Abstract
We tested the hypothesis that reductions in vascular endothelial function (endothelium-dependent dilation, EDD) with age are related to increases in sympathetic activity. Among 314 healthy men and women, age was inversely related to brachial artery flow-mediated dilation (FMD) (r = −0.30, P < 0.001), a measure of EDD, and positively related to plasma norepinephrine concentrations (PNE), a marker of sympathetic activity (r = 0.49, P < 0.001). Brachial FMD was inversely related to PNE in all subjects (r = −0.25, P < 0.001) and in men (n = 187, r = −0.17, P = 0.02) and women (n = 127, r = −0.37, P < 0.001) separately. After controlling for PNE (multiple regression analysis), brachial FMD remained significantly related to age in all subjects (r = −0.20, P < 0.001) and in men (r = −0.23, P < 0.01), but not women (r = −0.16, P = 0.06). Consistent with this, brachial FMD remained significantly related to PNE when controlling for age (r = −0.24, P < 0.01) and menopause status (r = −0.24, P < 0.01) in women. Indeed, PNE was the strongest independent correlate of brachial FMD in women after controlling for conventional cardiovascular disease risk factors (r = −0.22, P = 0.01). This relation persisted in a subset of women (n = 113) after further accounting for the effects of plasma oxidized low-density lipoprotein (P < 0.05), a circulating marker of oxidative stress. Endothelium-independent dilation was not related to age in either men or women (P > 0.05). These results provide the first evidence that EDD is inversely related to sympathetic activity, as assessed by PNE, among healthy adults varying in age. In particular, our findings suggest that sympathetic nervous system activity may be a key factor involved in the modulation of vascular endothelial function with aging in women.
Keywords: endothelium-dependent dilation, flow-mediated dilation, oxidative stress
age is the main risk factor for cardiovascular diseases, primarily as the result of adverse changes to arteries (23). A key change to arteries with aging that contributes to increased risk of cardiovascular diseases is the development of vascular endothelial dysfunction, as indicated by reductions in endothelium-dependent dilation (4, 24, 38, 46, 47). As such, identifying the factors related to impaired endothelium-dependent dilation with aging is an important clinical goal as it may lead to effective strategies to prevent and/or treat age-associated endothelial dysfunction (36).
Sympathetic nervous system activity could be an important factor contributing to endothelial dysfunction with age. In young adults, acute increases in sympathetic activity above normal baseline levels can impair endothelium-dependent dilation in response to experimental stressors (11, 18, 25). Moreover, several metabolic and cardiovascular disorders are associated with both increased resting sympathetic activity and reduced endothelium-dependent dilation (2, 5, 15, 27, 41, 42). Importantly, sympathetic activity increases with age in the absence of disease (35, 48). However, it is unknown if reductions in endothelium-dependent dilation with age are related to increases in sympathetic activity among healthy adults.
If endothelium-dependent dilation and sympathetic activity are related with aging, it is possible that the nature of the relation may not be the same for men and women. Although endothelium-dependent dilation decreases on average with age in both men and women, it is possible that some of the factors involved may differ between the sexes (32, 33), as they do for other forms of vascular dysfunction with aging (9, 29).
In the present study we tested the hypothesis that reductions in endothelium-dependent dilation with age are related to increases in sympathetic activity among healthy men and women. To do so, we assessed brachial artery flow-mediated dilation (FMD), a measure of endothelium-dependent dilation (3), and plasma norepinephrine (PNE), a marker of sympathetic activity (35, 48), in a large group of adults varying in age, but free of metabolic and cardiovascular disease. We first determined the simple relations among age, brachial FMD, and plasma norepinephrine in the overall group and separately in men and women. We then assessed the independent effects of PNE on brachial FMD using multiple regression and partial correlation analyses. Finally, we examined the potential role of oxidative stress by assessing the influence of plasma oxidized low-density lipoprotein (LDL), a circulating marker of oxidant modification of lipids (6).
METHODS
Subjects.
A cohort from our laboratory database (n = 314) previously assessed for endothelial function were used for the analysis. All subjects were healthy, nonsmoking adults (187 men, 127 women) between the ages of 18 and 79 yr who were free of clinical disease as assessed by medical history, physical examination, blood chemistries, electrocardiogram, resting blood pressure, and cardiovascular responses to a graded exercise test. Subjects were not taking medications and refrained from all dietary supplements for 2 wk prior to participation in the study. All procedures were approved by the Institutional Review Board at the University of Colorado at Boulder. The nature, risks, and benefits of all study procedures were explained to volunteers and their written informed consent was obtained before participation in the study.
Procedures.
