Abstract
Background
Locking plate fixation of proximal humeral fractures improves biomechanical stability. It has expanded the indications of traditional open reduction internal fixation and become increasingly common for treating unstable, displaced proximal humeral fractures. Despite improved stability it is unclear whether these improve function and if so for which patients.
Questions/purposes
We therefore determined patient function after a locked plating technique for the treatment of unstable proximal humeral fractures based on age, time, fracture pattern, and associated injures.
Patients and Methods
We retrospectively reviewed 66 patients with 69 proximal humeral fractures treated with a locked proximal humeral plating technique from 2002–2006 using prospectively gathered data. Function was measured using the Short Musculoskeletal Function Assessment (SMFA), Disability of the Arm, Shoulder, and Hand (DASH), and SF-36 at 6, 12, and 24 months. Fracture healing was determined radiographically and complication rates were determined from the medical records.
Results
At 2 years, DASH scores were 26.5 and 37.4 for isolated and polytrauma patients, respectively. For age differences, DASH scores were 33.1 and 28.9 for ages younger than 60 and 60 years old or older, respectively. At 2 years, SMFA scores were higher (worse) in older compared with younger patients. Function, but not bother continues to improve in younger patients up to 2 years. More severe fracture patterns performed worse in all SMFA indices at 2 years. Polytrauma patients consistently experienced worse mobility than isolated injury patients at each time interval.
Conclusions
With locked plating of unstable proximal humeral fractures, older patients function as well as younger patients; improvement continues until 1 year postoperatively, the Neer fracture classification differentiates function, and polytrauma patients perform worse clinically. Long-term functional deficits persist.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Fractures of the proximal humerus represent 4% to 5% of all fractures [4, 5, 13, 18]. These fractures occur in a bimodal frequency with younger high-energy and older lower-energy mechanisms. Because most proximal humeral fractures are minimally displaced and stable, these fractures can be treated nonoperatively [13, 52]. Osteoporosis, comminution, short-segment fracture length, and displacement complicate stabilization, fracture healing, and functional results [20, 22–25, 27, 28, 30, 31, 36, 39]. Despite stable rates of proximal humeral fractures, increasing rates of surgical treatment have been reported [7]. Various methods of stabilization are reported in the literature [28]. Open reduction with internal fixation (ORIF) for such fractures can aid in stability and allow the patient to begin early mobilization and rehabilitation [16, 17, 21, 28]. The methods of fixation and operative techniques have evolved over the years. Such fixation has included closed reduction with percutaneous pinning [19, 33], tension band wiring [11, 12, 15, 37], plate fixation [7, 8], intramedullary nailing [1, 41], and hemiarthroplasty [26, 28]. More recently, the advent of locked plate technology has increased ORIF indications and some surgeons are replacing the previously mentioned fixation methods with locked plates [28]. With increasing rates of operative fixation with locking plates, complications still exist [2]. Complications of hardware failure (0–4%), hardware removal (1–8%), intra-articular hardware (0–23%), varus deformity (0–25%), infections (2–5%), osteonecrosis (0–7%), subacromial impingement (0–14%), and fixation revision (6–16%) have been reported [10, 14, 18, 29, 38, 40, 42, 46, 48, 50].
Locking plates for proximal humeral fractures reportedly do not improve patient outcome, adverse events, or complications [3]. Most of the studies evaluating outcome measurements have used the Constant-Murley or the Disabilities of Arm, Shoulder, and Hand (DASH) [18, 29, 38, 40, 42]. Only one study used the Short Form Musculoskeletal Functional Assessment (SMFA) [46]. Only one study used the SF-36 [48]. Despite many of these studies evaluating the outcomes of locked plating, none has combined the DASH, SF-36, and SFMA for comparison. Increasing complications have been related to increasing age and osteoporosis [46]. Age in correlation to outcome has not been independently evaluated. The longest followup has been 1 year or less [18, 29, 38, 40, 42, 46, 48]. A more severe fracture pattern has been correlated with increased complications with locking plate application [46]. Furthermore, none of the studies has compared patients with isolated injuries and polytrauma patients.
Therefore, we determined whether (1) age; (2) interval time after surgery up to 2 years; (3) fracture pattern; and (4) associated injuries affected prospectively obtained functional outcome measurements after locking plate treatment of unstable displaced proximal humeral fractures. Furthermore, long-term functional outcome measurements were compared with validated normative outcome measurements.
Patients and Methods
We retrospectively reviewed 303 patients with 307 proximal humeral fractures treated from January 2002 through December 2006. Patients were identified by current procedural terminology codes 23600, 23605, 23615, and 23616 for proximal humeral fracture. The indications for locked plating were: (1) translated, unstable, and displaced fracture pattern of metaphyseal and/or head fragments; (2) intra-articular head-splitting injuries; (3) angulation of more than 45º of varus, valgus, or apex anterior; (4) metaphyseal and/or diaphyseal comminution; (5) osteoporosis; (6) open fractures; and (7) associated neurovascular injuries. The contraindications were: (1) isolated greater or lesser tuberosity fractures; (2) medical comorbidity precluding operative intervention; and (3) nonreconstructable head and/or tuberosity fragments. We excluded patients treated nonoperatively (99), with arthroplasty (21), operatively without locking plate (ie, percutaneous pins [91]), and those with incomplete data (26). These exclusions left 66 patients (22%) with 69 fractures treated with locked proximal humeral plates. All of these patients had followup radiographs, clinical examinations, and prospectively obtained outcome measurements at regularly scheduled intervals of 6 months, 12 months, and 2 years. The minimum followup was 24 months (average, 25 months; range, 24–47 months). No patients were lost to followup. No patients were recalled specifically for our study; all data were obtained from medical records and radiographs. We had prior Institutional Review Board approval.
