Abstract
It is advantageous for a clinician to understand how patients feel about their initial encounters, but it can be difficult to discern what is and what is not working. This qualitative, exploratory study is guided by the question, “What happens during an initial mental health encounter between a Black patient and a non-Black provider that leads the patient to describe it as a good or poor experience?” The findings are based on face to face, postintake interviews with 14 Black patients seen by 11 non-Black providers as part of the Patient-Provider Encounter Study (PPES). The objective is to explore the initial interpersonal interactions between Black patients and their non-Black mental health providers and to better understand how patients come to describe the encounter as good (favorable) or poor (unfavorable). A framework inclusive of 5 specific elements is introduced that maps the patient’s conceptualization process about how judgments are made about the encounter. Due to the naturalistic and exploratory nature of the study, a research hypothesis was not established. Instead, we observed how patients scanned the interaction with the provider, made assessments about their provider, and determined whether their experience was positive or negative. The implications of these findings will help to improve the interactions in mental health settings between minority patients and their providers.
Keywords: African American mental health, race concordance, healthy cultural paranoia, scanning, Patient-Provider Encounter Study
The importance of matching a patient and provider by their racial backgrounds (i.e., race concordance) remains inconsistent and not well understood. The available evidence has not paid enough attention to important factors like patient-level variables, which could also influence treatment outcomes (Chang & Berk, 2009; Meghani et al., 2009). Research supporting race concordance suggests that when Black patients are treated by Black providers, they report positive treatment outcomes. Specifically, the encounter is collaborative and Black patients are satisfied, more likely to retain in care, and more likely to adhere to their treatment plans (Cooper-Patrick et al., 1999; LaVeist & Nuru-Jeter, 2002; LaVeist, Nuru-Jeter, & Jones, 2003). Studies also show that when Black patients are treated by Black therapists, they feel more accepted, understood, and perceive the provider to be more culturally sensitive (Thompson Sanders & Alexander, 2006). Patients observe subtle cues during the interaction to make determinations about their provider’s ability to be sensitive to their culture, thus implying that Black providers could be more culturally sensitive to Black patients (Thompson Sanders, Bazile, & Akbar, 2004). However, Black providers are limited in numbers and thus are not widely available to serve Black patients. Specifically, Black professionals make up only 2.6% of mental health clinicians in the United States (American Medical News, 2001), which is low considering that approximately 20% of Black Americans seek mental health specialty treatment within a 12-month period (Neighbors et al., 2007). Therefore, there is an urgent need to better understand the experiences of Black patients who receive treatment from non-Black providers (i.e., racially discordant clinical encounters).
It may also be important for the patient and provider to be cognitively matched according to shared values, attitudes, and expectations about treatment, and not solely by their race or ethnicity (Gaston, 1990). Zane and colleagues (2005) prospectively examined whether cognitive match in problem perception, coping orientation, and treatment goals would be predictive of greater session impact and better treatment outcomes. The researchers found that when patients and providers were both cognitively and ethnically matched, patients were more relaxed, comfortable, positive, and engaged during sessions than patients who were only cognitively matched to providers. Findings like this underscore the value of cognitive connections and how vital it is for clinicians to have prior knowledge about how a patient feels about entering into an initial clinical encounter. However, understanding what is or is not working for the patient can still be difficult to discern. This may be especially challenging when providing treatment for Black patients, in particular, because they may exercise a level of caution, skepticism, or self-preservation concerning how they are treated by the provider (also referred to as health cultural paranoia) as a result of previous perceptions of negative, discriminatory, or racist interactions within racially discordant clinical encounters (Ridley, 1984). When examining the problems of nondisclosing Black patients who had seen White therapists for psychotherapy, Ridley (1984) suggested, “while self-disclosure is generally considered essential for maximizing therapeutic outcomes, complex interpersonal and social factors often affect the Black client’s level of self-disclosure” (p.1234). More than a decade later, healthy cultural paranoia (sometimes interchangeable with “cultural mistrust”) continues to be included in studies that seek to explain observations of skepticism or reservation for Black patients within mental health treatment settings (Terrell & Terrell, 1981; Whaley, 1997, 1998, 2001a, 2001b).