All testing was performed at the Clinical Translational Research Center (CTRC) at the University of Colorado at Boulder following a 12-h fast from food and caffeine and 24-h abstention from exercise and alcohol. All premenopausal women were tested during the low follicular phase of the menstrual cycle to account for possible confounds of circulating reproductive hormones. Postmenopausal status was confirmed by follicular stimulating hormone levels > 40 IU/l.
Subject characteristics.
Arterial blood pressure was measured over the brachial artery during seated rest using a semiautomated device (Dynamap pro 100, GE, Health Care). Total cholesterol, LDL cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides, and fasting glucose were measured using standard assays, and plasma norepinephrine by high-performance liquid chromatography (BioRad Laboratories) at the University of Colorado CTRC core laboratory. Plasma oxidized LDL was assessed by ELISA (ALPCO) as described previously (19, 20, 43). All blood samples were drawn from an intravenous catheter placed in the left antecubital fossa. Blood samples for norepinephrine measurements were drawn after 20 min of supine rest. Habitual physical activity levels were calculated from estimates of daily energy expenditure using the Stanford Physical Activity Questionnaire (34).
Brachial artery endothelium-dependent dilation and endothelium-independent dilation.
Duplex ultrasonography (Power Vision 6000, Toshiba; multi-frequency linear-array transducer) was used to assess brachial artery FMD and endothelium-independent dilation (i.e., brachial artery dilation in response to 0.4 mg sublingual nitroglycerin) as described previously by our laboratory (12, 19, 20). To ensure subject safety, endothelium-independent dilation was only assessed in individuals with a systolic blood pressure > 100 mmHg. FMD measurements were reported as absolute and percent change in accordance with recent guidelines (10, 16). In a subset of subjects (men: n = 48, women: n = 30), peak hyperemic shear rate was calculated as (4 × time-averaged peak velocity)/occlusion diameter based on a small, centered sample volume from the first 10 velocity envelopes (first 15 s) following cuff release per recent recommendations (16).
Data analysis.
Statistical analyses were performed in SPSS (IBM SPSS Statistics 19). The strength of the linear relations between age, PNE, and brachial FMD were assessed using Pearson product-moment correlation analyses. Differences in correlation coefficients were assessed using Fisher's z-transformation. Multiple linear regression analysis was used to further assess relations while controlling for additional variables. Partial correlation analysis was used to statistically remove such variables and assess the independent bivariate relation of interest. Statistical significance was set at P < 0.05.
RESULTS
Clinical characteristics of subjects.
Clinical and vascular characteristics are presented in Table 1 and Table 2, respectively. Mean PNE concentrations were 243 ± 7 pg/ml for all subjects, 220 ± 8 pg/ml for men, and 275 ± 11 pg/ml for women. Plasma oxidized LDL was 55 ± 1, 58 ± 1, and 51 ± 2 U/l for all subjects, men, and women, respectively.
Table 1.
Clinical characteristics of subjects
| Characteristic | All Subjects | Men | Women |
|---|---|---|---|
| n | 314 | 187 | 127 |
| Age, yr | 48 ± 1 | 47 ± 1 | 48 ± 2 |
| Systolic blood pressure, mmHg | 117 ± 1 | 120 ± 1 | 113 ± 1 |
| Diastolic blood pressure, mmHg | 69 ± 1 | 71 ± 1 | 67 ± 1 |
| Heart rate, beats/min | 60 ± 1 | 59 ± 1 | 61 ± 1 |
| Body mass index, kg/m2 | 25.2 ± 0.2 | 26.0 ± 0.3 | 23.9 ± 0.3 |
| Waist:hip ratio | 0.84 ± 0.01 | 0.89 ± 0.01 | 0.76 ± 0.00 |
| Physical activity, MET h/wk | 68 ± 4 | 68 ± 4 | 69 ± 7 |
| Total cholesterol, mg/dl | 191 ± 2 | 187 ± 3 | 198 ± 3 |
| HDL cholesterol, mg/dl | 54 ± 1 | 47 ± 1 | 64 ± 1 |
| LDL cholesterol, mg/dl | 115 ± 2 | 114 ± 2 | 116 ± 3 |
| Triglycerides, mg/dl | 110 ± 3 | 125 ± 6 | 92 ± 4 |
| Fasting blood glucose, mg/dl | 90 ± 1 | 92 ± 1 | 88 ± 1 |
Data are means ± SE; HDL, high-density lipoprotein, LDL, low-density lipoprotein.
Table 2.