Average age was 61 years (range, 23–89 years) with a typical bimodal distribution of young (younger than 60 years, n = 34; average, 48 years; range, 23–59 years) and old (60 years or older, n = 32; average, 75 years; range, 61–89 years). Given the bimodal distribution, we divided patients into a younger group (younger than 60 years) and an older group (60 years or older). There were more females (42 females versus 24 males). The mechanism was varied by cause and age (Table 1). Low-energy falls were most common followed by motor vehicle accidents, high-energy falls, motorcycle accident, and altercation. Older compared with younger patients had more low-energy falls (26 versus 10) but less high-energy falls (0 versus 11). Of the 40 isolated fracture cases, 16 (40%) were found in younger patients and 24 (60%) in older patients. Of the 26 polytrauma patients, 17 (65%) were found in younger patients and nine (35%) in older patients. Occupation was recorded as unknown, unemployed, retired, homemaker, sedentary (lifting less than 10 pounds), light duty (lifting 10–20 pounds), moderate duty (lifting 20–50 pounds), or heavy duty (lifting greater than 50 pounds). The occupation was unemployed (nine [14%]), retired (22 [33%]), homemaker (three [5%]), sedentary (four [6%]), light duty (nine [14%]), moderate duty (five [8%]), heavy duty (seven [10%]), or unknown (seven [10%]) at the time of injury.
Table 1.
Mechanism of injury
| Mechanism | Frequency (%) | Younger than 60 years | 60 years or older |
|---|---|---|---|
| Low-energy fall | 36 (54%) | 10 | 29 |
| High-energy fall | 11 (16%) | 11 | 0 |
| Motor vehicle accident | 17 (26%) | 12 | 5 |
| Motorcycle accident | 1 (2%) | 1 | 0 |
| Altercation | 1 (2%) | 0 | 1 |
| Total | 66 (100%) | 34 | 32 |
Radiographics were reviewed by two surgeons (CBJ, DKW) to grade fracture pattern and severity using the Neer classification [43–45]. Discrepancies were resolved by consensus. Neer fracture classification was recorded as two-part (32 [46%]), three-part (19 [28%]), or four-part (18 [26%]) fractures. Associated ipsilateral injuries were head split fracture with marginal impaction (six), diaphyseal extension (nine), and glenoid neck (one). Seventeen of the 69 fractures (25%) had associated osteoporosis noted on radiographs and/or intraoperatively.
Two periarticular locking plate systems were implanted (Synthes n = 35 [51%], Paoli, PA; and Zimmer n = 34 [49%], Warsaw, IN) with similar frequencies. Fractures were treated within 2 weeks of injury. A 2-week limit was chosen to include acute injuries and to exclude healing fractures, pre-existing callus, disuse atrophy, or conversion of failed closed to open treatment. Three fellowship-trained orthopaedic trauma surgeons (CBJ, JRR, TJE) performed all operative procedures.
A deltopectoral approach was used in all patients. Patient positioning was supine on a radiolucent table. All patients had surgery under general anesthetic. Regional pain control was patient-, surgeon-, and anesthesiologist-dependent. Fracture reduction was accomplished with a joystick (2.5-mm terminally threaded Schanz pins; Synthes) control. Tuberosity reduction and maintenance were accomplished using Number 2 Ethibond (Ethicon, Inc, New Brunswick, NJ) sutures as a tension band through the plate holes. The number of head screws, number of shaft screws, and use of a suture tension band were recorded and determined by surgeon preference. Radiographs were obtained intraoperatively with fluoroscopy.
Postoperative therapy began when pain diminished and patients were able to participate in an organized physical therapy program, which was coordinated at the first office visit, 2 weeks postoperatively. The first 6 postoperative weeks included passive forward flexion and abduction ROM up to 180°, no external rotation more than neutral, and no lifting greater than 10 pounds. After 6 weeks postoperatively, unlimited ROM in all planes and unlimited strengthening were instituted. Sling or immobilizer assistance was used initially for support of the extremity but strongly discouraged after the first 2 to 4 weeks postoperatively.
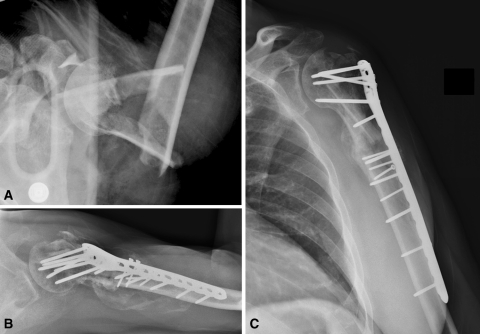
Clinical and radiographic followup was performed at intervals of 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and 2 years postoperatively. Clinical examination included affected extremity ROM, strength, and pain. We obtained true AP or Grashey view and axillary radiographs (Fig. 1). Complications were recorded such as avascular necrosis, intra-articular hardware, peri-implant fracture, and need for further surgery. Return to previous activities/occupation was also recorded. General health and musculoskeletal function outcome scores were obtained in a prospective manner at the 6-, 12-, and 24-month intervals from the time of surgery. Functional outcome measurements were compared with validated normative data [32]. The SMFA consists of 34 items comprising the dysfunction index, which assesses patient function including subscores of daily activity, emotional, arm/hand, and mobility, and 12 items comprising the bother index, which assesses how much patients are bothered by functional problems [49]. A lower score denotes improved function and a decreased perceived bother. The SMFA is widely used with high reliability (Cronbach’s alpha equals 0.93 for the dysfunction index and 0.88 for the bother index). The DASH survey evaluates disability and symptoms in single or multiple disorders of the upper limb at one point or at many points in time [6]. Low scores indicate better function with fewer related symptoms. Test-retest reliability (intraclass correlation = 0.96) exceeded reported guidelines [6]. The SF-36 is a general health instrument that has eight components to assess physical functioning, role limitations caused by physical problems, bodily pain, general health, vitality, social functioning, role limitations caused by emotional problems, and mental health [51]. These eight health concepts constitute the physical and mental component summary measures. High scores represent improved functioning and general health. Score reliability for the SF-36 scales exceeds 0.80 in all categories with physical functioning notably at 0.90.
