Abstract
Total hip arthroplasty (THA) with conventional polyethylene bearings is traditionally the standard operative treatment for endstage arthritis of the hip. This design has excellent survivorship in most populations, with a low occurrence of infection and other associated complications. Due to concern over increased wear in younger, more active populations, other bearing surfaces have been evaluated, particularly metal-on-metal with wear rates theorized to be lower than conventional THA. Unique to metal-on-metal THA, however, is the possibility of local soft tissue reactions that can mimic infection, making proper diagnosis and treatment difficult. We present a case series of nine hips in eight patients undergoing revision of metal-on-metal THA for local soft tissue reactions, three of which were also found to be concomitantly infected. The laboratory and hip aspirate data described show significant overlap between the infected and non-infected cases. Care must be taken when evaluating patients with failed metal-on-metal THA as there may be an increased incidence of co-infection in this group of patients.
INTRODUCTION
Total hip arthroplasty is a well established treatment for hip pain and dysfunction due to advanced osteoarthritis. The traditional bearing in hip arthroplasty is metal-on-polyethylene, formerly standard, and more recently highly cross-linked. Wear rates with this bearing surface have been studied extensively and found to be acceptable over long periods for most.1 With metal-on-polyethylene bearing surfaces, there is typically no significant local soft tissue reaction to wear. Infection rates are usually seen as a distinct complication for primary total hip arthroplasty, and have been shown to be approximately 1%.2,3,4 patients with a total hip arthroplasty presenting with complaints of pain, systemic symptoms, wound issues and/or local swelling, redness or warmth are evaluated with tests that make detection of an infection relatively straightforward, if they can all be done. These include serum ESR and CRP, and a hip aspiration sent for a cell count and differential as well as a culture and sensitivity profile.5,6 These patients often have typical signs and symptoms, and abnormal results of one or more of these laboratory values that are independent of and unrelated to any bearing wear. In those patients who are found to have an infected THA, the most common pathogen is Staphylococcus Aureus, followed by other strains of Staphylococcus, mainly coagulase-negative species.7 For total hips undergoing revision for presumed aseptic loosening, between 4%8 and 13%9 are found to be concomitantly infected at the time of revision surgery. Based on evidence of higher revision rates in younger, more active patients with THA,10,11 interest in alternative hard bearings including metal-on-metal has increased. The theoretical advantage of lower wear rates with this bearing surface has made it attractive for higher demand patients. Recently, however, the particles or ions generated by metal-on-metal bearings have been implicated in significant local reactions.12 These reactions, alternatively termed Aseptic Lymphocytic Vasculitis Associated Lesion (ALVAL), Adverse Reaction to Metal Debris (ARMD), Adverse Local Tissue Reaction (ALTR), metallosis or pseudotumor, can cause considerable dysfunction and local tissue destruction. Proper diagnosis of these local complications can be challenging as the clinical picture of one of these local reactions can be hard to distinguish from an infected metal-on-metal total hip arthroplasty. Laboratory values, radiographic imaging and aspiration cell count results can be similar in the aseptic (reaction to metal debris) and septic conditions. Infection rates for metal-on-metal arthroplasty (without concomitant local reactions) have also been shown to be approximately 1%, with typical pathogens being Staphylococcus species. Infection rates for patients with adverse local tissue reactions are currently not well defined.
Treatment of an infected total hip arthroplasty is typically by irrigation and debridement or two stage revision. Our hypothesis is that the concomitant infection rate in patients with a local tissue reaction around a metal-on-metal THA may be higher than in patients with either conventional bearing (metal-on-polyethylene) THA or those with a metal-on-metal THA without evidence of a local tissue reaction. Secondly, we predict that the causative pathogens in patients with local tissue reactions and concomitant infection are atypical compared to what is commonly seen with infected THA. We present a consecutive case series of patients undergoing revision THA for adverse reaction to metal debris and the subgroup that was found to have concomitant infection.
METHODS
Nine metal-on-metal total hip arthroplasties in eight consecutive patients undergoing revision for persistent pain and dysfunction, and with pre-operative and/or intra-operative findings of ALVAL, pseudotumor or metal debris reaction were followed post operatively via chart review. IRB approval was obtained from the institution's internal review board prior to the initiation of the study. The patients were followed between 3 months and 1 year after revision. Pathological, microbiology and laboratory markers for infection were assessed. Post operative treatment courses were also reviewed.