Vascular characteristics of subjects
| Characteristic | All Subjects | Men | Women |
|---|---|---|---|
| Flow-mediated dilation, %Δ | 6.1 ± 0.2 | 6.1 ± 0.2 | 6.3 ± 0.3 |
| Flow-mediated dilation, mmΔ | 0.22 ± 0.01 | 0.24 ± 0.01 | 0.19 ± 0.01 |
| Baseline diameter, mm | 3.69 ± 0.04 | 4.08 ± 0.04 | 3.12 ± 0.04 |
| Peak hyperemic blood velocity, cm/s | 45 ± 1 | 46 ± 1 | 45 ± 2 |
| Peak shear rate, s−1 | 438 ± 14 | 409 ± 15 | 484 ± 26 |
Data are means ± SE. Peak hyperemic blood velocity and shear rate assessed in subset of subjects [n (men/women) = 125/56 and 48/30, respectively].
Age-associated changes in brachial FMD and PNE.
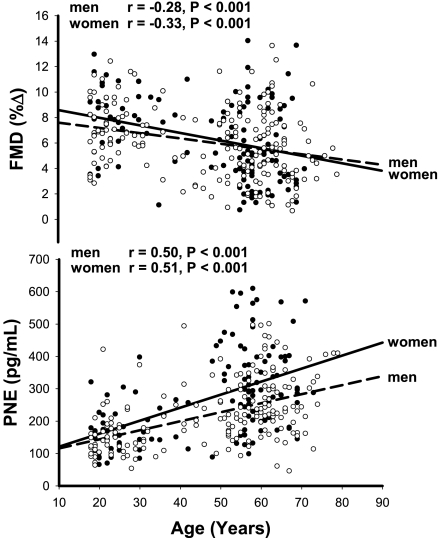
In all subjects, age was inversely related to brachial FMD (%Δ: r = −0.30, P < 0.001; mmΔ: r = −0.31, P < 0.001) and positively related to PNE (r = 0.49, P < 0.001). These relations also were observed in men (FMD%Δ: r = −0.28, P < 0.001; FMDmmΔ: r = −0.31, P < 0.001; PNE: r = 0.50, P < 0.001) and women (FMD%Δ: r = −0.33, P < 0.001; FMDmmΔ: r = −0.31, P < 0.001; PNE: r = 0.51, P < 0.001) when assessed separately (Fig. 1).
Fig. 1.
Relation between brachial artery flow-mediated dilation (FMD) and age (top) and plasma norepinephrine (PNE) and age (bottom) in men (○) and women (●).
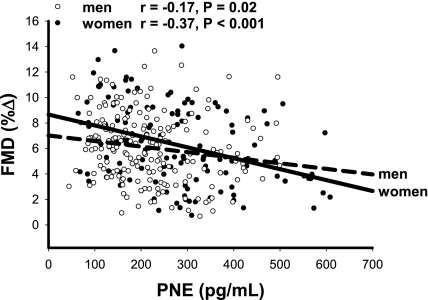
Brachial FMD was inversely related to PNE in all subjects (%Δ: r = −0.25, P < 0.001; mmΔ: r = −0.29, P < 0.001) and in men (%Δ: r = −0.17, P = 0.02; mmΔ: r = −0.16, P = 0.03) and women (%Δ: r = −0.37, P < 0.001; mmΔ: r = −0.37, P < 0.001) separately (Fig. 2), although the relation trended toward being stronger in women than in men (P = 0.06). Baseline brachial artery diameter and peak shear rate were not related to age or PNE in men or women (P > 0.05 for all relations).
Fig. 2.
Relation between FMD and PNE in men (○) and women (●).
Relation between brachial FMD and age when controlling for PNE.
In a multiple linear regression model, brachial FMD remained significantly related to age in all subjects (%Δ: r = −0.20, P < 0.001; mmΔ: r = −0.19, P < 0.001) and in men (%Δ: r = −0.23, P < 0.01; mmΔ: r = −0.27, P < 0.001) after controlling for PNE. In contrast, the relation between brachial FMD and age no longer was significant in women after controlling for PNE (%Δ: r = −0.16, P = 0.06; mmΔ: r = −0.14, P = 0.10). Consistent with this observation, brachial FMD remained significantly related to PNE when controlling for age in women (%Δ: r = −0.24, P < 0.01; mmΔ: r = −0.25, P < 0.01), but not men (P > 0.05). Further controlling for menopause status (coded bivariate variable) in women did not affect the FMD-PNE relation (%Δ: r = −0.24, P < 0.01; mmΔ: r = −0.25, P < 0.01). Menopause status was not independently predictive of FMD when controlling for age and PNE in women (P > 0.05).
Relation between brachial FMD, age, and PNE when controlling for clinical characteristics.