Fig. 1.
(A) A healthy 52-year-old man fell 15 feet and presented with an isolated open comminuted proximal humeral fracture. The injury AP radiograph demonstrates comminution, displacement, malalignment, and short proximal segment of the humeral head. The fracture was acutely repaired with open locked plating to stabilize the humeral head short segment, fibular strut grafting to bypass segmental comminution, and tension suture fixation of tuberosities to neutralize distraction forces. (B) The axillary view demonstrates no angulation or intra-articular screw penetration. (C) The AP view demonstrates bridging of comminution and re-establishment of anatomical relationships.
We obtained descriptive statistics to describe the sample, surgical results, and distribution of functional scores. We used Chi-square analysis to compare demographic variables such as mechanism of injury and isolated injury versus polytrauma between the two age groups and used T-tests to compare functional scores between the two age groups, isolated injury versus polytrauma for the DASH, and at each time interval of the SMFA. A change over time in functional outcomes was determined using repeated-measures analyses of variance (ANOVAs) for the SMFA and SF-36. A difference in functional outcomes based on the three Neer fracture patterns was determined by ANOVA. Data analyses were performed with the Statistical Package for the Social Sciences (SPSS) Version 15.0 (SPSS Inc, Chicago, IL).
Results
When grouping younger (younger than 60 years) versus older (60 years or older), high-energy mechanism was more common (p < 0.001) in the younger group. A greater incidence (p = 0.046) of polytrauma occurred in the younger group. Younger patients had a greater occurrence of polytrauma (p = 0.012). When evaluating SMFA scores, younger tended to improve until the 2-year mark with regard to dysfunction and arm/hand but not for bother, whereas the older patients remained stable (Table 2). At the 12-month interval, the younger group had worse (p = 0.049) bother scores than the older patient group. At the 6- and 12-month intervals, the younger group had worse emotional scores as compared with the older patient group (p = 0.030 and p = 0.044, respectively). Arm/hand function was similar at all time intervals and DASH scores were similar between age groups at 24 months (Table 3).
Table 2.
Average SMFA index scores for age at 6-, 12-, and 24-month intervals
| 6 months | 12 months | 24 months | |||||||
|---|---|---|---|---|---|---|---|---|---|
| SMFA index | Younger than 60 years | 60 years or older | Significance | Younger than 60 years | 60 years or older | Significance | Younger than 60 years | 60 years or older | Significance |
| Dysfunction | 26 | 29 | 22 | ||||||
| 24 | 28 | 32 | |||||||
| Bother | 33 | 30 | 32 | ||||||
| 26 | 18 | 0.049 | 24 | ||||||
| Arm/hand | 18 | 16 | 12 | ||||||
| 18 | 17 | 19 | |||||||
| Mobility | 24 | 29 | 21 | ||||||
| 22 | 31 | 26. | |||||||
| Daily activity | 28 | 30 | 22 | ||||||
| 32 | 33 | 46 | 0.030 | ||||||
| Emotional | 41 | 43 | 36 | ||||||
| 27 | 0.030 | 32 | 0.044 | 32 | |||||
SMFA = Short Musculoskeletal Function Assessment.
Table 3.
DASH scores at 24-month intervals
| 24-month DASH | Total | Younger than 60 years | 60 years or older | Isolated | Polytrauma |
|---|---|---|---|---|---|
| Mean | 31 | 33 | 28 | 26 | 37 |
| Range | 22–77 | 2–75 | 2–78 | 2–75 | 6–77 |
DASH = Disabilities of the Arm, Shoulder and Hand.
