Fractures of the pelvic ring comprise about 2% of all fractures, but the incidence is increasing due to increasing numbers of high-speed vehicular crashes and suicide attempts.1 Mortality associated with isolated pelvic injury, independent of severity, has been reported to be low: 1%–2%.2 Among multiply injured victims of blunt trauma, however, almost 20% have injuries to the pelvic ring.3,4,5 In this group, when closed pelvic ring disruption is associated with multiple injuries, the mortality rate rises to 10%–15%.6,7,8 Pelvic fractures associated with intra-cranial mass lesions or notable abdominal injuries have mortality rates as high as 50%.3 The mortality associated with open pelvic fractures has been shown to be 30%–50%.9,10 The parameters that predict mortality are age, injury severity score (ISS) and the existence of severe hemorrhage.11
Exsanguinating hemorrhage is the major cause of death in the first 24 hours after trauma.12,13,14,15,16 Immediate recognition of hemorrhagic shock and effective control of bleeding must be pivotal in every resuscitation effort. Appropriate recognition and management of serious pelvic fractures is also integral to resuscitative strategy. Management of these potentially lethal injuries requires expedited stabilization by a multidisciplinary team of trained personnel with a defined treatment protocol.
Multidisciplinary clinical-pathway and coordinated joint decision-making improves patient survival.17 A post mortem study by Wright and colleagues18 has shown that the average ISS of patients dying from pelvic fractures was much higher in patients treated by a protocol of care than in those treated with a “non-system” approach on an ad-hoc basis. As the understanding of these potentially fatal injuries improves, priorities of early management of pelvic ring injuries are evolving. This review article summarizes the current trend in emergent management of pelvic fractures, based on available evidence. A protocol designed to facilitate organized and systematic care of the serious pelvic fracture in multi-system trauma is proposed.
Advanced trauma life-support and the primary survey
Upon arrival in the emergency department, patients should be resuscitated according to the guidelines of the Advanced Trauma Life Support Course (ATLS) of the American College of Surgeons' Committee on Trauma.19 ATLS protocols are subject to periodic review and revision as new clinical and basic science data emerges. They are used worldwide for systematic management of multiply injured patients, and continue to be the most useful guidelines.
The primary survey emphasizes immediate assessment of the airway and breathing while maintaining spinal precautions. Attention is then focused on the cardiovascular system. Quickly identifying the site of hemorrhage in the hemodynamically unstable patient is both critical and time- dependant. Although volume resuscitation is generally begun after intravenous (IV) access has been established, it is only an adjunct to aggressive hemorrhage control.20,21 It is important to note that volume resuscitation without hemorrhage control is ineffective and may lead to secondary iatrogenic complications such as hypothermia and coagulopathy.
Hemorrhage control consists of stopping external bleeding by direct pressure and expeditiously determining whether surgery or other interventions are required for internal control of bleeding. If the patient shows signs of hypovolemia, a thorough and systematic search must be initiated to identify the source of bleeding. Plain radiographs of the chest (CXR) and pelvis are obtained at this stage. Optimally, this is followed by an evaluation for intra-abdominal bleeding, through either diagnostic peritoneal lavage (DPL) or, increasingly, a focused assessment with sonography for trauma (FAST) exam.22 We conceptualize this exam as a simple extension of the physical examination.23,24
Ideally, major blood losses into a hemothorax or the peritoneal cavity will thus be detected by either the CXR or the FAST. Retroperitoneal blood loss associated with a pelvic fracture will not be definitively detected through this algorithm, but can often be inferred when a severely displaced pelvic fracture is seen via x-rays and the chest radiograph and abdominal studies are reassuring.
Computed tomography (CT) is undeniably the most accurate means to identify peritoneal and especially retroperitoneal injuries, but the CT suite is an unsafe environment for the unstable trauma patient. An essential consideration in resuscitating these patients is thermal control, with a strict avoidance of early hypothermia, which exacerbates traumatic coagulopathies.25
Initial assessment of pelvic injury
The 2 most important factors that direct further management of pelvic injury are the patient's hemodynamic status and stability of the pelvic ring. Careful and thorough assessment of both parameters can be life-saving, and may direct systematic management priorities.
Hemodynamic status
Hypovolemia should be carefully evaluated and hemorrhagic shock diagnosed and graded promptly. Specific attention should be paid to assessing the pulse and respiratory rates and the state of skin circulation. Relying solely on systolic blood pressure may be misleading, as up to 30% of a patient's blood volume must be lost in order to incur hypotension. Tachycardia and cool peripheries are early indicators, and a narrowed pulse pressure may suggest significant blood loss. A very low hematocrit may also suggest massive blood loss, but normal hematocrit does not rule out shock. In young patients, estimations of arterial blood pressure, central venous pressure, hemoglobin and hematocrit have been shown to be unreliable markers of shock.26
A base deficit with metabolic acidosis, as estimated from arterial blood gas analysis, can be obtained quickly, which is useful in estimating the severity of shock and an important trend to follow.27,28 Ertel and associates29 have also emphasized lactate clearance as an accurate way to quantify both the degree of hemorrhagic shock and the probability of survival. Lactate levels are believed to better correlate with total oxygen debt, which ultimately depends on the magnitude of hypoperfusion and hemorrhagic shock.30,31 In the early resuscitative phase, clinical signs and symptoms, along with measurement of hourly urine output, continue to be the most practical indicators of systemic perfusion.
Fracture stability
If pelvic radiographs reveal obvious radiological instability of the ring, aggressive physical examination with compression and distraction will not provide additional information on injury severity, but rather could potentially cause further injury or aggravate bleeding. Recently, investigators such as Duane32 and Guillamondegui33 and their respective groups have questioned the need for routine pelvic radiographs in awake and alert patients, in whom clinical examination would be reliable. As in spinal fractures, however, many if not most severely injured patients have confounding factors such as head or neurologic injuries, intoxication, or other distracting injuries that make the physical examination unreliable.34,35,36 Thus, screening radiographs of the pelvis are recommended and continue to be an adjunct to resuscitation.