When controlling for clinical characteristics (age, menopause status, systolic blood pressure, diastolic blood pressure, body mass index, waist/hip ratio, physical activity, total cholesterol, HDL cholesterol, LDL cholesterol, and fasting glucose) in a multiple linear regression model, PNE remained a significant independent predictor of FMD in women (%Δ: r = −0.22, P = 0.01 [Table 3]; mmΔ: r = −0.25, P < 0.01). Indeed, PNE was a stronger independent predictor of FMD in women than any other clinical factor assessed. Accounting for the same clinical characteristics in men did not affect the relation between PNE and FMD (P > 0.05), but weakened the association between age and FMD (P > 0.05; Table 3).
Table 3.
Multiple linear regression analysis assessing the independent influence of plasma norepinephrine (PNE), age and clinical characteristics on brachial flow-mediated dilation (%Δ)
| Women |
Men |
|||
|---|---|---|---|---|
| Variable | r | P | r | P |
| PNE, pg/ml | −0.22 | 0.01 | −0.05 | 0.54 |
| Age, yr | −0.08 | 0.39 | −0.09 | 0.24 |
| Menopause status, pre/post | 0.03 | 0.74 | ||
| Systolic blood pressure, mmHg | 0.04 | 0.68 | −0.09 | 0.24 |
| Diastolic blood pressure, mmHg | −0.08 | 0.38 | 0.04 | 0.62 |
| Body mass index, kg/m2 | −0.07 | 0.45 | <0.00 | 0.99 |
| Waist:hip ratio | 0.12 | 0.17 | −0.04 | 0.58 |
| Physical activity, MET h/wk | −0.04 | 0.67 | 0.11 | 0.15 |
| Total cholesterol, mg/dl | 0.06 | 0.51 | −0.02 | 0.77 |
| HDL cholesterol, mg/dl | −0.10 | 0.26 | <0.00 | 1.00 |
| LDL cholesterol, mg/dl | −0.06 | 0.48 | 0.02 | 0.82 |
| Fasting blood glucose, mg/dl | −0.05 | 0.53 | −0.10 | 0.19 |
HDL, high-density lipoprotein, LDL, low-density lipoprotein.
Influence of plasma oxidized LDL on the brachial FMD-PNE relation in women.
Because brachial FMD and PNE remained inversely related when controlling for clinical characteristics in women, we sought to determine if the strength of this relation persisted after further accounting for oxidized LDL, a circulating marker of oxidative stress. As in the overall group of women, PNE was an independent predictor of brachial FMD when controlling for all factors shown in Table 3 in the large subset of women on whom plasma oxidized LDL values were available (%Δ: r = −0.19, P < 0.05; mmΔ: r = −0.21, P < 0.05, n = 113). PNE remained an independent correlate of brachial FMD after further accounting for the effect of plasma oxidized LDL in this group (P < 0.05).
Brachial artery endothelium-independent dilation.
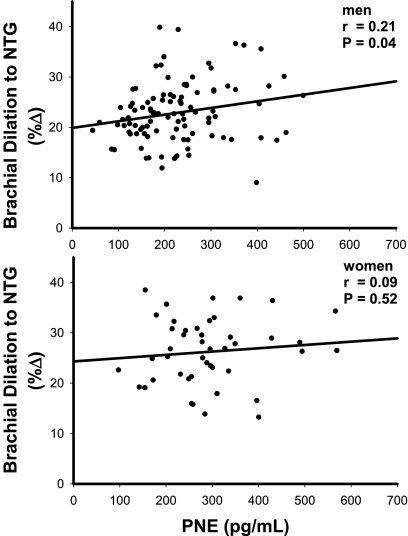
Endothelium-independent dilation, a measure of brachial artery vascular smooth muscle responsiveness to nitric oxide, was not related to age in the overall group or in men or women (P > 0.05). Endothelium-independent dilation was positively related to PNE in men (%Δ: r = 0.21, P = 0.04; mmΔ: r = 0.22, P = 0.02), but not women (%Δ: r = 0.09, P = 0.52; mmΔ: r = 0.01, P = 0.93; Fig. 3). Endothelium-independent dilation did not contribute to the lack of an independent relationship between FMD and PNE when accounting for age in men (data not shown).
Fig. 3.
Relation between endothelium-independent dilation (brachial dilation to nitroglycerin [NTG]) and PNE in men (top) and women (bottom).
