial 2D CT scans. However, in this study, the observers simply recorded whether there was displacement of less than or greater than 1 cm and whether there was angulation of less than or greater than 40°. This expression thereby leaves the true reliability of these radiographic modalities yet to be determined. Tadros et al. [26] have shown scapula trauma films are useful in detecting fractures of the scapula body, spine, and acromion fractures, but not coracoid, glenoid, and scapula neck fractures. They also showed 2D CT scans had low sensitivity with regard to detecting scapula neck and spine fractures, while 3D CT had high sensitivity for detecting fractures in all anatomic regions of the scapula, thereby having the greatest utility index of all three imaging modalities [26]. We provided systematic guidelines for measurement of displacement in extra-articular scapular fractures using five different measurement parameters. We then assessed the reliability of these measurements performed based upon two imaging modalities, radiographs and 3D CT scans. According to our assessment of inter- and intraobserver reliability, measurements for angulation, translation, and GPA were more reliable when performed on 3D CT than on radiographs, while reliability for M/L displacement was comparable (Tables 2 and 3).
Our data show, for each observer and across all observers, there was a difference in angular deformity as measured by angulation and GPA, when comparing measurements taken on radiographs and 3D CT scan, such that the values were higher with 3D CT scan (Table 4). We attribute this to the inaccuracy of obtaining a true AP and lateral image of the scapula using radiography. Any slight deviation from a true AP or lateral position will result in a decrease in both measured angulation and GPA as the image is rotated in the sagittal and coronal planes, respectively. Thus, measurements taken from radiographs often will give an underestimation of the true underlying deformity. It is reasonable to presume M/L displacement and translation deformity will also be affected by the same underlying phenomenon. Additionally, on a scapula Y radiograph, the cortices of the humerus often overlap with that of the scapula, making it more difficult to identify key landmarks, and in an axial view using 2D CT, the glenoid and scapula body must be visualized to accurately measure glenoid version. In addition, 3D CT provides the capability of demonstrating all anatomic details of the scapula, while reducing the adverse impact from factors such as patient body habitus, positioning, and technician experience and variability. Nevertheless, we believe a screening scapula radiographic trauma series remains useful as an economical diagnostic screen to identify a fracture, the relationship of fragments, and the proper relative location of the glenoid and humeral head.
In summary, our findings demonstrate CT scans are more reliable than plain radiographs to assess scapula fracture displacement by all known criteria. Furthermore, there is acceptable correlation among and within observers using this modality to measure translation and angulation in three planes (glenoid version, scapula Y angulation, and GPA). These measurements serve as a foundation for systematic injury assessment, comparisons between studies, and clinical decisions.
Acknowledgment
The authors thank Stephen E. Asche, MA, for his contributions to the study design, statistical analyses, and interpretation of the data.
Footnotes
The institution of the authors has received funding for this research from Zimmer, Inc (Warsaw, IN) and Synthes, Inc (West Chester, PA).
Each author certifies that his institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
At the time of this study, certain authors (JA, JC, GK, TG) were affiliated with the institution where Institutional Review Board study approval was attained.
This work was performed at the University of Minnesota, Regions Hospital, St Paul, MN, USA.
Contributor Information
Jack Anavian, Email: janavianmd@gmail.com.
Joseph M. Conflitti, Email: jmconflitti@etmc.org.
Gaurav Khanna, Email: khan0044@gmail.com.
S. Trent Guthrie, Email: trentguthrie@earthlink.net.
Peter A. Cole, Email: peter.a.cole@healthpartners.com.
References
- 1.Ada JR, Miller ME. Scapular fractures: analysis of 113 cases. Clin Orthop Relat Res. 1991;269:174–180. [PubMed] [Google Scholar]
- 2.Aday L, Cornelius L. Designing and Conducting Health Surveys: A Comprehensive Guide. 3rd ed. San Francisco, CA: Jossey-Bass Publishers; 2006:45.