In hemodynamically unstable patients with no obvious site of hemorrhage, careful clinical examination of the pelvis is mandatory even when radiographs look normal or a pelvic image demonstrates a stable fracture configuration. A hurriedly taken anteroposterior view of the pelvis in the trauma room is often inadequate and may fail to reveal posterior injury of the pelvic ring. Physical examination of the pelvis should include thorough inspection of the flanks, lower abdomen, groin, perineum and buttocks to detect any wounds or bruises. The genitals and rectum should be inspected carefully to detect any blood at the urethral meatus or in the rectal vault, and to assess for a high-riding prostate. In the presence of signs suggestive of a genito-urinary injury, insertion of a urinary catheter should be avoided, and a retrograde urethrogram performed.
Orthopedic assessment should also note any clinical deformity of the pelvis, limb-length discrepancy or malrotation. The pelvis is tested for rotational instability with pelvic compression and distraction tests. A push–pull test, in which the examiner palpates both iliac crests while and an assistant provides telescoping forces to the ipsilateral lower limb, will help to find vertical instability.
In patients who are both hemodynamically and mechanically unstable, and in whom the major bleeding is thought to be related to the pelvic fracture, external stabilization of the pelvis becomes the first priority. Because the main sources of bleeding are most frequently the presacral venous plexus (80%)37,38 and fractured bony surfaces, external stabilization decreases the hemorrhage by reducing the volume of the pelvic basin and approximating the fracture ends.
Pneumatic antishock garments
The pneumatic antishock garment (PASG) or medical antishock trouser (MAST) can be helpful for immediate mechanical stabilization at an accident scene.39 “Prehospital” personnel can apply these garments promptly to facilitate transfer to the trauma centre.40 The PASG may provide an initial redistribution of blood from the limb to the trunk and restrict the expansion of a pelvic hematoma.41
In multiply injured patients with both blunt and penetrating trauma, however, randomized trials have not shown a survival benefit for use of the MAST garment.42,43,44 It is also unsuitable for long periods of application because of the risk of compartment syndrome.45,46 It impedes access to limbs and abdomen, making assessment of the patient in the emergency room more difficult. Currently, the role of PASG and MAST is limited.
Pelvic binders
Circumferential pelvic binders or sheets are gradually replacing anterior external fixation (AEF) as the method of choice of immediate external stabilization, and currently form part of the ATLS protocol.47 These binders are noninvasive, simple to apply, inexpensive and can be applied at a prehospital stage.
Biomechanical studies48 with pelvic sheets applied around the greater trochanters and tensioned to 180 N have demonstrated their effectiveness. It has been shown that simple application of this sling increases pelvic stability by 61% in response to rotational stress and 55%, flexion–extension. Although the same study48 found this method to be less rigid than AEF, it has nonetheless been shown to reduce unstable pelvic fractures radiologically and to improve patients' hemodynamic status.49
To perform this method of stabilization, either an ordinary broad sheet can be tied at the level of the greater trochanter, or a commercial pelvic binder can be used or a MAST. It must be positioned appropriately or be moveable when required, to provide access to the entire abdomen and groin.
Clinical judgement and reassessment are important in using these techniques. Potential complications include skin necrosis if left in place too long or applied too tightly. In lateral compression injuries with transforaminal sacral fractures, possible visceral or neural injury may occur if applied too vigorously.50 In vertically unstable pelvic fractures, a supracondylar skeletal traction pin should be introduced; note also that to bring the affected hemipelvis level before applying a pelvic binder, some 25–30 pounds (about 11–14 kg) of longitudinal traction is required.
At present, the only evidence available on the efficacy of pelvic binders is anecdotal. Nevertheless this safe, noninvasive method seems to be a logical first resuscitative step with a serious pelvic fracture, to provide early hemorrhage control before considering invasive methods.
Anterior external fixation
Immediate AEF of an unstable pelvic injury has been the mainstay of acute stabilization for the past few decades. Reimer and coworkers51 reduced mortality rates from 22% to 8% by adding acute AEF to their hospital resuscitation protocol. Based on their results, they concluded that skeletal stabilization of pelvic injury should be viewed as a part of resuscitation rather than reconstruction. Burgess and colleagues52 and others53,54 have also documented decreased transfusion needs and reduced mortality with the use of anterior external fixator. Subsequent investigators52,53,55,56,57,58 have also recommended immediate application of external fixation for hemodynamically unstable patients, and consider it a life-saving procedure.
Some investigators have advised53 prophylactic stabilization with anterior external fixator(s) in all patients demonstrating bony instability, as even those patients who are initially hemodynamically stable on presentation may decompensate later. The anterior fixator is thought to contribute to hemostasis by maintaining a reduced pelvic volume, allowing tamponade, and by decreasing bony motion at the fracture site, allowing clots to stabilize.59
The anterior pelvic frame can be applied in the trauma bay, intensive care unit (ICU) or operating room (OR) in around 20–30 minutes. Fixator pins can be placed percutaneously or with an open technique. There are 2 common sites of pelvic pin placement; in emergency situations the high route (directly between the 2 tables of the iliac crest) is preferable to the low route (the supra-acetabular area between the anterior inferior and the anterior superior iliac spine). Biomechanical studies60 have shown that the low pin location has greater rigidity and pull-out strength; but in the trauma bay, placement of pins in the low route without guidance by fluoroscopy can be dangerous and is not recommended. Injuries to the lateral cutaneous nerve of the thigh and intra-articular pin placement have been reported.55,60
In the high route, stab incisions for pin placement are made 1 finger-breadth behind the ASIS (Fig. 1). The natural overhang of the outer table of the iliac crest is taken into consideration; the drill guide has to be placed along the inner two-thirds of the crest. After opening the cortex of the ilium with the drill, a 5-mm threaded pin is directed toward the greater trochanter and inserted into the ilium. Two pins, placed in a converging manner, are usually used in each iliac crest and are connected by bars. Manual force is used to reduce the pelvic fracture before tightening of the bars, which are positioned to allow access to the abdomen and permit flexion of the hip.