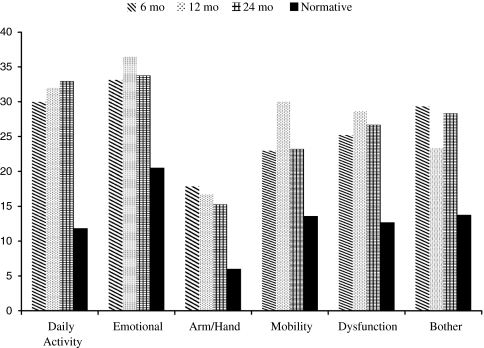
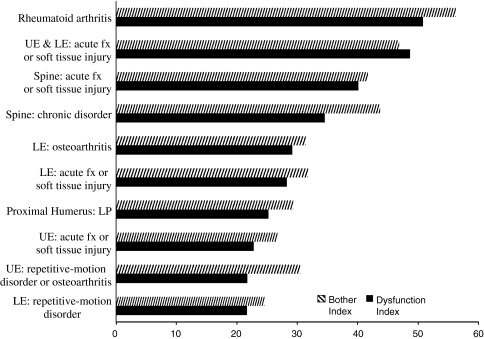
At the 6-month interval, differences in arm/hand, mobility, daily activity, and emotional measurements were noted between the Neer fracture patterns (Table 4). At all time intervals, differences in arm/hand measurements were noted between Neer two-part versus Neer three-part fractures and Neer two-part and Neer four-part fractures, but not between the Neer three-part and Neer four-part fractures except at 2 years. Differences in arm/hand measurements were noted among Neer two-, three-, and four-part fractures with dysfunction corresponding to more severe Neer fracture patterns. At 2 years, more severe fracture patterns performed worse in all SMFA indices. The Neer four-part fractures demonstrated declines in function, bother, arm/hand, mobility, and emotional over time, whereas the Neer two- and three-part did not. Through the 2-year time period, daily activity, emotional, arm/hand, mobility, dysfunction, and bother scores continue to be worse (p < 0.05) than normative scores (Fig. 2). Compared with other acute and chronic conditions, bother and dysfunction persist for proximal humeral fractures treated with locked plates (Fig. 3). SF-36 health indices declined across all subscores except bodily pain and general health remained stable at the 12-month interval and improved at the 24-month interval (Table 5). The emotional role category was the only area that demonstrated a significant improvement (p = 0.003) over time.
Table 4.
Average SMFA index scores for Neer classification at 6-, 12-, and 24-month intervals
| 6 months | 12 months | 24 months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SMFA index | Two-part | Three-part | Four-part | Significance | Two-part | Three-part | Four-part | Significance | Two-part | Three-part | Four-part | Significance |
| Dysfunction | 18 | 23 | 0.041 (2 and 3) | 20 | 0.010 (2 and 4) | |||||||
| 28 | 35 | 27 | 0.020 | |||||||||
| 24 | 29 | 46. | (3 and 4) | |||||||||
| Bother | 25 | 22 | 22 | 0.020 | ||||||||
| 31 | 25 | 32 | (2 and 4) | |||||||||
| 36 | 25 | 42 | ||||||||||
| Arm/hand | 11 | 0.041 | 6 | 0.025 | 8 | 0.006 | ||||||
| 23 | (2 and 3) 0.032 | 21 | (2 and 3) 0.037 | 4 | (2 and 4) 0.004 | |||||||
| 24 | (2 and 4) | 18 | (2 and 4) | 40 | (3 and 4) | |||||||
| Mobility | 15 | 0.038 (2 and 3) | 24 | 0.041 (2 and 3) | 8 | 0.010 (2 and 3) | ||||||
| 28 | 0.035 (2 and 4) | 36 | 30 | 0.002 (2 and 4) | ||||||||
| 33 | 32 | 44 | 0.030 (3 and 4) | |||||||||
| Daily activity | 21 | 0.041 | 29 | 0.038 | 26 | 0.005 | ||||||
| 37 | (2 and 3) | 43 | (2 and 3) | 37 | (2 and 4) | |||||||
| 38 | 0.040 (2 and 4) | 27 | 0.040 (3 and 4) | 53 | 0.033 (3 and 4) | |||||||
| Emotional | 27 | 27 | 28 | 0.010 | ||||||||
| 34 | 0.042 | 34 | 0.042 | 37 | (2 and 4) | |||||||
| 44 | (2 and 4) | 44 | (2 and 4) | 49 | 0.032 (3 and 4) | |||||||
SMFA = Short Musculoskeletal Function Assessment.
Fig. 2.
Proximal humeral fractures with locked plating treatment Short Musculoskeletal Function assessment (SMFA) scores compared with the normative population as described by Hunsaker, et al. [32] demonstrates improvement, but sustained disability of indices.
Fig. 3.
Proximal humeral fractures with locked plating treatment 6-month Short Musculoskeletal Function Assessment (SMFA) scores were compared with regional musculoskeletal disorders. UE = upper extremity; LE = lower extremity; fx = fracture; LP = locked plating.
Table 5.
SF-36 scores at 6-, 12-, and 24-month intervals
| Interval | Physical functioning | Role–physical | Bodily pain | General health perceptions | Vitality | Social functioning | Role–emotional | Mental health |
|---|---|---|---|---|---|---|---|---|
| 6 months | 56 | 49 | 52 | 60 | 55 | 78 | 64 | 73 |
| 12 months | 49 | 39 | 51 | 62 | 50 | 73 | 52 | 70 |
| 24 months | 52 | 42 | 60 | 64 | 59 | 78 | 77 | 77 |
Polytrauma patients performed consistently worse in mobility and emotional outcome measurements than isolated fracture patients at each time interval (Table 6). Polytrauma patients had worse DASH scores (t = −2.296, p = 0.027) than those with isolated injuries at 24 months.
Table 6.
Average SMFA index scores for isolated injuries and polytrauma at 6-, 12-, and 24-month intervals
| 6 months | 12 months | 24 months | |||||||
|---|---|---|---|---|---|---|---|---|---|
| SMFA index | Isolated | Polytrauma | Significance | Isolated | Polytrauma | Significance | Isolated | Polytrauma | Significance |
| Dysfunction | 21 | 22 | 22 | ||||||
| 32 | 0.070 | 37 | 0.007 | 31 | |||||
| Bother | 25 | 16 | 22 | ||||||
| 35 | 33 | 0.006 | 34 | 0.043 | |||||
| Arm/hand | 17 | 15 | 14 | ||||||
| 20 | 19 | 16 | |||||||
| Mobility | 15 | 22 | 13 | ||||||
| 34 | 0.008 | 41 | 0.012 | 33 | 0.008 | ||||
| Daily activity | 26 | 37 | 31 | ||||||
| 36 | 39 | 35 | |||||||
| Emotional | 27 | 27 | 27 | ||||||
| 42 | 0.030 | 48 | < 0.001 | 40 | 0.031 | ||||
SMFA = Short Musculoskeletal Function Assessment.