- 3.Armitage BM, Wijdicks CA, Tarkin IS, Schroder LK, Marek DJ, Zlowodzki M, Cole PA. Mapping of scapular fractures with three-dimensional computed tomography. J Bone Joint Surg Am. 2009;91:2222–2228. doi: 10.2106/JBJS.H.00881. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong CP, Spuy J. The fractured scapula: importance and management based on a series of 62 patients. Injury. 1984;15:324–329. doi: 10.1016/0020-1383(84)90056-1. [DOI] [PubMed] [Google Scholar]
- 5.Bauer G, Fleischmann W, Dussler E. Displaced scapular fractures: indication and long-term results of open reduction and internal fixation. Arch Orthop Trauma Surg. 1995;114:215–219. doi: 10.1007/BF00444266. [DOI] [PubMed] [Google Scholar]
- 6.Bestard EA, Schvene HR, Bestard EH. Glenoplasty in the management of recurrent shoulder dislocation. Contemp Orthop. 1986;12:47–55. [Google Scholar]
- 7.Bozkurt M, Can F, Kirdemir V, Erden Z, Demirkale I, Basbozkurt M. Conservative treatment of scapular neck fracture: the effect of stability and glenopolar angle on clinical outcome. Injury. 2005;36:1176–1181. doi: 10.1016/j.injury.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 8.Chadwick EK, Noort A, Helm FC. Biomechanical analysis of scapular neck malunion—a simulation study. Clin Biomech (Bristol, Avon) 2004;19:906–912. doi: 10.1016/j.clinbiomech.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 9.Edwards SG, Whittle AP, Wood GW., 2nd Nonoperative treatment of ipsilateral fractures of the scapula and clavicle. J Bone Joint Surg Am. 2000;82:774–780. doi: 10.1302/0301-620X.82B5.11311. [DOI] [PubMed] [Google Scholar]
- 10.Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma. 1996;10(Suppl 1):v-ix, 1–154. [PubMed]
- 11.Goss TP. Scapular fractures and dislocations: diagnosis and treatment. J Am Acad Orthop Surg. 1995;3:22–33. doi: 10.5435/00124635-199501000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Haapamaki V, Kiuru M, Koskinen S. Multidetector CT in shoulder fractures. Emerg Radiol. 2004;11:89–94. doi: 10.1007/s10140-004-0376-x. [DOI] [PubMed] [Google Scholar]
- 13.Hardegger FH, Simpson LA, Weber BG. The operative treatment of scapular fractures. J Bone Joint Surg Br. 1984;66:725–731. doi: 10.1302/0301-620X.66B5.6501369. [DOI] [PubMed] [Google Scholar]
- 14.Harris RD, Harris JH., Jr The prevalence and significance of missed scapular fractures in blunt chest trauma. AJR Am J Roentgenol. 1988;151:747–750. doi: 10.2214/ajr.151.4.747. [DOI] [PubMed] [Google Scholar]
- 15.Jones CB, Cornelius JP, Sietsema DL, Ringler JR, Endres TJ. Modified Judet approach and minifragment fixation of scapular body and glenoid neck fractures. J Orthop Trauma. 2009;23:558–564. doi: 10.1097/BOT.0b013e3181a18216. [DOI] [PubMed] [Google Scholar]
- 16.Kopecky KK, Bies JR, Ellis JH. CT diagnosis of fracture of the coracoid process of the scapula. Comput Radiol. 1984;8:325–327. doi: 10.1016/0730-4862(84)90045-3. [DOI] [PubMed] [Google Scholar]
- 17.Martin SD, Weiland AJ. Missed scapular fracture after trauma: a case report and a 23-year follow-up report. Clin Orthop Relat Res. 1994;299:259–262. [PubMed] [Google Scholar]
- 18.McAdams TR, Blevins FT, Martin TP, DeCoster TA. The role of plain films and computed tomography in the evaluation of scapular neck fractures. J Orthop Trauma. 2002;16:7–11. doi: 10.1097/00005131-200201000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Ng GP, Cole WG. Three-dimensional CT reconstruction of the scapula in the management of a child with a displaced intra-articular fracture of the glenoid. Injury. 1994;25:679–680. doi: 10.1016/0020-1383(94)90014-0. [DOI] [PubMed] [Google Scholar]
- 20.Nordqvist A, Petersson C. Fracture of the body, neck, or spine of the scapula: a long-term follow-up study. Clin Orthop Relat Res. 1992;283:139–144. [PubMed] [Google Scholar]
- 21.Nork SE, Barei DP, Gardner MJ, Schildhauer TA, Mayo KA, Benirschke SK. Surgical exposure and fixation of displaced type IV, V, and VI glenoid fractures. J Orthop Trauma. 2008;22:487–493. doi: 10.1097/BOT.0b013e31817d5356. [DOI] [PubMed] [Google Scholar]
- 22.Pace AM, Stuart R, Brownlow H. Outcome of glenoid neck fractures. J Shoulder Elbow Surg. 2005;14:585–590. doi: 10.1016/j.jse.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 23.Romero J, Schai P, Imhoff AB. Scapular neck fracture—the influence of permanent malalignment of the glenoid neck on clinical outcome. Arch Orthop Trauma Surg. 2001;121:313–316. doi: 10.1007/s004020000224. [DOI] [PubMed] [Google Scholar]
- 24.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 25.Tadros AM, Lunsjo K, Czechowski J, Abu-Zidan FM. Causes of delayed diagnosis of scapular fractures. Injury. 2008;39:314–318. doi: 10.1016/j.injury.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 26.Tadros AM, Lunsjo K, Czechowski J, Corr P, Abu-Zidan FM. Usefulness of different imaging modalities in the assessment of scapular fractures caused by blunt trauma. Acta Radiol. 2007;48:71–75. doi: 10.1080/02841850601026435. [DOI] [PubMed] [Google Scholar]
- 27.Thompson DA, Flynn TC, Miller PW, Fischer RP. The significance of scapular fractures. J Trauma. 1985;25:974–977. doi: 10.1097/00005373-198510000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Noort A, Kampen A. Fractures of the scapula surgical neck: outcome after conservative treatment in 13 cases. Arch Orthop Trauma Surg. 2005;125:696–700. doi: 10.1007/s00402-005-0044-y. [DOI] [PubMed] [Google Scholar]