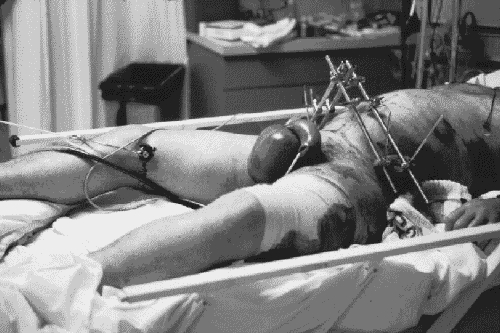
FIG. 1. Anterior fixator placed using the high route for pin placement, with 2 pins for each iliac crest.
The pelvic fractures most amenable to this form of treatment are the open book fracture, and the unstable shear type when combined with longitudinal traction. Lateral compression injuries incur fewer benefits from this method.55 AEF should be applied after discussion with the general surgical team, illustrating the importance of multidisciplinary communication. Its judicious use before laparotomy can both reduce further bleeding and prevent hypotension from decompression of the tamponade effect upon opening the abdominal wall. Ghanayem and associates61 have demonstrated in cadavers that the abdominal wall provides stability by means of a tension band effect, and that performing a laparotomy may further destabilize an open book pelvic injury and increase pelvic volume. The potential mechanical effects of leaving the abdominal fascia open after a laparotomy, as is commonly done in the “damage control” approach to intra-abdominal injury, remains unknown but is worthy of further study.
The application of AEF requires training and can be difficult to accomplish in the trauma room. It is hard to maintain a sterile environment, and contamination of the pin tracts can jeopardize definitive care of pelvic fractures. Pins can easily be misplaced, which could contribute to premature loosening and mechanical failure. Hospodar and coworkers62 have reported pin misplacement of up to 25% without use of fluoroscopy. Anterior external fixators can be difficult to apply in obese persons and can impede access to the abdomen and groin. And most importantly, AEF can aggravate the posterior instability in an unstable fracture configuration. Dickson and Matta63 have demonstrated worsening of posterior deformity in patients treated with AEF.
C–clamps
To deal with posteriorly unstable fractures, Ganz and coauthors64 developed a pelvic C-clamp, now available in most trauma units. It acts like a simple carpenter's clamp and can exert transverse compression directly across the sacroiliac joint. Experimental data64 have shown that an average compression force of 342 N can be applied to the area of this joint.
These clamps have been used therapeutically in hemodynamically unstable patients, and prophylactically in stable patients with unstable pelvic-ring disruptions. Hemodynamic status and fracture reduction have been shown to improve in both groups.64
Mechanically and technically, a posterior device is better than an anterior one.55,65 In experienced hands the posterior device is faster and safer to apply, and its position can be easily modified to allow access to the abdomen for the general surgeon.
The C-clamp is generally applied in the emergency department, if possible with the aid of an image intensifier. Witschger and colleagues66 have described the typical site for pin placement to be at the point of intersection of a line from the posterior to the anterior superior iliac spine, with the extension of the longitudinal axis of the dorsal border of the femur (Fig. 2). Once both pins are placed, the clamp is assembled and can be swivelled on its axis to permit access either to the legs or abdomen.

FIG. 2. Application of C-clamp with pins placed at line of intersection of a line from the posterior superior iliac spine to the anterior superior iliac spine with the extension of the longitudinal axis of the dorsal border of the femur.
C-clamp application can not only be difficult but dangerous in cases of comminuted sacral fractures: neurovascular injury can occur due to crushing of the sacrum. Agneu and associates67 have reported pelvic penetration of the stabilizing pins and overcompression of the clamps. The prongs of the C-clamp can be misapplied and have been accidentally placed into the true pelvis through the greater sciatic notch.
Two types of pelvic clamps are available. Schutz and coworkers68 compared use of the AO and ACE (Depuy International, Leeds, UK) pelvic clamps in 9 cases of posterior injuries to the pelvis, achieving satisfactory primary compression and stability in all cases with either clamp, but found the ACE clamp to be less stable rotationally due to its design.
Although potentially life-saving, these devices should be applied by an experienced surgeon, and considered only in cases of posteriorly unstable pelvic fractures accompanied by hemodynamic instability.
Acute fracture fixation
Provisional fixation of unstable pelvic-ring disruptions with a pelvic clamp or an external frame with a supracondylar pin has proved markedly beneficial in the resuscitative phase of management. If the patient is too ill to allow a more invasive intervention, traction pins can remain in place with the external frame as definitive treatment. If, however, the patient undergoes a laparotomy to deal with visceral injuries, symphyseal disruption and medial ramus fractures should be plated at the same time. Because neither blood loss nor operative time are greatly increased, combining these repairs decreases the risk of complications in a patient who is already compromised.69
A role has been suggested for percutaneous fixation; however, only surgeons appropriately trained should use this technique. Open surgery provides the opportunity for direct visualization, but is often put off for several days to allow maturation of the pelvic hematoma: acute entrance may disrupt early tamponade.70
Percutaneous pelvic fixation techniques allow for acute and definitive treatment of anterior and posterior pelvic ring injuries, without extensive dissection. Their success relies on accurate closed reduction, excellent intraoperative imaging and correct patient selection.