Sixty-three (96%) returned to previous activities or occupation. Three patients (4%) experienced restrictions to activities or returned to a different occupation. These three patients experienced polytrauma as a result of a motor vehicle accident, had associated injuries, and three- or four-part fractures.
Discussion
In recent years, ORIF with locked plate technology for proximal humeral fractures has had increased indications and use. Complications remain for this treatment method, but the literature is sparse with studies evaluating functional outcome measurements with long-term followup, comparison of fracture pattern, and effect of associated injuries. Therefore, we determined whether age, time intervals after surgery up to 2 years, fracture pattern, and associated injuries affected prospectively obtained functional outcome measurements after locking plate treatment of unstable displaced proximal humeral fractures.
Our study is associated with a number of limitations. First, our patient population was obtained from a single trauma practice with a single treatment philosophy. This similar treatment regimen improves consistency but limits the generalizability of these data to other proximal humeral locked plating methods. Second, the combination of polytrauma and isolated proximal humeral injuries could bias the results and limit the numbers needed for statistical analysis. Further studies evaluating isolated injuries would diminish confounding variables but also select out only low-energy fall and exclude high-energy injuries. Third, this study did not compare or contrast results with a similar patient population treated with other options such as pinning, nonlocked plates, nails, or arthroplasty. It did select out the most difficult fracture patterns not amenable to other nonarthroplasty treatments. Comparative effectiveness of treatment options would be beneficial and prudent. Fourth, most studies evaluated outcome measurements of Constant-Murley, DASH, or SMFA separately at 1 year maximum and not a combination of scores up to 2 years postoperatively. One study combined the SMFA scores instead of reporting the indices’ subscores [46], thus it is not possible to compare our subscore data. However, we had prospectively obtained outcome measures from a consecutive series of patients. The outcome questionnaires were completed during the office visit. Having the questionnaire completed while in the office improves the return rate but could generate nonblinded [34] and responder bias [47]. Retrospective patient data collection and demographic evaluation have all the associated biases of retrospective studies. Further, we evaluated patients up to 2 years, which is more than the early time point of 1 year in most studies.
Proximal humeral fracture outcome measurements are becoming more evident but have primarily been reported using the Constant-Murley score. In a series of 176 proximal humeral fractures treated with a locking proximal humeral plate, Constant-Murley scores measured improved outcomes of 80% and 73% in patients older than 65 years old compared with patients younger than 65 years old [35]. In a series of 72 fractures treated with a locking proximal humeral plate, Bjorkenheim et al. noted the Constant-Murley score to be acceptable [8]. In a smaller series of 32 fractures treated with the Philos plate, Moonot et al. observed a mean Constant-Murley score of 66.5% with no difference in the older versus the younger patients [42]. In our study, the typical bimodal younger high-energy and older low-energy fractures were noted. Older patients had better outcome measurements than younger patients but similar DASH scores. With younger patients having more polytrauma and associated injuries, the DASH score, which evaluates upper extremity not general health scores, may be a more specific proximal humeral outcome measure. Our SF-36 outcome measurements were inversely related to our SMFA scores. As confirmed with the literature and our study, SF-36 and SMFA measurements for orthopaedic fractures results are highly inversely correlated [9] and redundant if performing both concurrently. Instead of performing both questionnaires, we recommend using an outcome measurement chosen to answer a specific clinical question [47]. Compared with other published data [42] older patient outcome measurements peak at 1 year and then decline minimally at the 2-year measurement. We cannot explain this decline, unless it somehow reflects a general decline in the older patients. In this study, younger compared with older patients continue to improve until the 2-year mark for dysfunction and arm/hand but not for bother. Bother and emotional scores for younger patients were worse than older patients at the 2-year interval.
Most studies evaluate the functional outcome at one time point, which was at 1 year or less [18, 29, 38, 40, 42, 46]. Laflamme et al. did determine improving DASH scores at each time interval until 1 year [40]. No evaluation past 1 year was recorded for any comparison purposes. The purpose of evaluating outcome measurements over time is to determine when the scores plateau and determine if the scores diminish with time. Clinically, this translates into determining a time when physical therapy should be stopped because further costly therapy would not be beneficial. Furthermore, determining a time when scores may diminish should effect minimal followup times to truly elucidate final results. In our study, SMFA outcome measurements of the arm/hand and bother improved with time. Standardization of musculoskeletal outcome measurements was created from a collection of population-based normative data [32]. At the 2-year interval, arm/hand and bother outcome measurements were more than twice as dysfunctional as normative data. When evaluating the bother and dysfunction index, proximal humeral fractures treated with locked plating performed similar to repetitive-motion disorder or osteoarthritis of the upper extremity but better than osteoarthritis of the lower extremity. Our data demonstrate persistent long-term deviation from normative data for all functional measurements. SF-36 scores improve with time also. Because DASH was only performed at the 2-year interval, a comparison with time could not be performed. With a DASH score of 31, continued disability was noted. Our 2-year average DASH score of 31 compared well with the only other recorded 1-year DASH score of 26 [40]. If the outcome measurements were obtained at earlier time intervals, further differences over time might have been measured. Proximal humeral fractures are debilitating injuries that require many months to years of formal and individual rehabilitation until reaching maximum functional potential.