RESULTS
Demographics: The current series consisted of five men and three women ages 50 to 73 years. For one patient (#2) both the right and left hips were involved at separate incidences. Time from index procedure to revision ranged from 12 months to five years. Revisions were undertaken due to: Pain (3/8), acetabular loosening (2/8), dislocation/instability (1/8), and infection (2/8).
Laboratory Evaluation: Pre-operative ESR/CRP levels, hip joint aspirate cell counts, and serum cobalt/ chromium levels (Table 1) when available.
TABLE 1.
Serum Cobalt and Chromium, Total nucleated cells from hip aspirate, ESR and CRP for each patient
| Patient | Preoperative Serum Co/Cr Ion Levels (ug/L) | Total Nucleated/MM3 | ESR (mm/hr) | CRP (mg/dl) |
|---|---|---|---|---|
| 1 | n/a | 1599* | 75* | 33.2* |
| 2a | n/a | 57715* | 81* | 7.7* |
| 2b | 33.7 / 2.4 | 11147 | 29 | 3.6 |
| 3 | n/a | lost sample | 42 | 8.9 |
| 4 | 9.1 / 3.9 | 41344 | 43 | 2.5 |
| 5 | 127.5 / 1.0 | n/a | 3 | 0.5 |
| 6 | n/a | 183530 | 14 | 0.5 |
| 7 | n/a | 112432 | 3 | 0.5 |
| 8 | n/a | 480195* | 58* | 30.8* |
denotes infected cases.
For patient #2 both the right (a) and left (b) metal-on-metal total hips were revised.
Microbiology: Thirty-three percent (3/9) of the cases were culture positive via pre- operative aspirate (Patient 1 and Patient 8), or with post-operative growth of intra-operative cultures (Patient 2a). Of the culture positive patients all three grew streptococcus; two with -Hemolytic streptococcus (Patients 1 and 8) and one with nutritionally variant streptococcus-Granulicatella Abiotrophia (Patient 2a).
Intraoperative Findings: Thirty-Three percent (3/9 cases) with necrotic appearing tissues (Figure 1). Other common findings were large joint effusions 33% (Patients 2a/b, 6) and metallosis 33% (Patients 4,5,7).
Figure 1.
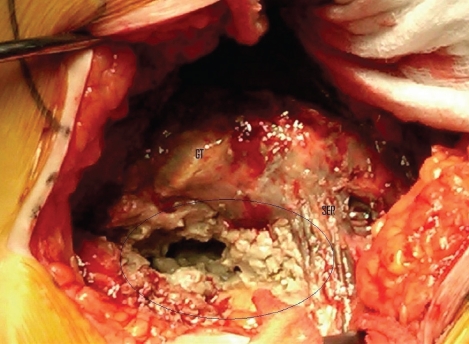
Representative intra operative photo showing soft tissue necrosis and “purulence” which is typically seen. GT: Greater Trochanter, SER: Residual short external rotators.
Pathology: (Table 2).
TABLE 2.
Final pathology tissue diagnosis from specimens obtained at the time of operation.
| Patient | Final Tissue Diagnosis |
|---|---|
| 1* | Coagulative Necrosis |
| 2a* | Acute inflammation with areas of histiocytic and fibrotic appearance. |
| 2b | Coagulative Necrosis. No acute/chronic inflammation |
| 3 | Necrosis, acute and chronic inflammation and fibrinopurulent exudate |
| 4 | Dense fibrous tissue with chronic inflammation, focal granulomatous inflammation and foreign body giant cell reaction and necrosis. |
| 5 | Aseptic lymphocytic vasculitis associated lesion |
| 6 | Necrotic tissue without significant associated inflammation |
| 7 | Necrotic tissue. No viable synovium or acute inflammation identified. |
| 8* | Fibrovascular tissue w/mixed acute and chronic inflammatory infiltrate. Focal areas of dense perivascular lymphocytic aggregates |
denotes infected cases.
Operative Treatment: Irrigation and debridement alone (Patient 8, acute hematogenous infection, mono-block cup). Irrigation and debridement with bearing exchange (Patient 1,3). Acetabular Revision w/polyethylene liner (Patients 2a/b, 4-7).