Accurate early pelvic stabilization diminishes pain and hemorrhage, provides better patient nursing and comfort, and allows early mobilization. Fixation can be performed acutely, even as a component of the patient's resuscitation. Early intervention improves the likelihood of a closed reduction, since the pelvic hematoma is compliant. Operative blood loss is minimal and wound complications are unusual.
Minimally invasive anterior ring fixation includes external fixation with retrograde or anterograde screws in the medulla of the superior ramus. Closed reduction and fixation with percutaneuous sacroiliac screws offers definitive stable fixation for many posterior pelvic ring injuries, such as fracture / dislocation of the sacroiliac joint or sacral fractures, with the advantage of minimal dissection and a reduction in wound complications.71,72
Angiography
Interventional angiographic procedures are increasingly being used as adjuncts to hemorrhage control in cases of solid-organ trauma.73,74,75 As experience and familiarity increases, many patients are having interventional radiological procedures instead of formal surgical intervention.73,76 Similarly, the role of pelvic angiography is evolving in a selected group of patients with pelvic fractures.
Although the source of bleeding is non-arterial in most cases, arterial injury can account for hemodynamic instability in 10%–20% of patients.77,78 Various arteries that cross the pelvis, including the internal iliac, obturator, superior gluteal and pudendal arteries, have been found to be the cause of bleeding in these fractures.79 Patients who remain hemodynamically labile after external stabilization and other resuscitative measures but have no major intraperitoneal bleeding are potential candidates for pelvic angiography. Eastridge and coauthors80 reported a 60% mortality rate in patients with unstable pelvic fractures who underwent laparotomy before angiography, and suggested that angiography should be considered before laparotomy and packing. Agolini and associates,81 in a large series of 806 patients, reported on 35 who underwent pelvic angiography: 15 of the 35 required embolization, which was successful in all cases. Cook's group82 reported a 15% rate of angiography in a series of 150 patients with unstable pelvic fractures. They concluded that the morphology of the fracture was unreliable as a guide to the associated vascular injury.
Other indications for pelvic angiography include the incidental discovery of an arterial “blush” in a contrast CT scan in an apparently stable patient, and as a last-ditch effort in thermally stable patients who remain in shock after exploratory laparotomy and surgical control of all other sources of bleeding. Overall requirements for angiography have been shown to be between 5% and 15%.83,84,85
The > 40% mortality rate reported in these patients indicates the relatively severe nature of the injury and its associated poor prognosis. Open surgical exploration of arterial bleeding is not recommended: access to the iliac arteries is difficult to gain, and disruption of the pelvic hematoma and consequential loss of tamponade effect can produce massive, uncontrollable and often fatal bleeding.86,87 Pelvic angiography is typically performed in a designated suite by a trained interventional radiologist, although the resuscitative suite of the future is likely to have both operative and interventional radiological capabilities. Sites of extravasation of arterial contrast are identified and selectively cannulated with Gelfoam or stainless steel coils.82
In practice, angiography has some drawbacks. It is time-consuming and currently requires transfer of a severely injured, unstable patient to the angiography suite, which may hamper resuscitative efforts. It also requires the availability of a skilled radiologist. When anatomical studies suggest the main source of hemorrhage to be non-arterial, the expected yield of angiography is low.81
Nevertheless, numerous investigators have reported the benefits of angiography in selected cases. We believe that pelvic angiography remains an important option in management of these life-threatening injuries, and can be diagnostic as well as therapeutic in patients in shock with no obvious cause of hemorrhage. In trained hands, angiography has been shown to be a safe procedure.88
Pelvic packing
Patients who remain in extremis with a probable retroperitoneal cause in spite of aggressive resuscitative efforts should not be transported to a distant angiography suite, especially if delay is involved.77 These are often patients at risk for abdominal compartment syndrome, and who therefore need an open peritoneal cavity for adequate cardiovascular physiologic support after surgery.
Such patients undergoing laparotomy for an identifiable intraperitoneal cause of hemorrhage should be assessed for an expanding pelvic hematoma. The true pelvis should be packed at that time if the hematoma has ruptured; the pelvic hematoma is otherwise not opened routinely. The true pelvis should be packed with large abdominal swabs and the wound closed over the packs to create tamponade. The packs are removed or changed in a second procedure at 24–48 hours.
The efficacy of pelvic packing to achieve hemostasis after hepatic, colorectal and gynecologic surgery is well documented.89,90,91 This approach is practised in some European trauma centres. Ertel29 and Pohlemann92 and their respective groups have shown promising results with laparotomy and packing prior to considering pelvic angiography; however, all their patients were either in extremis or in severe shock at presentation. This technique seems particularly applicable to patients with multiple hemorrhagic sources, both intra- and retroperitoneal, whose visceral injuries mandated a laparotomy as the first operative resuscitative measure.
The rationale behind pelvic packing derives from the fact that the major source of hemorrhage from pelvic ring injury is venous. Ertel's group29 reported success in controlling both arterial and venous bleeding by tightly packing the pelvis. Although pelvic packing has not often been used in North America, we feel it should be considered when patients are in ongoing shock but clinical and radiological features of arterial injury, such as an expanding groin hematoma or a fracture traversing the greater sciatic notch, are absent.
Open fractures
Potentially lethal injuries with a reported mortality rate of 30%–50%,93 open fractures of the pelvis by definition communicate with the rectum, the vagina, or the outside environment by disruption of the skin. They are often associated with disruption of the pelvic floor, leading to loss of tamponade and persistent bleeding. Clinical suspicion of an open fracture and any rectal or vaginal bleeding mandate a thorough examination, proctoscopic, sigmoidoscopic or by speculum.