DISCUSSION
This is the first study to report that vascular endothelial function is related to an index of sympathetic nervous system activity in individuals free from clinical disease. Specifically, we found brachial artery FMD, a measure of endothelium-dependent dilation (3), was inversely related to PNE, a commonly used marker of sympathetic activity (35, 48), in an overall group of healthy adults aged 18–79 yr. This also was the case in men and women when analyzed separately, with the relation tending to be stronger in women than in men. The inverse relation between brachial FMD and age in women no longer was significant after accounting for the influence of PNE, whereas there was no effect of PNE on the brachial FMD-age relation in men. Importantly, our results indicate that PNE is an independent predictor of brachial FMD across age and menopause status in women and is a stronger correlate of FMD than any clinical characteristic in that group, including conventional risk factors for cardiovascular diseases. Finally, we found that the independent association between brachial FMD and PNE in women was not related to either plasma oxidized LDL, a circulating marker of oxidative stress, or brachial artery dilation to nitroglycerin, a measure of vascular smooth muscle sensitivity to nitric oxide.
Brachial FMD, PNE, and age.
The relation between baseline brachial FMD and PNE in the present study is consistent with previous findings showing reductions in endothelium-dependent dilation in response to experimental sympathetic activation in young subjects and the fact that endothelium-dependent dilation and sympathetic activity are inversely associated in patients with clinical disorders (2, 5, 11, 15, 18, 25, 27, 41, 42). A recent study also reported an inverse relation between muscle sympathetic activity and nonspecific peripheral vascular function in a small cohort of healthy adults (37) and, in rodents, changes in α-adrenergic vascular tone modulate endothelium-dependent dilation in skeletal muscle arterioles (8, 21). Our results extend these findings by showing for the first time that a well-established measure of vascular endothelial function is inversely related to a commonly used marker of sympathetic activity among individuals free of clinical disease.
The inverse relation between brachial FMD and PNE in the overall group was primarily driven by the strength of this relation in women. As a result, controlling for the influence of PNE in women was sufficiently strong as to render the relation between age (or menopause status) and brachial FMD nonsignificant. Moreover, in contrast to men, PNE was an independent predictor of brachial FMD in women and, in fact, was a stronger independent correlate than conventional cardiovascular disease risk factors. In men, no clinical characteristic was found to be a significant independent predictor of FMD. These findings further support the idea that the factors modulating vascular endothelial function with aging in women may, in some cases, differ from those in men (9, 29). In particular, the present results suggest that increases in sympathetic activity might contribute independently to age-associated endothelial dysfunction in women, but not men.
Mechanisms.
The mechanisms by which sympathetic activity (PNE) might influence endothelium-dependent dilation more in women than men cannot be completely discerned from the present analysis. That plasma oxidized LDL had no influence on the independent relation between brachial FMD and PNE in women does not support an obvious role for oxidative stress. However, experimental manipulation of reactive oxygen species bioavailability (e.g., via antioxidant administration) would be required to more definitively assess this mechanism. Our data also indicate that brachial artery dilation to nitroglycerin, a nitric oxide donor, is not related to age in either men or women, or to PNE in women. This finding suggests that the inverse relation between brachial FMD and PNE in women is mediated by factors associated with production of dilatory molecules by vascular endothelium per se (e.g., nitric oxide) rather than the responsiveness of vascular smooth muscle to nitric oxide.
It is possible that sympathetic-adrenergic vasoconstrictor mechanisms counteracting endothelium-dependent dilation are greater in women compared with men. For example, sympathetic activity may have been greater in this mixed cohort of pre- and postmenopausal women compared with the men based on their higher mean PNE concentrations. Moreover, the slope of the increase in PNE with age trended toward being greater in women than men. As such, a higher sympathetic “background” may have led to a stronger tonic inhibition of brachial FMD. Another possibility is a greater vasoconstrictor influence in women for a given level of tonic sympathetic stimulation. Although some evidence for this exists in middle aged and older women (26, 30), we found no differences in vasoconstriction to α-adrenergic stimulation between premenopausal women and men during ganglionic blockade (7). Furthermore, under basal conditions, young women demonstrate less sympathetic vasoconstriction to exogenous norepinephrine than men and this is due, in part, to higher β-adrenergic-mediated dilation (17, 22). Decreases in β-adrenergic receptor expression and/or affinity with age may potentiate sympathetic vasoconstriction in women. Indeed, β2-adrenergic receptor density is modulated by female sex hormones in vivo (44). Finally, because brachial FMD is mediated by endothelium-synthesized dilating molecules (nitric oxide, prostaglandins, and hyperpolarizing factors), it also is possible that the interaction between sympathetic-adrenergic constrictor signaling and these dilating molecules differs in men and women.
Endothelium-independent dilation and PNE in men.
Although dilation to sublingual nitroglycerin was not related to PNE in women, a modest positive, rather than inverse, relation was observed in men. It is possible that this represents a compensatory response to the suppressive influence of sympathetic activity on brachial artery FMD. If so, it is unclear why a similar response was not observed in women.