The challenge is to improve racially discordant clinical interactions before the patient exits care so as to ensure the possibility of a positive second visit. To date, few studies have specifically examined racially discordant clinical encounters. Moreover, the available race-concordant evidence has certain limitations. First, a substantial portion of the literature focuses on patients in primary care settings, and we cannot assume that the same observations would occur within mental health settings. Second, these studies have relied on questionnaires and instruments that have neglected to explore the qualitative aspects of the patient-provider interactions. Finally, compared to an emphasis on the provider’s contribution to the clinical encounter, studies that explore the patient’s perceptions and reactions during the clinical interaction are rare. Few studies have been able to include actual examples of patients reflecting on how they processed their experiences with their racially discordant providers. Obtaining the perspective of the client about care has been shown to directly influence treatment outcomes (Horvath & Bedi, 2002). Therefore, the objective of this study is to use data from the Patient and Provider Encounter Study (PPES; Alegría et al., 2008) to address some of these limitations. We use semistructured interview data to explore the interactions between Black patients and their non-Black mental health providers to better understand how they come to describe the initial encounter as good (favorable) or poor (unfavorable). This exploratory study is motivated by observations of how Black patients reflected on their initial mental health encounter with non-Black providers, as well as reporting on primary interests of the PPES--the process of diagnostic assessment. Based on these observations, the current study is guided by the following question: What happens during an initial mental health encounter between a Black patient and a non-Black provider that leads the patient to describe it as a good or poor experience?
Method
Patient-Provider Encounter Study Sample
We report postinitial mental health intake interview data from the Patient-Provider Encounter Study (PPES; Alegría et al., 2008). The current study specifically focuses on the Black patient sample, but overall, the PPES includes 129 patient and provider interview dyads. More specifically, the convenience sample included 129 patients and 47 clinicians. In order to allow for variation, no provider participated in the study more than five times. Most patients were 18–49 years old (n=102, 80%), female (n=77, 60%), had completed high school (n=83, 65%), had a household income below $15,000 (n=81, 64%), and were not working (n=70, 54%). Approximately 50% of the patient sample was Latino, 30% was non-Latino White, and 11% was Black. Interviews began in March 2006 and ended in March 2008. Participants were recruited from eight, public safety-net, outpatient mental health clinics in the Northeastern United States. Institutional Review Board approval was obtained for each clinic. All clinics were based in large urban areas and nested within local community settings. In order to maintain confidentiality, unique identifiers were assigned to patient cases. The names and locations of the clinics are not disclosed in this article.
Patients seeking an initial mental health intake evaluation were eligible to participate. An “initial” intake was defined as an evaluation either of a new patient to the clinic or of an established patient who came in to be reevaluated because he or she was absent for mental health treatment for at least 3 consecutive months. The majority of patients were not entirely new to the system, with approximately 84% reporting previous mental health treatment. Since patients were recruited prior to seeing the providers, a capacity to consent screen (Zayas, Cabassa, & Perez, 2005) was administered to ensure that they were able to provide informed consent to the study. Patients who were identified as psychotic or suicidal, required an interpreter, or who could not demonstrate capacity to consent were not eligible to participate.
Current Study Sample
The current study includes postintake interview data from 14 Black patients who were seen by 11 non-Black providers. Patients self-identified as being Black (not of Spanish or Hispanic heritage). The term Black refers to persons born of African descent currently living in the United States, including Africans, African Americans and non-Spanish speaking Caribbean Blacks. Although the PPES Black patient sample includes a total of 17 individuals, three individuals who self-identified as being of Hispanic or Latino backgrounds were excluded from this analysis to prevent confounding race with ethnicity.
Participants of our sample were between 20 and 63 years old, with the median age of 47 years. The majority of the Black sample completed high school (71.4%) and reported an average annual household income of $33,154. Comorbid symptomatology was common, with either depression or at least one anxiety disorder being assessed for 57% of the Black participants and substance use/dependence disorders being reported by the provider for 36% percent of the sample. Of the 11 providers who saw Black patients, four were psychiatrists, four were social workers, two were psychiatric nurses, and one was a psychologist. Based on self-reports, nine were white, one was Asian, and one was Hispanic/Latino. Three of the 11 providers saw more than one patient.