Owsley and Gorczyca noted that worse fracture patterns had more complications with locked plating of proximal humeral fractures [46]. They indirectly noted that patients with more complications had worse outcome measurements at the 1-year interval. One may presume that worse fracture patterns have worse outcome measurements. The Neer fracture pattern affected arm/hand outcome measures at the 6-, 12-, and 24-month intervals. Worse fracture patterns had worse functional outcome measurements. Major differences in arm/hand measurements were noted among Neer two-, three-, and four-part fractures with corresponding dysfunction with more severe fracture pattern. Comparing the 2-year with the 1-year arm/hand measurements, the Neer four-part fractures might have had a decline in function secondary to the development of avascular necrosis and subsequent surgical revision to arthroplasty.
Isolated fractures in younger patients compared with older patients had similar outcome measurements. As expected, patients with polytrauma injury patterns consistently performed worse than patients with isolated fractures. Long-term dysfunction and bother persisted compared with normative data. At the 6-month time interval, isolated injuries had better dysfunction, mobility, and emotional outcome measurements. At the 1- and 2-year time intervals, isolated injuries had better bother, mobility, and emotional outcome measurements. The arm/hand and daily activity outcome measurements were similar in both groups. Patients with isolated injuries had better DASH scores than polytrauma patients. With sustained severe disability noted with younger polytrauma patients, vocational rehabilitation or retraining should begin early in the rehabilitation period. A majority of our patients, 96%, returned to a similar level of activities, functioning, and occupation. Having one-third of our patients retired and one-seventh unemployed could have skewed these results, although vocational retraining or worker’s compensation may benefit from delaying changes until further rehabilitation is attempted.
In our opinion, further outcome measurements utilizing a single standardized score or multiple outcome different measurements (DASH, Constant-Murley, ASES, and SMFA) would assist analysis of the growing literature on locked plating of proximal humeral fractures. Secondly, reporting data less than two years is incomplete and portrays an inaccurate final analysis of the treatment. Thirdly, comparative effectiveness studies evaluating cost and complication analysis with other treatment regimens is warranted.
Our data quantify and qualify the outcome measurements of proximal humeral fractures treated with a periarticular locked plate at a single trauma center. Older age, less complex fracture pattern, and isolated injuries resulted in improved functional outcome measurements. Compared with prior studies, outcome measurements were affected by fracture pattern and continued to improve up to 2 years postoperatively. All SMFA indices were worse than normative data. Younger polytrauma patients may benefit with early vocational retraining. Continued counseling and maintenance of a rehabilitation program over an extended period of time is needed to meet maximum functional potential.
Acknowledgments
We thank orthopaedic trauma surgeons, James R. Ringler, MD (JRR), and Terrence J. Endres, MD (TJE), for their surgical expertise, contribution of patients for this study, and encouragement for this study. Additionally, we thank Kevin D. Sietsema, BA, for his assistance in obtaining and calculating the functional outcome survey scores.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and an approval for informed consent for participation in the retrospective study was obtained.
References
- 1.Agel J, Jones CB, Sanzone AG, Camuso M, Henley MB. Treatment of proximal humeral fractures with Polarus nail fixation. J Shoulder Elbow Surg. 2004;13:191–195. doi: 10.1016/j.jse.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 2.Agudelo J, Schurmann M, Stahel P, Helwig P, Morgan SJ, Zechel W, Bahrs C, Parekh A, Ziran B, Williams A, Smith W. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007;21:676–681. doi: 10.1097/BOT.0b013e31815bb09d. [DOI] [PubMed] [Google Scholar]
- 3.Anglen J, Kyle RF, Marsh JL, Virkus WW, Watters WC, 3rd, Keith MW, Turkelson CM, Wies JL, Boyer KM. Locking plates for extremity fractures. J Am Acad Orthop Surg. 2009;17:465–472. doi: 10.5435/00124635-200907000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Baron JA, Barrett J, Malenka D, Fisher E, Kniffin W, Bubolz T, Tosteson T. Racial differences in fracture risk. Epidemiology. 1994;5:42–47. doi: 10.1097/00001648-199401000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Baron JA, Karagas M, Barrett J, Kniffin W, Malenka D, Mayor M, Keller RB. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7:612–618. doi: 10.1097/00001648-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Beaton DE, Katz JN, Fossel AH, Wright JG, TArasuk V, Bombardier C. Measureing the whole or the parts? Validity, reliability, and responsiveness of the disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14:128–146. [PubMed] [Google Scholar]