Classically, an open pelvic fracture prompts recommendations for colostomy to prevent soft-tissue sepsis in an expanded perineum.94,95,96 It has recently been suggested97 that fecal diversion in an open pelvic fractures can be applied selectively, according to the actual location of the cutaneous wound. In the experience of Pell and coauthors,98 anterior wounds of the groin, anterior thigh, iliac crest or pubis do not require diversion.
In addition to hemorrhage control and stabilization of the pelvic ring, meticulous debridement of the wound and administration of broad-spectrum antibiotics are required. In open pelvic fractures with continuing hemorrhage, packing can be life-saving. These patients need careful ICU monitoring of hemodynamic and wound status, and may need serial and radical debridement along with changes of packs every 24–48 hours (packs left > 48 h may themselves potentiate pelvic sepsis).8 If bleeding recurs upon pack removal, the pelvis should be repacked.
In conclusion, lack of consensus persists among trauma surgeons on a standardized sequence of resuscitative steps for serious pelvic fractures. European centres generally prefer the more radical approach of laparotomy and direct packing, whereas North American centres rely more on angiographic embolization. Exploration of these issues is hindered by the extreme complexity of the patients and the limited numbers seen by any one centre. The complementary roles of newer hemostatic adjuncts such as recombinant factor VII also deserve further study.99,100 A system of care with a mutually agreed-upon protocol would reduce confusion and expedite resuscitation, which would certainly improve outcomes in these severely injured patients.
Competing interests: Drs. Kortbeek and Kirkpatrick serve on a Trauma Advisory Board for Novo Nordisk (makers of Factor VIIa), for which they have received compensation.
Correspondence to: Dr. Andrew W. Kirkpatrick, Department of Surgery, Foothills Medical Centre, 1403–29th St. NW, Calgary AB T2N 2T9; fax 403 944-1277; andrew.kirkpatrick@calgaryhealthregion.ca
Accepted for publication May 28, 2004
References
- 1.Pohlemann T. Pelvic ring injuries: assessment and concepts of surgical management. Chapter 4.4 in: Rüedi TP, Murphy WM, eds. AO principles of fracture management. Stuttgart (Germany): Thieme Publishing Group; 2000. p. 391–413.
- 2.Poole GV, Ward EF. Causes of mortality in patients with pelvic fractures. Orthopædics 1994; 17:691-6. [DOI] [PubMed]
- 3.McMurtry RY, Walton D, Dickinson D, Kellam J, Tile M. Pelvic disruption in the polytraumatized patient: a management protocol. Clin Orthop 1980;(151):22-30. [PubMed]
- 4.Pennal CF, Sutherland GO. Fractures of the pelvis [motion picture]. Park Ridge (IL): American Academy of Orthopædic Surgeons film library; 1981.
- 5.Gertzbein SD, Chenoweth DR. Occult injuries of the pelvic ring. Clin Orthop 1977; (128):202-7. [PubMed]
- 6.Heini PF, Witt J, Ganz R. The pelvic C-clamp for the emergency treatment of unstable pelvic ring injuries: a report on clinical experience of 30 cases. Injury 1996;27:S-A38–45. [DOI] [PubMed]
- 7.Witschger P, Heini PF, Ganz R. [Pelvic clamps for controlling shock in posterior pelvic ring injuries application, biomechanical aspects and initial clinical results.] Orthopade 1992;21:393-9. [PubMed]
- 8.Tile M. Fractures of the pelvis and acetabulum. Baltimore (MD): Williams & Wilkins; 1984.
- 9.Perry JF Jr. Pelvic open fractures. Clin Orthop 1980;(151):41-5. [PubMed]
- 10.Hanson PB, Milne JC, Chapman MW. Open fractures of the pelvis. J Bone Joint Surg Br 1991;73B:325-9. [DOI] [PubMed]
- 11.Ertel W. Therapeutic strategies and outcome of polytraumatized patients with pelvic injuries: a six year experience. Eur J Trauma 2000;6:278.
- 12.Gilliland MD, Ward RE, Burton RM, Miller PW, Duke JH. Fractures affecting mortality in pelvic fractures. J Trauma 1982;22:691-3. [DOI] [PubMed]
- 13.Paterson FP, Morton KS. The cause of death in fractures of the pelvis. J Trauma 1973;13:849-56. [PubMed]
- 14.Rothenberger DA, Fischer RP, Strate RG, Velasco R, Perry JF Jr. The mortality associated with pelvic fractures. Surgery 1978;84:356-61. [PubMed]
- 15.Sevitt S. Fatal road accidents: injuries, complications and causes of death in 257 subjects. Br J Surg 1968;55:481-505. [DOI] [PubMed]
- 16.Routt ML Jr, Simonian PT, Ballmer F. A rational approach to pelvic trauma: resuscitation and early definitive stabilization. Clin Orthop 1995;(318):61-73. [PubMed]
- 17.Biffl WL, Smith WR, Moore EE, Gonzalez RJ, Morgan SJ, Hennessey T, et al. Evolution of a multidisciplinary clinical pathway for the management of unstable patients with pelvic fractures. Ann Surg 2001;233(6):843-50. [DOI] [PMC free article] [PubMed]
- 18.Wright CS, McMurtry RY, Pickard J. A postmortem review of trauma mortalities — a comparative study. J Trauma 1984; 24: 67-8. [DOI] [PubMed]
- 19.American College of Surgeons. Advanced Trauma Life Support. 6th ed. Chicago (IL): the College; 1997.