Procedures
After the initial clinical intake session, separate interviews were conducted using a semi-structured interview protocol. The semistructured interview protocol was designed to invite patients to reflect on their experiences during the intake visit. The questions focused on the presenting problem, rapport with providers, and the significance of socio-cultural factors on their perception of the clinical interaction with the provider. Additional details about the PPES interview process have been published elsewhere (Katz & Alegría, 2009). Postintake interviews lasted approximately 30 min, were audiotaped, and later transcribed by a professional service. Interviews were conducted by two female research assistants who were in their mid-twenties and of Puerto Rican descent. Throughout the data collection process, qualitative interview supervision and trainings were provided on a weekly basis by the PPES senior consultant in qualitative research. All members of the PPES research team, including the two research assistants noted in this study, were required to participate. Proficiency in conducting qualitative interviews was evaluated formatively as a result of this continuous evaluation and review process as well as by review of audiotapes and transcribed transcripts. Patient postintake interviews began with questions to patients about their reasons for seeking treatment, their interactions with the provider, and concerns that they felt had not been addressed during the intake session. Subsequent questions asked the patients to share what they thought was most important about who they were as individuals and ended with a question seeking advice that they would give to providers on how to build relationships with others similar to them. Additional probes were available to obtain more information throughout the interview process. All participants provided written informed consent to the audiotaping of the postintake interviews and to the publication of the results, including the blinded quotes. The PPES patient interview guide can be obtained from the first author.
Conceptual Framework and Analysis
Originally, PPES researchers planned to use the postintake patient interview to aid in understanding how information shared in the intake interview informed the diagnostic assessment (Alegría et al., 2008). In other words, the patient’s perception of the quality of the interpersonal interaction was not the only topic of interest. The goal of the training and the open-ended, narrative format of the study invited patients to reflect on their experiences, which seemed to expand their descriptions beyond the closed-ended reports from the literature we explored regarding race concordance and ethnic matching. We started with open coding to identify thematic content areas within the transcribed interviews. Theme development and segment coding proceeded in an iterative process. First, the professionally transcribed interviews were read in their entirety by two independent coders. In discussing the initial rounds of coding, we were struck by how Black patients described their interactions with providers and how these interactions seemed to be informed by previous experiences, acknowledgement of racial or cultural similarities or differences, and instances of what has been referred to as healthy cultural paranoia (i.e., being skeptical, cautious or guarded). For instance, while reporting their general satisfaction with the providers, Black patients also talked about what they had been looking for during the encounter, in order to determine whether it was a good (favorable) or poor (unfavorable) experience.
Before initiating a more focused round of coding, we returned to the literature seeking guidance on the patients’ reflections of the initial clinical encounter. We discovered Atdjian and Vega’s (2005) concept of scanning within psychiatric settings. The authors suggest that when patients, especially those of racial and ethnic backgrounds, meet with providers, they simultaneously monitor the encounter (i.e., scan) for certain cues to ascertain how they feel about the interaction. Specifically, they scan to determine their feelings of (a) comfort with the provider, (b) safety in disclosing personal information, (c) trust for the provider, and (d) being listened to and understood by the provider. Atdjian and Vega (2005) argue that “important cues” derive from “reading material in the waiting room, the demeanor and diversity of the support staff, the receptivity to accompanying family members, and the verbal and nonverbal communication of the psychiatrist” (p. 1600). Taken together, these observations inform the patients’ judgments of the totality of that clinical experience.
While Atdjian and Vega’s concept of scanning captured a good deal of the reflective activity we observed during our coding process, it did not capture everything. We noticed that patients sometimes used the word “respect,” which has particular relevance for the Black community. Therefore, in order to better understand the manner in which the term related to the interaction with the provider, we amended their concept with a fifth dimension that captured interview segments in which patients used the term “respect.” After extensive discussions and consensus about the final set of codes to be analyzed in this study, we used NVivo 7 software (QSR International Pty Ltd., 2006) to sort the coded data by frequency of occurrence.