DISCUSSION
This case series presents eight patients with nine metal-on-metal total hips undergoing revision arthroplasty for pain, dysfunction or arthroplasty failure. All patients had evidence of an adverse local tissue reaction to metal debris, pseudotumor or ALVAL by direct intra-operative observation of significant tissue destruction or a cystic mass, or by pathological tissue diagnosis. Thirty-three percent of the cases were found to be concomitantly infected.
The concern over adverse metal reactions and soft tissue pseudotumors in patients undergoing metal bearing hip arthroplasty continues to grow. Reports to date have been mostly single cases or case series,13-17 but Glyn-Jones et al.18 presented a large series of patients undergoing revision of metal-on-metal hips, and found a 1.8 % revision rate for pseudotumor alone. In their series, Kaplan Meier curves showing cumulative revision rates for pseudotumor increased with time, to as high as 4% at eight years.
It has also been found that infection in the face of adverse local tissue reaction after metal-on-metal total hip arthroplasty may be challenging to properly diagnose and treat given the overlap of symptoms, signs and laboratory values in both processes.19 Despite the similarities in clinical presentation, the treatment strategies for these two problems is usually quite different, making accuracy of the diagnosis important in optimizing patient outcome after revision.
In general, the infection rate for traditional (polyethylene) bearing THA is around 1%. (NIH Concensus Development Panel). The overall infection rate for metal-on-metal THA has also been shown to have an incidence of 1% or less.20,21 The presenting symptoms and signs of infection should be similar for both traditional (polyethylene) bearings and metal bearings particularly in the absence of any adverse local soft tissue reaction. Patients presenting with an adverse soft tissue reaction and/or pseudotumor typically present with more vague complaints of pain and hip dysfunction along with radiographic findings of a cystic mass.13 This presentation may be difficult to differentiate from infection.19
The standard evaluation to diagnose an infected arthroplasty includes serum ESR and CRP values, and if these are elevated or suspicion is high, a hip joint aspiration sent for white (total nucleated) cell count and differential (PMN percentage in particular) and bacterial culture with sensitivity testing. Although nonspecific, the ESR and CRP are good indicators of systemic inflammation when elevated. The joint aspiration is a more accurate test for the diagnosis, but false positives and negatives do occur, as well as an inability to obtain fluid on occasion. Hip aspirates with a total nucleated cell count greater than 4200 cells/ml and greater than 80% PMN if taken in isolation or with a total nucleated cell count >3000, if both ESR and CRP are elevated above 30 mm/hr and 10mg/dL respectively, have a high probability of being infected.6 A positive culture from the hip aspirate is the gold standard for pre-operative diagnosis of an infected THA, but it can take as long as 5-10 days to grow. Gross purulence and positive intra-operative tissue culture then becomes the final test used to confirm or refute infection.
It is now being recognized, however, that many of these pre-operative laboratory values may also be abnormal in metal-on-metal hips with local tissue reactions but without infection.19 In the current series, ESR and CRP were elevated in 3 of 6 hips without infection, and the total nucleated cell count was highly elevated in all uninfected hips (4/6) that had a successful aspirate. Furthermore, patient 3 did have an aspirate with this report “Approximately 13 ml of pus were aspirated (from the hip). The fluid was delivered to pathology for cell count and to microbiology for culture … per the clinical request” Unfortunately, the cell count tube was lost during transportation. The culture was negative. Thus, it appears that aspirates of affected metal-on-metal hips without infection can even have purulent appearing fluid.
This considerable overlap can make obtaining an accurate diagnosis and choosing the optimal treatment quite challenging. Differentiating the two processes as being separate or concomitant is critical since isolated local soft tissue reactions can often be treated with revision of the bearing surface only to a non-metal alternative; but for infection, irrigation and debridement with extended IV antibiotics or more commonly two stage revision of the entire prosthesis may be necessary.