- 20.Bickell WH, Wall MJ, Pepe PE, Martin RR, Ginger VF, Allen MK, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med 1994;331: 1105-9. [DOI] [PubMed]
- 21.Baron BJ, Scalea TM. Acute blood loss. Emerg Med Clin N Am 1996;14:35-55. [DOI] [PubMed]
- 22.Boulanger BR, Kearney PA, Brenneman FD, Tsuei B, Ochoa J. FAST utilization in 1999: results of a survey of North American trauma centers. Am Surg 2000;66:1049-55. [PubMed]
- 23.Kirkpatrick AW, Simons RK, Brown DR, Ng AKT, Nicolaou S. Digital hand-held sonography utilized for the focused assessment with sonography for trauma: a pilot study. Ann Acad Med Singapore 2001;30:577-81. [PubMed]
- 24.Kirpatrick AW, Simons RK, Brown DR, Nicolaou S, Dulchavsky S. The hand-held FAST: experience with hand-held trauma sonography in a level-1 urban trauma center. Injury 2002;33:303-8. [DOI] [PubMed]
- 25.Kirkpatrick AW, Chun R, Brown R, Simons RK. Hypothermia and the trauma patient. Can J Surg 1999;42:33-43. [PMC free article] [PubMed]
- 26.Collicott PE, Hughes I. Training in advanced trauma life support. JAMA 1980;243:1156-9. [PubMed]
- 27.Davis JW. The relationship of base deficit to lactate in porcine hemorrhagic shock and resuscitation. J Trauma 1994;36:168-72. [DOI] [PubMed]
- 28.Davis JW, Shackford SR, Mackersie RC, Hoyt DB. Base deficit as a guide to volume resuscitation. J Trauma 1988;28(10):1464-7. [DOI] [PubMed]
- 29.Ertel W, Keel M, Eid K, Platz A, Trentz O. Control of severe hemorrhage using C-clamp and pelvic packing in multiply injured patients with pelvic ring disruption. J Orthop Trauma 2001;15(7):468-74. [DOI] [PubMed]
- 30.Abramson D, Scalea DM, Hitchcock R, Trooskin SZ, Henry SM, Greenspan J. Lactate clearance and survival following injury. J Trauma 1993;35:584-8, discussion 588-9. [DOI] [PubMed]
- 31.Mizock BA, Falk JA. Lactic acidosis in critical illness. Crit Care Med 1992;20:80-93. [DOI] [PubMed]
- 32.Duane TM, Tan BB, Golay D, Cole FJ Jr, Weireter LJ Jr, Britt LD. Blunt trauma and the role of routine pelvic radiographs: a prospective analysis. J Trauma 2002;53(3):463-8. [DOI] [PubMed]
- 33.Guillamondegui OD, Pryor JP, Gracias VH, Gupta R, Reilly PM, Schwab CW. Pelvic radiography in blunt trauma resuscitation: a diminishing role. J Trauma 2002;53(6):1043-7. [DOI] [PubMed]
- 34.American College of Surgeons. Advanced Trauma Life Support course for doctors. Instructors course manual. Chicago (IL): the College; 1997.
- 35.Kirkpatrick AW, McKevitt EC. Thoracolumbar spine fractures: Is there a problem? Can J Surg 2002;45:21-4. [PMC free article] [PubMed]
- 36.Meek S. Fracture of the thoracolumbar spine in major trauma patients. BMJ 1999;317:1442-3. [DOI] [PMC free article] [PubMed]
- 37.Heini PF, Witt J, Ganz R. The pelvic C-clamp for the emergency treatment for the unstable pelvic ring injuries: a report on clinical experience of 30 cases. Injury 1996;27(Suppl 1):S-A38–45. [DOI] [PubMed]
- 38.Huittinen VM, Slatis P. Post-mortem angiography and dissection of the hypogastric artery in pelvic fractures. Surgery 1973;73:454-62. [PubMed]
- 39.Batalden DJ, Wickstrom PH, Ruiz E. Value of the G suit in patients with severe pelvic fractures: controlling hemorrhagic shock. Arch Surg 1974;109:326-8. [DOI] [PubMed]
- 40.American College of Surgeons. Advanced Trauma Life Support manual. Chicago (Ill.): the College; 1989.
- 41.McSwain NE. Pneumatic anti-shock garment: state of the art 1988. Ann Emerg Med 1988;17:506-25. [DOI] [PubMed]
- 42.Mattox KL, Bickell WH, Pepe PE, Mangelsdorff AD. Prospective randomized evaluation of antishock MAST in post-traumatic hypotension. J Trauma 1986;26:779-86. [DOI] [PubMed]
- 43.Bickell WH, Pepe PE, Bailey ML, Wyatt CH, Mattox KL. Randomized trial of pneumatic antishock garments in the prehospital management of penetrating abdominal injuries. Ann Emerg Med 1987;16:653-8. [DOI] [PubMed]
- 44.Mattox KL, Bickell W, Pepe PE, Burch J, Feliciano D. Prospective MAST study in 911 patients. J Trauma 1989;29:1104-12. [DOI] [PubMed]
- 45.Aprahamian C, Gessert G, Bandyk D, Sell L, Stiehl J, Olson DW. MAST associated compartment syndrome (MACS): a review. J Trauma 1989;29:549-55. [DOI] [PubMed]
- 46.Christensen KS. Pneumatique antishock garment (PASG): Do they precipitate lower extremity compartment syndromes? J Trauma 1986;26:549-55. [DOI] [PubMed]
- 47.American College of Surgeons. Advanced Trauma Life Support for Doctors. Instructor Course Manual. Chicago (IL): the College; 1997. p. 206-9.