Limitations.
The present study used correlation analysis in a large group of healthy adults as an initial probe to determine if vascular endothelial function might be related to sympathetic activity. Functional studies involving inhibition of sympathetic activity and/or α-adrenergic receptor signaling would be required to more definitively assess sex-specific relations between brachial FMD, sympathetic activity, and age. However, such studies are not feasible in a large cohort of subjects, and the present findings serve to provide important initial experimental insight upon which to base future work requiring more invasive procedures.
Individual variables assessed in this analysis, including PNE, only explained a relatively small amount of the total variance in brachial FMD. However, it is difficult to find significant relations between vascular function and factors that potentially modulate that function in large, highly diverse cohorts of human subjects because of 1) the substantial variability between individuals; and 2) the inherent measurement error associated with physiological assessments in humans. Consequently, the present analysis likely underestimates the true physiological significance of the reported relations.
The present study used brachial artery FMD as a noninvasive measure of conduit artery endothelial function (endothelium-dependent dilation) and PNE as a minimally invasive marker of sympathetic activity. Invasive methods are available to assess microvascular endothelial function in humans (i.e., forearm blood flow responses to brachial artery infusion of acetylcholine), and the limitations of interpreting PNE as a measure of sympathetic activity compared with more invasive, direct techniques are widely appreciated (13, 35, 39). For example, PNE concentrations are influenced by the rate of metabolic clearance of norepinephrine. Although norepinephrine clearance is reduced with age in both men and women, there is no evidence that these changes differ between sexes (28, 35, 40), suggesting further that our results were most likely due to differences in norepinephrine appearance and sympathetic activity. Moreover, PNE correlates with more invasive measures of sympathetic activity among healthy adults differing in age (31), and we were able to show relations between brachial FMD, PNE, and age despite such limitations.
Finally, circulating estrogen, which exerts a tonic modulatory effect on endothelial vasodilatory responsiveness (1, 14, 45), was not measured in a sufficient number of the women to assess the potential influence of this factor. However, menopause status, as objectively assessed by follicular stimulating hormone levels, did not affect the strong relation between FMD and PNE in women.
Conclusions.
Our findings provide the first evidence that endothelium-dependent dilation is inversely related to sympathetic activity, as assessed by PNE, among healthy adults varying in age, particularly in women. PNE was the strongest independent predictor of brachial FMD in women in the present study, and correction for PNE abolished the relation between brachial FMD and age in this group. Overall, the present results suggest that sympathetic nervous system activity may represent one of several key factors involved in the modulation of vascular endothelial function with primary aging (36), especially in women.
GRANTS
This study was supported by National Institutes of Health Awards AG-013038, AG-006537, AG-031617, AG-000279, and RR-00051 and American Heart Association 0715735Z.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
REFERENCES
- 1. Adkisson EJ, Casey DP, Beck DT, Gurovich AN, Martin JS, Braith RW. Central, peripheral and resistance arterial reactivity: fluctuates during the phases of the menstrual cycle. Exp Biol Med 235: 111–118, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Braunwald E. Biomarkers in heart failure. Preface. Heart Fail Clin 5: xiii–xiv, 2009 [DOI] [PubMed] [Google Scholar]
- 3. Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, Lloyd JK, Deanfield JE. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 340: 1111–1115, 1992 [DOI] [PubMed] [Google Scholar]
- 4. Celermajer DS, Sorensen KE, Spiegelhalter DJ, Georgakopoulos D, Robinson J, Deanfield JE. Aging is associated with endothelial dysfunction in healthy men years before the age-related decline in women. J Am Coll Cardiol 24: 471–476, 1994 [DOI] [PubMed] [Google Scholar]