In the current series, 33% (3/9 hips) were found to be infected as well as have signs of local reaction to metal debris. Two patients had known infections at the time of operation with a pathological diagnosis of ALVAL or intraoperative pseudotumor. The third, with a large pseudotumor and presumed ALVAL only, proved to be culture positive on post operative day 4. This ratio is much higher than that reported for either traditional bearings or metal-on-metal bearings without evidence of a local soft tissue reaction. Prior to this series concomitant infection and local soft tissue reaction had only been described in a single case report by Watters et al17 In this case, the presentation and treatment of a patient with concomitant local soft tissue reaction and local infection is described. This rate of coinfection is also presumably higher than those patients found to be infected at the time of revision for polyethylene wear.
Intraoperative observational evaluation also has the potential to be unreliable in distinguishing infection from isolated local soft tissue reactions. Common to both, in this series (whether or not infection was present) and those previously published, are the findings of metal staining of the soft tissues, cystic masses, large exudates and tissue necrosis. In the current series pathological evaluation is consistent with previous descriptions of pseudotumor and local metal reactions.13,17,19 In our infected patients, a pathology reading of the intraoperative frozen section of ‘acute inflammation’ (>5 WBC per hpf in multiple fields) seemed to be the most predictive descriptor of infection as two of the three patients had this present.
Finally, the prevalence of uncommon infective agents in our series was also felt to be unusual. Streptococcus has occasionally been implicated in concomitant infection and local metal reaction,17 but it is not among the more common bacteria isolated from infected total hip arthroplasties, particularly Granulicatella Abiotrophia. This finding may certainly be a function of the small number of patients, but predilection for infection with atypical agents in the face of soft tissue metal reaction cannot be excluded.
CONCLUSION
The prevalence of concomitant infection and adverse local tissue reaction in patients with a metal-on-metal total hip arthroplasty may be higher than in patients with traditional polyethylene bearings or in patients with metal-on-metal bearings without signs of ALVAL, ALTR, or pseudotumor. Distinguishing between isolated adverse soft tissue reactions, deep infection and the coexistence of both can be challenging in a metal bearing total hip arthroplasty. Vigilance should be maintained in the evaluation of patients with painful metal-on-metal total hips with a suspicion of infection or ALTR, as the treatment algorithm and outcome for each problem can vary significantly. Atypical pathogens may be found more frequently in hips with ALTR and concomitant infection.
REFERENCES
- 1.McCalden R.W., et al. Wear rate of highly cross-linked polyethylene in total hip arthroplasty. A randomized controlled trial. The Journal of bone and joint surgery. American volume. 2009;91(4):773–82. doi: 10.2106/JBJS.H.00244. [DOI] [PubMed] [Google Scholar]
- 2.Urquhart D.M., et al. Incidence and risk factors for deep surgical site infection after primary total hip arthroplasty: a systematic review. The Journal of arthroplasty. 2010;25(8):1216–22. doi: 10.1016/j.arth.2009.08.011. e1-3. [DOI] [PubMed] [Google Scholar]
- 3.Engesaeter L.B., et al. Does cement increase the risk of infection in primary total hip arthroplasty? Revision rates in 56,275 cemented and uncemented primary THAs followed for 0-16 years in the Norwegian Arthroplasty Register. Acta orthopaedica. 2006;77(3):351–8. doi: 10.1080/17453670610046253. [DOI] [PubMed] [Google Scholar]
- 4.Hailer N.P., Garellick G., Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta orthopaedica. 2010;81(1):34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghanem E., et al. Cell count and differential of aspirated fluid in the diagnosis of infection at the site of total knee arthroplasty. The Journal of bone and joint surgery. American volume. 2008;90(8):1637–43. doi: 10.2106/JBJS.G.00470. [DOI] [PubMed] [Google Scholar]