Results
Every patient (100%) talked about a previous experience. Descriptions of previous experiences were from prior health or mental health care or from nontreatment-related social interactions with others. Approximately 86% (n=12) reported previous mental health treatment. Approximately 71% reported that they felt listened to and understood and also trustful of the provider. Sixty-four percent talked about feeling safe to disclose personal information to the provider, and 57% of the patients described feelings of comfort with the non-Black provider during the encounter. The remaining thematic categories discussed during the postintake interviews were issues related to healthy cultural paranoia (43%) and to feeling respected by the provider (36%).
The following reports exemplar text to describe the thematic categories we formulated to describe how Black patients scanned during the initial mental health encounter with non-Black providers.
Feeling Comfortable With the Provider
Scanning to assess for feelings of comfort was as much a nonverbal process as it was a verbal one. For example, one patient talks about judging his provider by “watching” him:
I’m a very good judge of character. I can tell, I mean, I was watching him just like he was watching me…he made me feel comfortable and he was comfortable…it’s not so much that it’s important in how people react to me, but it’s very obvious to me when people do react to me in certain ways… If he didn’t know what he was doing I would have known. …He just has the compassion…it was real, I feel good about him, I respect him. (Patient 315)
From the statement “it’s very obvious to me when people do react to me in certain ways,” we might assume that this man has had some type of experience that offers him a negative template against which he is able to assess whether this particular provider is reacting to him in the same way. Although the patient does not provide overt details, by “watching” the provider, he scans and then reacts to the provider’s “compassionate” behavior in a way that allows him to conclude that he feels good, comfortable, and respectful of the provider.
In the next example, the patient clearly feels uncomfortable and betrayed (i.e., disrespected) by the provider’s behavior:
I didn’t feel like he put his job on the line, you know what I mean? Like it was my job to do…I know he tried to do what he was supposed to do, but I felt uncomfortable with him ‘cause, he didn’t give me that 110%… I’m just trying to find the right words. Know how some people work a job and some people work for paychecks, he worked for the paycheck … I just felt betrayed, we’re both suppose to be on this mission together and he did a half ass job…I would not return back if you paid me to. (Patient 450)
The concept of working a job as opposed to working for a paycheck was an effective metaphor to describe the discontent felt by this patient. The patient enters the encounter with certain expectations that were clearly not shared by the provider; his scanning detects this, and ultimately, he determines that the provider’s poor investment does not warrant his return for subsequent treatment.
Feeling Safe to Disclose Personal Information
When patients talked about feeling safe to disclose personal information, they wanted to express themselves and tell their stories without being interrupted by providers. They also wanted to have the providers’ attention as they freely shared personal or sensitive information. In the following example, the patient uses a previous poor experience to explain why she sensed (i.e., through scanning) that she would be able to safely disclose information to her current provider:
…she just asked me why am I here and, I told her…I just started talking and then I couldn’t shut up. (Laughter) And that’s another thing that you can sense about a person.…she made me feel real good…she made me feel like I can talk to her about anything… it’s about (letting) that person in front of you get out what they need to get out at that time; and that’s how she was…I remember an incident where, (clears throat) a psychiatrist mind you, um, I was sitting there, you know, talking out my problems with him and he’s sitting there watching the clock… I shut down. I was like ‘oh, okay, well, you know, um, I see you’re, you’re not (listening), our session is over…then he says to me, “do you feel good?”…he didn’t care… (Patient 411)
Feeling Trustful of the Provider
As patients scanned for feelings of trust for providers, they frequently referenced negative experiences (within or outside of clinical treatment) in order to explain what the current provider had done differently to make them feel good about the encounter. For instance, in the following example, the patient had been previously mistreated, which led him to come to the current encounter fairly guarded (i.e., healthy cultural paranoia). Consequently, during the initial encounter, he scanned to determine if the current provider would be similar to his previous provider:
I don’t trust no one… when I was hospitalized the first time they treated me wrong… Some people just don’t care about people; they just care about their paychecks… I never wanted to come here because (of) how they mistreated me (referring to the previous facility)… she (the current provider) wasn’t insulting me… she wasn’t just seeing it from her point of view; she was putting herself in my shoes. (Patient 608)
Similarly, another patient implicitly uses an example from a previous nonclinical experience to explain why he felt that he could trust and respect his current provider.