- 5. Charkoudian N, Rabbitts JA. Sympathetic neural mechanisms in human cardiovascular health and disease. Mayo Clin Proc 84: 822–830, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chin JH, Azhar S, Hoffman BB. Inactivation of endothelial derived relaxing factor by oxidized lipoproteins. J Clin Invest 89: 10–18, 1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Christou DD, Jones PP, Jordan J, Diedrich A, Robertson D, Seals DR. Women have lower tonic autonomic support of arterial blood pressure and less effective baroreflex buffering than men. Circulation 111: 494–498, 2005 [DOI] [PubMed] [Google Scholar]
- 8. Delp MD, Brown M, Laughlin MH, Hasser EM. Rat aortic vasoreactivity is altered by old age and hindlimb unloading. J Appl Physiol 78: 2079–2079, 1995 [DOI] [PubMed] [Google Scholar]
- 9. Dinenno FA, Jones PP, Seals DR, Tanaka H. Limb blood flow and vascular conductance are reduced with age in healthy humans: relation to elevations in sympathetic nerve activity and declines in oxygen demand. Circulation 100: 164–170, 1999 [DOI] [PubMed] [Google Scholar]
- 10. Donald AE, Halcox JP, Charakida M, Storry C, Wallace SML, Cole TJ, Friberg P, Deanfield JE. Methodological approaches to optimize reproducibility and power in clinical studies of flow-mediated dilation. J Am Coll Cardiol 51: 1959–1964, 2008 [DOI] [PubMed] [Google Scholar]
- 11. Dyson KS, Shoemaker JK, Hughson RL. Effect of acute sympathetic nervous system activation on flow-mediated dilation of brachial artery. Am J Physiol Heart Circ Physiol 290: H1446–H1453, 2006 [DOI] [PubMed] [Google Scholar]
- 12. Eskurza I, Monahan KD, Robinson JA, Seals DR. Effect of acute and chronic ascorbic acid on flow-mediated dilatation with sedentary and physically active human ageing. J Physiol 556: 315–324, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Esler M. The sympathetic system and hypertension. Am J Hypertens 13: 99S–105S, 2000 [DOI] [PubMed] [Google Scholar]
- 14. Gavin KM, Seals DR, Silver AE, Moreau KL. Vascular endothelial estrogen receptor alpha is modulated by estrogen status and related to endothelial function and endothelial nitric oxide synthase in healthy women. J Clin Endocrinol Metab 94: 3513–3520, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harris KF. Interactions between autonomic nervous system activity and endothelial function: a model for the development of cardiovascular disease. Psychosomat Med 66: 153–164, 2004 [DOI] [PubMed] [Google Scholar]
- 16. Harris Ra Nishiyama SK, Wray DW, Richardson RS. Ultrasound assessment of flow-mediated dilation. Hypertension 55: 1075–1085, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hart EC, Charkoudian N, Wallin BG, Curry TB, Eisenach JH, Joyner MJ. Sex differences in sympathetic neural-hemodynamic balance: implications for human blood pressure regulation. Hypertension 53: 571–576, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hijmering ML, Stroes ESG, Olijhoek J, Hutten BA, Blankestijn PJ, Rabelink TJ. Sympathetic activation markedly reduces endothelium-dependent, flow-mediated vasodilation. J Am Coll Cardiol 39: 683–688, 2002 [DOI] [PubMed] [Google Scholar]
- 19. Jablonski KL, Chonchol M, Pierce GL, Walker AE, Seals DR. 25-Hydroxyvitamin D deficiency is associated with inflammation-linked vascular endothelial dysfunction in middle-aged and older adults. Hypertension 57: 63–69, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jablonski KL, Gates PE, Pierce GL, Seals DR. Low dietary sodium intake is associated with enhanced vascular endothelial function in middle-aged and older adults with elevated systolic blood pressure. Ther Adv Cardiovasc Dis 3: 347–356, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jackson DN, Moore AW, Segal SS. Blunting of rapid onset vasodilatation and blood flow restriction in arterioles of exercising skeletal muscle with ageing in male mice. J Physiol 588: 2269–2282, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kneale BJ, Chowienczyk PJ, Brett SE, Coltart DJ, Ritter JM. Gender differences in sensitivity to adrenergic agonists of forearm resistance vasculature. J Am Coll Cardiol 36: 1233–1238, 2000 [DOI] [PubMed] [Google Scholar]
- 23. Lakatta EG. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises. I. Aging arteries: a “set up” for vascular disease. Circulation 107: 139–146, 2003 [DOI] [PubMed] [Google Scholar]
- 24. Lind L, Berglund L, Larsson A, Sundström J. Endothelial function in resistance and conduit arteries and 5-year risk of cardiovascular disease. Circulation 123: 1545–1551, 2011 [DOI] [PubMed] [Google Scholar]
- 25. Lind L, Johansson K, Hall J. The effects of mental stress and the cold pressure test on flow-mediated vasodilation. Blood Pressure 11: 22–27, 2002 [DOI] [PubMed] [Google Scholar]