- 7.Bell JE, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC, Tosteson AN. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93:121–131. doi: 10.2106/JBJS.I.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bjorkenheim JM, Pajarinen J, Savolainen V. Internal fixation of proximal humeral fractures with a locking compression plate: A retrospective evaluation of 72 patients followed for a minimum of 1 year. Acta Orthop Scand. 2004;75:741–745. doi: 10.1080/00016470410004120. [DOI] [PubMed] [Google Scholar]
- 9.Busse JW, Bhandari M, Guyatt GH, Heels-Ansdell D, Mandel S, Sanders D, Schemitsch E, Swiontkowski M, Tornetta P, 3rd, WAi E, Walter SD. Use of both Short Musculoskeletal Function Assessment questionnaire and Short Form-36 among tibial fracture patients was redundant. J Clin Epidemiol. 2009;62:1210–1217. doi: 10.1016/j.jclinepi.2009.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charalambous CP, Siddique I, Valluripalli K, Kovacevic M, Panose P, Srinivasan M, Marynissen H. Proximal humeral internal locking system (PHILOS) for the treatment of proximal humeral fractures. Arch Orthop Trauma Surg. 2007;127:205–210. doi: 10.1007/s00402-006-0256-9. [DOI] [PubMed] [Google Scholar]
- 11.Cornell CN. Tension-band wiring supplemented by lag-screw fixation of proximal humerus fractures: a modified technique. Orthop Rev. 1994;Suppl:19–23. [PubMed]
- 12.Cornell CN, Levine D, Pagnani MJ. Internal fixation of proximal humerus fractures using the screw-tension band technique. J Orthop Trauma. 1994;8:23–27. doi: 10.1097/00005131-199402000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 14.Court-Brown CM, Garg A, McQueen MM. The translated two-part fracture of the proximal humerus. Epidemiology and outcome in the older pateint. J Bone Joint Surg Br. 2001;83:799–804. doi: 10.1302/0301-620X.83B6.11401. [DOI] [PubMed] [Google Scholar]
- 15.Darder A, Darder A, Jr, Sanchis V, Gastaldi E, Gomar F. Four-part displaced proximal humeral fractures: operative treatment using Kirschner wires and a tension band. J Orthop Trauma. 1993;7:497–505. doi: 10.1097/00005131-199312000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Esser RD. Open reduction and internal fixation of three- and four-part fractures of the proximal humerus. Clin Orthop Relat Res. 1994;299:244–251. [PubMed] [Google Scholar]
- 17.Esser RD. Treatment of three- and four-part fractures of the proximal humerus with a modified cloverleaf plate. J Orthop Trauma. 1994;8:15–22. doi: 10.1097/00005131-199402000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Fankhauser F, Boldin C, Schippinger G, Haunschmid C, Szyszkowitz R. A new locking plate for unstable fractures of the proximal humerus. Clin Orthop Relat Res. 2005;430:176–181. doi: 10.1097/01.blo.0000137554.91189.a9. [DOI] [PubMed] [Google Scholar]
- 19.Fenichel I, Oran A, Burstein G, Perry Pritsch M. Percutaneous pinning using threaded pins as a treatment option for unstable two- and three-part fractures of the proximal humerus; a retrospective study. Int Orthop. 2006;30:153–157. doi: 10.1007/s00264-005-0058-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Galatz LM, Iannotti JP. Management of surgical neck nonunions. Orthop Clin North Am. 2000;31:51–61. doi: 10.1016/S0030-5898(05)70127-9. [DOI] [PubMed] [Google Scholar]
- 21.Gardner MJ, Griffith MH, Dines JS, Briggs SM, Weiland AJ, Lorich DG. The extended anterolateral acromial approach allows minimally invasive access to the proximal humerus. Clin Orthop Relat Res. 2005;434:123–129. doi: 10.1097/01.blo.0000152872.95806.09. [DOI] [PubMed] [Google Scholar]
- 22.Gardner MJ, Lorich DG, Werner CM, Helfet DL. Second-generation concepts for locked plating of proximal humerus fractures. Am J Orthop. 2007;36:460–465. [PubMed] [Google Scholar]
- 23.Gardner MJ, Voos JE, Wanich T, Helfet DL, Lorich DG. Vascular implications of minimally invasive plating of proximal humerus fractures. J Orthop Trauma. 2006;20:602–607. doi: 10.1097/01.bot.0000246412.10176.14. [DOI] [PubMed] [Google Scholar]
- 24.Gibson JN, Handoll HH, Madhok R. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2001;1:CD000434. doi: 10.1002/14651858.CD000434. [DOI] [PubMed] [Google Scholar]
- 25.Gibson JN, Handoll HH, Madhok R. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2002;2:CD000434. doi: 10.1002/14651858.CD000434. [DOI] [PubMed] [Google Scholar]
- 26.Hawkins RJ, Switlyk P. Acute prosthetic replacement for severe fractures of the proximal humerus. Clin Orthop Relat Res. 1993;289:156–160. [PubMed] [Google Scholar]
- 27.Healy WL, Jupiter JB, Kristiansen TK, White RR. Nonunion of the proximal humerus. A review of 25 cases. J Orthop Trauma. 1990;4:424–431. [PubMed] [Google Scholar]
- 28.Helmy N, Hintermann B. New trends in the treatment of proximal humerus fractures. Clin Orthop Relat Res. 2006;442:100–108. doi: 10.1097/01.blo.0000194674.56764.c0. [DOI] [PubMed] [Google Scholar]
- 29.Hepp P, Theopold J, Voigt C, Engel T, Josten C, Lill H. The surgical approach for locking plate osteosynthesis of displaced proximal humeral fractures influences the functional outcome. J Shoulder Elbow Surg. 2008;17:21–28. doi: 10.1016/j.jse.2007.03.029. [DOI] [PubMed] [Google Scholar]