Just be straight, you know, speak (to) and treat me just like you’re talking to any other man. You don’t have to be careful with me. Don’t treat me like, ‘I got to be careful with him, he’s Black’. Just talk to me, just like any other man, because if you be careful with me, I’m going to feel it, I’m going to know you’re doing it. Don’t give me that, ‘hey buddy.’ I don’t need that, let’s just be straight. That’s what he (the provider) was doing with me… I feel good about him, I trust and respect him and I think he respects me…(Patient 411)
Feeling Listened to and Understood by the Provider
In order to determine that providers were listening to and understanding them and their reasons for presenting for treatment, patients scanned the providers’ body language and facial expressions. For example:
Interviewer: What would make you know he understood (you)?
Patient: By the expression on his face. I think he, you know, understands …he was really looking at me hard.
Interviewer: When you say expression on his face, what does that look like?
Patient: Like he was saying ‘oh, really.’ And like he’s really concerned about what I’m saying. I could tell he wanted to hear more… (Patient 406)
Feeling Respected by the Provider
Feelings of respect were described as a consequence of an action or observation that patients made about their providers. Although, as illustrated below, it can be difficult to define and articulate, these feelings seem to enable the patient to feel as if the provider withheld judgment.
It’s hard to explain (responding to a probe from the interviewer to elaborate on a previous statement)…be as empathetic as you can, because it’s different for everybody, and everybody goes through different stuff…just be patient, be respectful, be attentive…cause if you don’t…they’re (referring to other patients, in general) not gonna be more open…it’s hard for an African-American to do things and not feel like we’re kind of a statistic. I’m not asking for her (referring to her provider) to be my friend. (I just want her to) be respectful towards me, um, not be judgmental. (Patient 435)
In the same way, coming from an initial encounter where the interpersonal interaction was unfavorable (poor), patient 450 scanned the actions of his provider to conclude that what he gave had not been reciprocated:
Patient: I wouldn’t, I told him I couldn’t work with him…this Black man, wants respect-good respect, and don’t disrespect me.
Interviewer: What does respect mean? A lot of people talk about respect. I want to make sure that I understand, what does that mean (to you)?
Patient: What I give you I want back.
Interviewer: (following up on a comment made by the patient earlier in the interview): So you came in giving 110 percent and you felt that he was giving half?
Patient: Like I said, on a scale of 1 to 10, (he gave) like a 6, 6 1/2. (Patient 450)
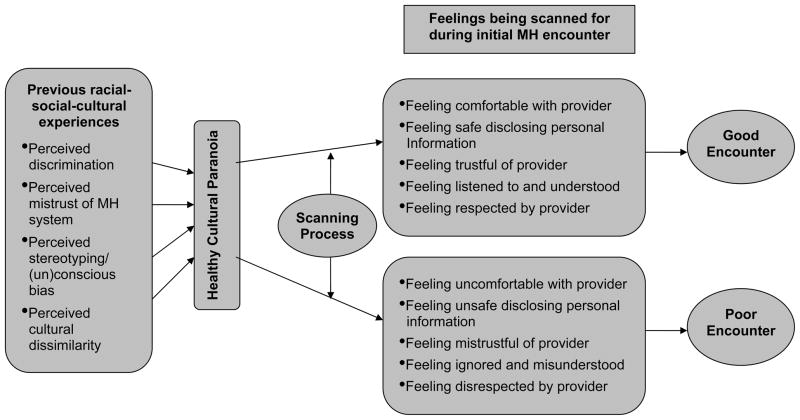
Mapping the process
As a result of our analysis, the following framework (Figure 1) was developed to serve as a conceptual map or blueprint that explains how patients seemed to process their perceptions, feelings, and thoughts during the encounter. Black patients entered the initial mental health encounter with previous experiences (both within and outside of treatment) such as discrimination, mistrust of the mental health system, stereotyping, bias and cultural dissimilarity, all of which may have prompted them to be cautious, skeptical, or to exhibit healthy cultural paranoia. This in turn serves as an existing conceptualization of “scanning” through which patients assess feelings of comfort, safety to disclose personal information, trust with the provider, and being listened to, understood, and respected by the provider. The cumulative result of such impressions is a determination about whether the encounter is favorable (“good”) or unfavorable (“poor”).