- 48.Bottlang M, Krieg JC, Mohr M, Simpson TS, Madey SM. Emergent management of pelvic ring fractures with use of circumferencial compression. J Bone Joint Surg Am 2002;84(Suppl 2):43-7. [DOI] [PubMed]
- 49.Simpson T, Krieg JC, Heuer F, Bottlang M. Stabilization of pelvic ring disruptions with a circumferencial sheet. J Trauma 2002;52:158-61. [DOI] [PubMed]
- 50.Routt ML Jr, Falicov A, Woodhouse E, Schildhauer TA. Circumferencial pelvic antishock sheeting: a temporary resuscitation aid. J Orthop Trauma 2002;16(1):45-8. [DOI] [PubMed]
- 51.Reimer BL, Butterfield SL, Diamond DL, Young JC, Raves JJ, Cottington E, et al. Acute mortality associated with injuries to the pelvic ring: the role of early patient mobilization and external fixation. J Trauma 1993;35:671-7. [DOI] [PubMed]
- 52.Burgess AR, Eastridge BJ, Young JW, Ellison TS, Ellison PS Jr, Poka A, et al. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma 1990;30:845-56. [PubMed]
- 53.Poka A, Libby E. Indications and techniques for external fixation of the pelvis. Clin Orthop 1996;(329):54-9. [DOI] [PubMed]
- 54.Gylling SF, Ward RE, Holcroft JW, Bray TJ, Chapman MW. Immediate external fixation of unstable pelvic fractures. Am J Surg 1985;150(6):721-4. [DOI] [PubMed]
- 55.Kellam JF. The role of external fixation in pelvic disruptions. Clin Orthop 1989; (241) : 66-82. [PubMed]
- 56.Slatis P, Karaharju EO. External fixation of unstable pelvic fractures: experience in 22 patients treated with trapezoid compression frame. Clin Orthop 1980;(151): 73-80. [PubMed]
- 57.Trafton PG. Pelvic ring injuries. Surg Clin North Am 1990;70:655-69. [DOI] [PubMed]
- 58.Wild JJ Jr, Hansen JW, Tullos HS. Unstable fractures of the pelvis treated by external fixation. J Bone Joint Surg Am 1982;64:1010-20. [PubMed]
- 59.Mears DC. Clinical techniques in the pelvis. In: Mears DC, editor. External skeletal fixation. Baltimore (MD): Williams and Wilkins; 1983. p. 342.
- 60.Kim WY, Hearn TC, Seleem O, Mahalingam E, Stephen D, Tile M. Effect of pin location on stability of pelvic external fixation. Clin Orthop 1999;(361):237-44. [DOI] [PubMed]
- 61.Ghanayem AJ, Stover MD, Goldstein JA, Bellon E, Wilber JH. Emergent treatment of pelvic fractures. Comparison of methods for stabilization. Clin Orthop 1995;(318):75-80. [PubMed]
- 62.Hospodar P, Ulh R, Traub JA, Keller GS. Effect of fluoroscopy on accuracy of pelvic external fixator pin placement [poster 82]. Orthopædic Trauma Association meeting; 1999 Oct 22–24; Charlotte, NC.
- 63.Dickson KF, Matta JM. Skeletal deformity following external fixation of the pelvis [paper]. American Academy of Orthopædic Surgeons Annual Meeting; 1998 Mar 19–23; New Orleans, La.
- 64.Ganz R, Krushell AJ, Jakob RP, Kuffer J. The antishock pelvic clamp. Clin Orthop 1991;(267):71-8. [PubMed]
- 65.Egbers HJ, Draijr F, Habemann D, Zenker W. [Stabilizing the pelvic ring with the external fixator: biomechanical studies and clinical experience.] Orthopade 1992;6:363-72. [PubMed]
- 66.Witschger P, Heini P, Ganz R. [Pelvic clamps for controlling shock in posterior pelvic ring injuries: application, biomechanical aspects and initial clinical results.] Orthopade 1992;21:393-9. [PubMed]
- 67.Agnew SG, Agel J, Chip Routt ML Jr, et al. Preliminary experience with the anti-shock pelvic clamp: complications and early outcomes [poster]. Orthopædic Trauma Association meeting; 1996 Sep 26–29; Boston, Mass.
- 68.Schutz M, Stockle R, Hoffmann R, Sudkamp N, Haas N. Clinical experience with two types of pelvic C-clamps for unstable pelvic ring injuries. Injury 1996; 27 (Suppl 1);S-A46–50. [PubMed]
- 69.Tile M. Acute pelvic fractures: II. Principles of management. J Am Acad Orthop Surg 1996;4(3):152-61. [DOI] [PubMed]
- 70.Ghanayem AJ, Wilber JH, Lieberman JM, Motta AO. The effect of laparotomy and external fixator stabilization on pelvic volume in an unstable pelvic injury. J Trauma 1995;38:396-401. [DOI] [PubMed]
- 71.Barei DP, Bellabarba C, Mills WJ, Routt ML Jr. Percutaneous management of unstable pelvic ring disruptions. Injury 2001; 32 (Suppl 1):S-A33–44. [DOI] [PubMed]
- 72.Rout ML Jr, Nork SE, Mills WJ. High-energy pelvic ring disruptions. Orthop Clin North Am 2002;33(1):59-72. [DOI] [PubMed]
- 73.Kushimoto S, Arai M, Aiboshi J, Harada N, Tosaka N, Koido Y, et al. The role of interventional radiology in patients requiring damage control surgery. J Trauma 2003;54:171-6. [DOI] [PubMed]
- 74.Johnson JW, Gracias VH, Gupta R, Guillamondegui O, Reilly PM, Shapiro MB, et al. Hepatic angiography in patients undergoing damage control laparotomy. J Trauma 2002;52:1102-6. [DOI] [PubMed]