- 30.Hertel R. Fractures of the proximal humerus in osteoporotic bone. Osteoporos Int. 2005;16(Suppl 2):S65–S72. doi: 10.1007/s00198-004-1714-2. [DOI] [PubMed] [Google Scholar]
- 31.Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13:427–433. doi: 10.1016/j.jse.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 32.Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American Academy of Orthopaedic Surgeons outcomes instruments: Normative values from the general population. J Bone Joint Surg Am. 2002;84:208–215. doi: 10.2106/00004623-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Jakob RP, Miniaci A, Anson PS, Jaberg H, Osterwalder A, Ganz R. Four-part valgus impacted fractures of the proximal humerus. J Bone Joint Surg Br. 1991;73:295–298. doi: 10.1302/0301-620X.73B2.2005159. [DOI] [PubMed] [Google Scholar]
- 34.Karanicolas PJ, Bhandari M, Taromi B, Akl EA, Bassler D, Alonso-Coello P, Rigau D, Bryant D, Smith SE, Walter SD, Guyatt GH. Blinding of outcomes in trials of orthopaedic trauma: an opportunity to enhance the validity of clinical trials. J Bone Joint Surg Am. 2008;90:1026–1033. doi: 10.2106/JBJS.G.00963. [DOI] [PubMed] [Google Scholar]
- 35.Kettler M, Biberthaler P, Braunstein V, Zeiler C, Kroetz M, Mustschler W. Treatment of proximal humeral fractures with the PHILOS angular stable plate: Presentation of 225 cases of dislocated fractures [in German] Der Unfallchirurg. 2006;109:1032–1040. doi: 10.1007/s00113-006-1165-7. [DOI] [PubMed] [Google Scholar]
- 36.Khan AA, Khan SU, Hossain Z. Intrathoracic migration of a humeral orthopedic pin. J Cardiovasc Surg. 2003;44:275–277. [PubMed] [Google Scholar]
- 37.Kim KC, Rhee KJ, Shin HD. Tension band sutures using a washer for a proximal humerus fracture. J Trauma. 2008;64:1136–1138. doi: 10.1097/TA.0b013e318076b514. [DOI] [PubMed] [Google Scholar]
- 38.Koukakis A, Apostolou CD, Taneja T, Korres DS, Amini A. Fixation of proximal humerus fractures using the PHILOS plate: early experience. Clin Orthop Relat Res. 2006;442:115–120. doi: 10.1097/01.blo.0000194678.87258.6e. [DOI] [PubMed] [Google Scholar]
- 39.Kristiansen B, Christense SW. Plate fixation of proximal humeral fractures. Acta Orthop Scand. 1986;57:320–323. doi: 10.3109/17453678608994401. [DOI] [PubMed] [Google Scholar]
- 40.Laflamme GY, Rouleau DM, Berry GK, Beaumont PH, Reindl R, Harvey EJ. Percutaneous humeral plating of fractures of the proximal humerus: results of a prospective multicenter clinical trial. J Orthop Trauma. 2008;22:153–158. doi: 10.1097/BOT.0b013e3181694f7d. [DOI] [PubMed] [Google Scholar]
- 41.Lin J, Hou SM, Hang YS. Locked nailing for displaced surgical neck fractures of the humerus. J Trauma. 1998;45:1051–1057. doi: 10.1097/00005373-199812000-00013. [DOI] [PubMed] [Google Scholar]
- 42.Moonot P, Ashwood N, Hamlet M. Early results for treatment of three- and four-part fractures of the proximal humerus using the PHILOS plate system. J Bone Joint Surg Br. 2007;89:1206–1209. doi: 10.1302/0301-620X.89B9.18528. [DOI] [PubMed] [Google Scholar]
- 43.Neer CS., 2nd Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 44.Neer CS., 2nd Four-segment classification of proximal humeral fractures: purpose and reliable use. J Shoulder Elbow Surg. 2002;11:389–400. doi: 10.1067/mse.2002.124346. [DOI] [PubMed] [Google Scholar]
- 45.Neer CS., 2nd Displaced proximal humeral fractures: part I. Classification and evaluation. 1970. Clin Orthop Relat Res. 2006;442:77–82. doi: 10.1097/01.blo.0000198718.91223.ca. [DOI] [PubMed] [Google Scholar]
- 46.Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures. J Bone Joint Surg Am. 2008;90:233–240. doi: 10.2106/JBJS.F.01351. [DOI] [PubMed] [Google Scholar]
- 47.Poolman RW, Swiontkowski MF, Fairbank JC, Schemitsch EH, Sprague S, Vet HC. Outcome instruments: rationale for their use. J Bone Joint Surg Am. 2009;91(Suppl 3):41–49. doi: 10.2106/JBJS.H.01551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sharafeldin K, Wuinlan JF, Corrigan J, Kelly IP. Functional follow-up of locking plate fixation of fractures of the proximal humerus. Eur J Orthop Surg. 2008;18:87–92. doi: 10.1007/s00590-007-0266-5. [DOI] [Google Scholar]
- 49.Swiontkowski MF, Engelberg R, Martin DP, Agel J. Short Musculoskeletal Function Assessment questionnaire: Validity, reliability, and responsiveness. J Bone Joint Surg Am. 1999;81:1245–1260. doi: 10.1302/0301-620X.81B6.9794. [DOI] [PubMed] [Google Scholar]
- 50.Voigt C, Woltmann A, Partenheimer A, Lill H. Management of complications after angularly stable locking proximal humerus plate fixation [in German] Chirurg. 2007;78:40–46. doi: 10.1007/s00104-006-1241-0. [DOI] [PubMed] [Google Scholar]
- 51.Ware J, Kosinski M, Gandek B. SF-36 Health Survey: Manual & Interpretation Guide. Lincoln, RI: Quality Metric; 2000. [Google Scholar]
- 52.Zyto K, Wallace WA, Frostick SP, Preston BJ. Outcome after hemiarthroplasty for three- and four-part fractures of the proximal humerus. J Shoulder Elbow Surg. 1998;7:85–89. doi: 10.1016/S1058-2746(98)90215-4. [DOI] [PubMed] [Google Scholar]