Figure 1.
Conceptual framework: Black patients’ interpersonal processing during the initial mental health encounter.
Discussion
Prospective Black patients interacted with their non-Black providers exercising caution and skepticism. Their previously established levels of healthy cultural paranoia seemed to function as a filter through which the present encounter was viewed. Black patients simultaneously engaged in and “scanned” the encounter for feelings of comfort, safety in disclosing personal information, being trustful of the provider, and being listened to, understood, and respected by the provider. For some patients, judgments about the initial encounter seem to have less to do with clinical expertise or experience of the provider and more with perceptions of empathy and the quality of the interpersonal connection between the two individuals. This was demonstrated with statements like, if he didn’t know what he was doing I would have known, he just has the compassion …it was real, or when they reported feeling “betrayed,” because they felt disrespected by a provider, and when a simple facial expression could lead to the patient to “feel understood” by the provider. Although we focused on patients’ perceptions, our findings suggested that the initial mental health encounter is an opportunity for both the patients and providers to “audition” for the opportunity to work together. If the patient feels that the provider’s performance is subpar, the clinician’s attempts to understand the situation will be superfluous, because the patient may have already made up his or her mind to disengage from the interaction.
Achieving Good Initial Mental Health Encounters
While the previous literature has demonstrated the advantages of race concordance (Cooper-Patrick et al., 1999; LaVeist & Nuru-Jeter, 2002; LaVeist et al., 2003; Saha, Komaromy, Koepsell, & Bindman, 1999), based on our findings, achieving good racially discordant encounters is also possible. However, in order for this to occur, Black patients need to feel comfortable, safe, able to trust the provider, listened to, understood, and respected by the provider. “Feeling out” or scanning a provider should not be considered a display of difficulty or resistance. Instead, it is probable that our analysis demonstrates, through the process of scanning, how healthy cultural paranoia or cultural mistrust may operate for Black patients (Terrell & Terrell, 1981; Whaley, 1997, 1998, 2001a, 2001b). The behavior should be interpreted as an act of self-preservation and be considered a strength or sign of resilience and not as pathology. For instance, when respondents say, “this Black man wants respect, good respect,” or “she wasn’t insulting me,” or “don’t treat me like, ‘I got to be careful with him, he’s Black,’ you know, just talk to me just like any other man…”, we cannot minimize or overlook what this means for Black patients, especially within mental health settings.
Upon reflecting on the process of developing the African American section of the U.S. Surgeon General’s supplemental report on mental health, Snowden (2003) explains how collectively Blacks have faced issues of racism and discrimination that affects many aspects of their lives, including their perceptions of and willingness to engage in mental health treatment. This underscores the need for more research to examine how residual effects of discrimination, mistrust of the mental health system, stereotyping, bias, and cultural dissimilarities could affect racial and ethnic minorities as they attempt to interpersonally engage in treatment with providers from differing backgrounds.
Limitations
Several limitations should be considered when interpreting these findings. First, we only examined a total of 14 cases of Blacks in the Northeast United States. Our findings might have been different if we had a larger sample of Blacks from other geographic regions. Also, we were unable to explore for different perceptions of the initial mental health by subgroup diversity heterogeneity within our Black patient sample. Future research should examine for diversity within the Black community and include diverse geographic regions, clinical, and socioeconomic settings.
Secondly, we only had one opportunity to interview patients immediately after the initial mental health intake. Had we been able to conduct follow up interviews, we may have been able to further develop the thematic categories. Thirdly, few patients talked extensively about poor or negative experiences during the initial encounter. This could be explained in a variety of ways. For instance, it is possible that poor or negative experiences did not exist for patients, or some patients did not feel comfortable or familiar enough with the interviewer to share this type of information. Although the confidentiality of the information shared was strongly emphasized during the informed consent process, it is possible that some patients could have had concerns about the impact on their treatment of sharing this type of information.