- 6.Schinsky M.F., et al. Perioperative testing for joint infection in patients undergoing revision total hip arthroplasty. The Journal of bone and joint surgery. American volume. 2008;90(9):1869–75. doi: 10.2106/JBJS.G.01255. [DOI] [PubMed] [Google Scholar]
- 7.Bergstrom B., et al. Complications after total hip arthroplasty according to Charnley in a Swedish series of cases. Clinical orthopaedics and related research. 1973(95):91–5. [PubMed] [Google Scholar]
- 8.Parvizi J., et al. Aseptic Loosening of Total Hip Arthroplasty: Infection Always Should be Ruled Out. Clinical orthopaedics and related research. 2011 doi: 10.1007/s11999-011-1822-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moojen D.J., et al. Incidence of low-grade infection in aseptic loosening of total hip arthroplasty. Acta orthopaedica. 2010;81(6):667–73. doi: 10.3109/17453674.2010.525201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dowdy P.A., Rorabeck C.H., Bourne R.B. Uncemented total hip arthroplasty in patients 50 years of age or younger. The Journal of arthroplasty. 1997;12(8):853–62. doi: 10.1016/s0883-5403(97)90154-6. [DOI] [PubMed] [Google Scholar]
- 11.Solomon M.I., et al. Survivorship of cemented total hip arthroplasty in patients 50 years of age or younger. The Journal of arthroplasty. 1992;7(Suppl):347–52. doi: 10.1016/s0883-5403(07)80023-4. [DOI] [PubMed] [Google Scholar]
- 12.Aroukatos P., et al. Immunologic adverse reaction associated with low-carbide metal-on-metal bearings in total hip arthroplasty. Clinical orthopaedics and related research. 2010;468(8):2135–42. doi: 10.1007/s11999-009-1187-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pandit H G.-J.S., McLardy-Smith P, Gundle R, Whitwell D, Gibbons CLM, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours Associated with Metal-on-Metal Hip Resurfacing. J Bone Joint Surg Br. 2008;90-B:847–51. doi: 10.1302/0301-620X.90B7.20213. [DOI] [PubMed] [Google Scholar]
- 14.Pandit H V.M., Whitwell D, Crook D, Luqmani R, Ostlere S, Murray DW, Athanasou NA. Necrotic Granulomatous Pseudotumours in Bilateral Resurfacing Hip Arthoplasties: Evidence for a Type IV Immune Response. Vichows Arch. 2008;453:529–534. doi: 10.1007/s00428-008-0659-9. [DOI] [PubMed] [Google Scholar]
- 15.Clayton RAE B.A., Salter DM, grant MH, Patton JT, Porter D. Inflammatory Pseudotumor Associated with Femoral nerve Palsy Following Metal-on-Metal resurfacing of the Hip. A Case Report. J Bone Joint Surg Am. 2008;90:1988–1993. doi: 10.2106/JBJS.G.00879. [DOI] [PubMed] [Google Scholar]
- 16.Leigh W O.G.P., Lawson EM, Hung NA, Theis JC, Matheson J. Pelvic Pseudotumor: An Unusual Presentation of an Extra-Articular granuloma in a Well-Fixed Total Hip Arthroplasty. J Arthroplasty. 2008;23(6):934–938. doi: 10.1016/j.arth.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Watters T.S., et al. Pseudotumor with superimposed periprosthetic infection following metal-on-metal total hip arthroplasty: a case report. The Journal of bone and joint surgery. American volume. 2010;92(7):1666–9. doi: 10.2106/JBJS.I.01208. [DOI] [PubMed] [Google Scholar]
- 18.Glyn-Jones S PH., Kwon Y-M, Doll H, Gill HS, Murray DW. Risk Factors for Inflammatory Pseudo-tumour Formation Following Hip resurfacing. J Bone Joint Surg Br. 2009;91-B:1566–74. doi: 10.1302/0301-620X.91B12.22287. [DOI] [PubMed] [Google Scholar]
- 19.Mikhael M.M., Hanssen A.D., Sierra R.J. Failure of metal-on-metal total hip arthroplasty mimicking hip infection. A report of two cases. The Journal of bone and joint surgery. American volume. 2009;91(2):443–6. doi: 10.2106/JBJS.H.00603. [DOI] [PubMed] [Google Scholar]
- 20.Milosev I, T.R., Kovac S, Cor A, Pisot V. Survivorship and Retrieval Analysis of Sikomet Metal-on-Metal Total Hip Replacements at a Mean of Seven Years. J Bone Joint Surg Am. 2006;88(6):1173–82. doi: 10.2106/JBJS.E.00604. [DOI] [PubMed] [Google Scholar]
- 21.Kim SY, K.H., Ihn JC, Cho MR, Koo KH, Kim CY. Cementless Metasul Metal-on-Metal Total Hip Arthroplasty in Patients Less Than Fifty Years Old. J Bone Joint Surg Am. 2004;86-A(11):2475–81. doi: 10.2106/00004623-200411000-00018. [DOI] [PubMed] [Google Scholar]