- 26. Lipsitz LA, Iloputaife I, Gagnon M, Kiely DK, Serrador JM. Enhanced vasoreactivity and its response to antihypertensive therapy in hypertensive elderly women. Hypertension 47: 377–383, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Malpas SC. Sympathetic nervous system overactivity and its role in the development of cardiovascular disease. Physiol Rev 90: 513–557, 2010 [DOI] [PubMed] [Google Scholar]
- 28. Marker JC, Cryer PE, Clutter WE. Simplified measurement of norepinephrine kinetics: application to studies of aging and exercise training. Am J Physiol Endocrinol Metab 267: E380–E387, 1994 [DOI] [PubMed] [Google Scholar]
- 29. Moreau KL, Donato AJ, Tanaka H, Jones PP, Gates PE, Seals DR. Basal leg blood flow in healthy women is related to age and hormone replacement therapy status. J Physiol 547: 309–316, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Narkiewicz K, Phillips BG, Kato M, Hering D, Bieniaszewski L, Somers VK. Gender-selective interaction between aging, blood pressure, and sympathetic nerve activity. Hypertension 45: 522–525, 2005 [DOI] [PubMed] [Google Scholar]
- 31. Ng AV, Callister R, Johnson DG, Seals DR. Age and gender influence muscle sympathetic nerve activity at rest in healthy humans. Hypertension 21: 498–503, 1993 [DOI] [PubMed] [Google Scholar]
- 32. Parker BA, Kalasky MJ, Proctor DN. Evidence for sex differences in cardiovascular aging and adaptive responses to physical activity. Eur J Appl Physiol 110: 235–246, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pierce GL, Eskurza I, Walker AE, Fay TN, Seals DR. Sex-specific effects of habitual aerobic exercise on brachial artery flow-mediated dilation in middle-aged and older adults. Clin Sci 120: 13–23, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, Paffenbarger RS. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol 121: 91–106, 1985 [DOI] [PubMed] [Google Scholar]
- 35. Seals DR, Esler MD. Human ageing and the sympathoadrenal system. J Physiol 528: 407–417, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Seals DR, Jablonski KL, Donato AJ. Aging and vascular endothelial function in humans. Clin Sci 120: 357–375, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sverrisdóttir YB, Jansson LM, Hägg U, Gan LM. Muscle sympathetic nerve activity is related to a surrogate marker of endothelial function in healthy individuals. PLos One 5: e9257–e9257, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Taddei S, Virdis A, Ghiadoni L, Salvetti G, Bernini G, Magagna A, Salvetti A. Age-related reduction of NO availability and oxidative stress in humans. Hypertension 38: 274–279, 2001 [DOI] [PubMed] [Google Scholar]
- 39. Vaz M, Jennings G, Turner A, Cox H, Lambert G, Esler M. Regional sympathetic nervous activity and oxygen consumption in obese normotensive human subjects. Circulation 96: 3423–3429, 1997 [DOI] [PubMed] [Google Scholar]
- 40. Veith RC, Featherstone JA, Linares OA, Halter JB. Age differences in plasma norepinephrine kinetics in humans. J Gerontol 41: 319–319, 1986 [DOI] [PubMed] [Google Scholar]
- 41. Versari D, Daghini E, Virdis A, Ghiadoni L, Taddei S. Endothelial dysfunction as a target for prevention of cardiovascular disease. Diabetes Care 32: Suppl 2: S314–S321, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Virdis a Ghiadoni L, Giannarelli C, Taddei S. Endothelial dysfunction and vascular disease in later life. Maturitas 67: 20–24, 2010 [DOI] [PubMed] [Google Scholar]
- 43. Walker AE, Seibert SM, Donato AJ, Pierce GL, Seals DR. Vascular endothelial function is related to white blood cell count and myeloperoxidase among healthy middle-aged and older adults. Hypertension 55: 363–369, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wheeldon NM, Newnham DM, Coutie WJ, Peters JA, McDevitt DG, Lipworth BJ. Influence of sex-steroid hormones on the regulation of lymphocyte beta 2-adrenoceptors during the menstrual cycle. Br J Clin Pharmacol 37: 583–588, 1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Williams MR, Westerman RA, Kingwell BA, Paige J, Blombery PA, Sudhir K, Komesaroff PA. Variations in endothelial function and arterial compliance during the menstrual cycle. J Clin Endocrinol Metab 86: 5389–5395, 2001 [DOI] [PubMed] [Google Scholar]
- 46. Yeboah J, Crouse JR, Hsu FC, Burke GL, Herrington DM. Brachial flow-mediated dilation predicts incident cardiovascular events in older adults: the Cardiovascular Health Study. Circulation 115: 2390–2397, 2007 [DOI] [PubMed] [Google Scholar]
- 47. Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, Post W, Lima JA, Crouse JR, Herrington DM. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the multi-ethnic study of atherosclerosis. Circulation 120: 502–502, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ziegler MG, Lake CR, Kopin IJ. Plasma noradrenaline increases with age. Nature 261: 333–335, 1976 [DOI] [PubMed] [Google Scholar]