Fourthly, we examined postintake patient descriptions of the interaction with the provider rather than directly observed interactions, which would have yielded more information about the provider’s behavior during the session. Investigations that explain the ways in which specific actions or behaviors from the provider influence the patient’s perception of the interaction are logical next steps for this area of research. Finally, it is important to mention that when we speak about Black patients, the intent is not to have these data serve as what we might expect from every Black patient, but instead provide examples of how patients reflected on these initial mental health encounters.
Recommendations for Improving Encounters
This information might help providers and clinical supervisors better understand what needs to happen between a Black patient and a non-Black provider for the patient to feel good about the initial mental health encounter. As previously mentioned, knowing exactly what to do during a clinical encounter can be challenging, so training non-Black providers to facilitate a race-discordant positive experience is salient. We learned that Black patients instinctively integrate experiences from previous social or clinical interactions to appraise the current encounter. Future research should specifically test whether investigating previous negative clinical experiences improves subsequent patient and provider interpersonal interactions. The discovery of what might have been a negative clinical experience for the patient could inform mental health providers about how to avoid them. For example, one way for providers to efficiently understand reservations a minority patient may have about mental health treatment is to start the encounter by specifically asking about any previous negative clinical experiences. This process could enable the provider to obtain clues about the patient’s prior experiences, expectations, or attitudes about being in care. Such clues can provide pertinent information that allows providers to effectively match and cognitively engage with this individual, even in the absence of race/ethnic concordance (Zane et al., 2005).
There are also aspects of the clinical environment being scanned by patients that may have implications for clinics or agencies (Atdjian & Vega, 2005). For instance, creating a warm and welcoming clinical environment can be just as important as the patient and provider’s relationship. For patients, particularly those of racial and ethnic backgrounds, important cues emerge from sources such as the reading material in the waiting room, the demeanor and diversity of the support staff, and the receptivity to accompanying family members (Atdjian & Vega, 2005). Ongoing staff trainings and supervision that specifically address barriers to treatment engagement and cultural mistrust are additional resources that could assist in achieving good clinical encounters.
To some, these recommendations may seem obvious or too simple, yet if we consider the countless reports of poor patient treatment engagement, adherence, and retention, we cannot deny the need for change. Having patients, especially minority patients, disclose important information during the initial clinical encounters could prevent poor interpersonal interactions that leave patients feeling uncomfortable, unsafe, mistrustful, disrespected, and skeptical about their mental health care.
Acknowledgments
The Patient-Provider Encounter Study data used in this analysis was provided by the Advanced Center for Latino and Mental Health Systems Research of the Center for Multicultural Mental Health Research at the Cambridge Health Alliance. This study was supported by NIH Research Grant P50 MHO 73469-01 funded by the National Institute of Mental Health, Minority/Diversity Supplement to Grant P50 MH73469 (NIMH) and P60 MDO 02261 (NCMHD) funded by the National Center for Minority Health and Health Disparities.
The authors also thank Kim Hopper, Elliot G. Mishler, and Peter Guarnarccia for their invaluable comments and feedback on earlier versions of this article.
Contributor Information
Tara R. Earl, Boston College
Margarita Alegria, Harvard Medical School.
Frances Mendieta, Loyola University.
Yaminette Diaz Linhart, Boston University.