- 75.Haan J, Scott J, Boyd-Kranis RL, Ho S, Kramer M, Scalea TM. Admission angiography for blunt splenic injury: advantages and pitfalls. J Trauma 2001;51:1161-5. [DOI] [PubMed]
- 76.Kos X, Franchamps JM, Trotteur G, Dondelinger RF. Radiologic damage control: evaluation of a combined CT and angiography suite with a pivoting table. Cardiovasc Intervent Radiol 1999;22:124-9. [DOI] [PubMed]
- 77.Gansslen A, Giannoudis P, Pape HC. Hemorrhage in pelvic fractures: Who needs angiography? Curr Opin Crit Care 2003;9:515-23. [DOI] [PubMed]
- 78.Huittinen VM, Slatis P. Postmortem angiography and dissection of the hypogastric artery in pelvic fractures. Surgery 1973; 73:454-62. [PubMed]
- 79.O'Neill PA, Riina J, Sclafani S, Tornetta P 3rd. Angiographic findings in pelvic fracture. Clin Orthop 1996;(329):60-7. [DOI] [PubMed]
- 80.Eastridge BJ, Starr A, Minei JP, O'Keefe GE, Scalea TM. The importance of fracture pattern in guiding therapeutic decision- making in patients with hemorrhagic shock and pelvic ring disruptions. J Trauma 2002;53(3):446-50. [DOI] [PubMed]
- 81.Agolini SF, Shah K, Jaffe J, Newcomb J, Rhodes M, Reed JF 3rd. Arterial embolization is a rapid and effective technique for controlling pelvic fracture hemorrhage. J Trauma 1997;43(3):395-9. [DOI] [PubMed]
- 82.Cook RE, Keating JF, Gillespie I. The role of angiography in the management of hemorrhage from major fractures of the pelvis. J Bone Joint Surg Br 2002;84(2):178-82. [DOI] [PubMed]
- 83.Gilliland MG, Ward RE, Flynn TC, Miller PW, Ben-Menachem Y, Duke JH Jr. Peritoneal lavage and angiography in the management of patients with pelvic fractures. Am J Surg 1992;144:744-7. [DOI] [PubMed]
- 84.Moreno C, Moore EE, Rosenberger A, Cleveland HC. Hemorrhage associated with major pelvic fracture: a multidisciplinary challenge. J Trauma 1996;26: 987-94. [DOI] [PubMed]
- 85.Evers BM, Cryer HM, Miller FB. Pelvic fracture hemorrhage: priorities in management. Arch Surg 1989;124:422-4. [DOI] [PubMed]
- 86.Panetta T, Sclafani SJ, Goldstein AS, Phillips TF, Shaftan GW. Percutaneous transcatheter embolization for massive bleeding from pelvic fractures. J Trauma 1985;25:1021-9. [PubMed]
- 87.Ben-Menachem Y, Coldwell DM, Young JW, Burgess AR. Hemorrhage associated with pelvic fractures: causes, diagnosis and emergent management. AJR Am J Rœntgenol 1991;157(5):1005-14. [DOI] [PubMed]
- 88.Velmahos GC, Toutouzas KG, Vassiliu P, Sarkisyan G, Chan LS, Hanks SH, et al. A prospective study on the safety and efficacy of angiographic embolization for pelvic and visceral injuries. J Trauma 2002;52(2):303-8. [DOI] [PubMed]
- 89.Shen GK, Rappaport W. Control of nonhepatic intra-abdominal hemorrhage with temporary packing. Surg Gynecol Obstet 1992;174:411-3. [PubMed]
- 90.Zama N, Fazio V, Jagelman DG, Lavery IC, Weakley FL, Church JM. Efficacy of pelvic packing in maintaining hemostasis after rectal excision of cancer. Dis Colon Rectum 1998;31(12):923-8. [DOI] [PubMed]
- 91.Finan MA, Fiorica JV, Hoffman MS, Barton DP, Gleeson N, Roberts WS, et al. Massive pelvic hemorrhagic during gynecologic cancer surgery: “pack and go back.” Gynecol Oncol 1996;62:390-5. [DOI] [PubMed]
- 92.Pohlemann T, Bosch U, Gansslen A, Tscherne H. The Hannover experience in management of pelvic fractures. Clin Orthop 1994;(305):69-80. [PubMed]
- 93.Jones AL, Powell JN, Kellam JF, McCormack RG, Dust W, Wimmer P. Open pelvic fractures: a multicenter retrospective analysis. Orthop Clin North Am 1997;28(3):345-50. [DOI] [PubMed]
- 94.Poole GV. Pelvic fractures. In: Cameron JL, editor. Current surgical therapy. 6th ed. St. Louis (MO): Mosby; 1998. p. 979-83.
- 95.Kusmisky RE, Shbeeb I, Makos G, Boland JP. Blunt pelviperineal injuries: an expanded role for the diverting colostomy. Dis Colon Rectum 1982;25:787-90. [DOI] [PubMed]
- 96.Davidson BS, Simmons GT, Williamson PR, Buerk CA. Pelvic fractures associated with open perineal wounds: a survivable injury. J Trauma 1993;35:36-9. [DOI] [PubMed]
- 97.Faringer PD, Mullins RJ, Feliciano PD, Duwelius PJ, Trunkey DD. Selective fecal diversion in complex open pelvic fractures from blunt trauma. Arch Surg 1994;129:958-63. [DOI] [PubMed]
- 98.Pell M, Flynn WJ, Seibel RW. Is colostomy always necessary in the treatment of open pelvic fractures? J Trauma 1998;45:371-3. [DOI] [PubMed]
- 99.Allen GA, Hoffman M, Roberts HR, Monroe DM 3rd. Recombinant activated factor VII: its mechanism of action and role in the control of hemorrhage. Can J Anæsth 2002;49:S7-14. [PubMed]
- 100.Martinowitz U, Kenet G, Segal E, Luboshitz J, Lubetsky A, Ingersley J, et al. Recombinant activated factor VII for adjunctive hemorrhage control in trauma. J Trauma 2001;51:431-9. [DOI] [PubMed]