References
- Alegría M, Nakash O, Lapatin S, Oddo V, Gao S, Lin J, Normand S. How missing information in diagnosis can lead to disparities in the clinical encounter. Journal of Public Health Management and Practice. 2008;14:S26–S35. doi: 10.1097/01.PHH.0000338384.82436.0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Medical Association physician characteristics and distribution in the US, 2001–2002. American Medical News; 2001. Retrieved from http://www.amednews.com/2001/prsa0903. [Google Scholar]
- Atdjian S, Vega W. Disparities in mental health treatment in U.S. racial and ethnic minority groups: Implications for psychiatrists. Psychiatric Services. 2005;56:1600–1602. doi: 10.1176/appi.ps.56.12.1600. [DOI] [PubMed] [Google Scholar]
- Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, Ford DE. Race, gender, and partnership in the patient-physician relationship. The Journal of the American Medical Association. 1999;282:583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- Gaston L. The concept of the alliance and its role in psychotherapy: Theoretical and empirical considerations. Psychotherapy. 1990;27:143–153. [Google Scholar]
- Katz A, Alegría M. The clinical encounter as local moral world: Shifts of assumptions and transformation in relational context. Social Science & Medicine. 2009;68:1238–1246. doi: 10.1016/j.socscimed.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? Journal of Health and Social Behavior. 2002;43:296–306. [PubMed] [Google Scholar]
- LaVeist TA, Nuru-Jeter A, Jones KE. The association of doctor-patient race concordance with health services utilization. Journal of Public Health Policy. 2003;24:312–323. [PubMed] [Google Scholar]
- Meghani S, Brooks J, Gipson-Jones T, Waite R, Whitfield-Harris L, Deatrick J. Patient-provider race concordance: Does it matter in improving minority patients’ health outcomes. Ethnicity & Health. 2009;14:107–130. doi: 10.1080/13557850802227031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors HW, Caldwell C, Williams DR, Nesse R, Taylor RJ, Bullard KM, Jackson JS. Race, ethnicity, and the use of services for mental disorders: Results from the national survey of American life. Archives of General Psychiatry. 2007;64:485–494. doi: 10.1001/archpsyc.64.4.485. [DOI] [PubMed] [Google Scholar]
- NVivo7 (Computer software) Doncaster, Victoria 3108 Australia: QSR International Pty Ltd; [Google Scholar]
- Ridley CR. Clinical treatment of the nondisclosing Black client. A therapeutic paradox. The American Psychologist. 1984;39:1234–1244. doi: 10.1037//0003-066x.39.11.1234. [DOI] [PubMed] [Google Scholar]
- Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine. 1999;159:997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- Snowden LR. Challenges to consensus in preparing the supplement to the surgeon general’s report on mental health. Culture, Medicine and Psychiatry. 2003;27:409–418. doi: 10.1023/b:medi.0000005480.75504.4b. [DOI] [PubMed] [Google Scholar]
- Terrell F, Terrell S. An inventory to measure cultural mistrust among blacks. Western Journal of Black Studies. 1981;5:180–184. [Google Scholar]
- Whaley A. Ethnicity/race, paranoia, and psychiatric diagnoses: Clinician bias versus sociocultural differences. Journal of Psychopathology and Behavioral Assessment. 1997;19:1–20. doi: 10.1007/BF02263226. [DOI] [Google Scholar]
- Whaley A. Cross-cultural perspective on paranoia: A focus on the Black American experience. Psychiatric Quarterly. 1998;69:325–343. doi: 10.1023/A:1022134231763. [DOI] [PubMed] [Google Scholar]
- Whaley A. Cultural mistrust and mental health services for African Americans: A review and meta-analysis. The Counseling Psychologist. 2001a;29:513–531. doi: 10.1177/0011000001294003. [DOI] [Google Scholar]
- Whaley A. Cultural mistrust of white mental health clinicians among African Americans with severe mental illness. The American Journal of Orthopsychiatry. 2001b;71:252–256. doi: 10.1037/0002-9432.71.2.252. [DOI] [PubMed] [Google Scholar]
- Zane N, Sue S, Chang J, Huang L, Huang J, Lowe S, Lee E. Beyond ethnic match: Effects of client-therapist cognitive match in problem perception, coping orientation, and therapy goals on treatment outcomes. Journal of Community Psychology. 2005;33:569–585. doi: 10.1002/jcop.20067. [DOI] [Google Scholar]
- Zayas L, Cabassa L, Perez M. Capacity-to-consent in psychiatric research: Development and preliminary testing of a screening tool. Research on Social Work Practice. 2005;15:545–556. doi: 10.1177/1049731505275867. [DOI] [Google Scholar]