Abstract
Background:
Limited studies have been published so far, which revealed the association of different types of smokeless tobacco on various periodontal health indicators, including mobility and furcation, on North Indian population. The present study has been undertaken to evaluate the effects of commonly used smokeless tobacco forms on periodontal health in Lucknow, North India.
Methods:
This cross-sectional study investigated the effect of commonly used smokeless tobacco on periodontal health in local population of Lucknow, for which 2045 individuals were evaluated. Amongst them, 1069 individuals were found to be using some kind of tobacco; amongst the tobacco users, n=122 were smokers, n=657 were only using only smokeless tobacco and n=290 were using both smokeless tobacco as well as tobacco in smoking form. After completing the questionnaire, all the participants underwent clinical examination for the various clinical parameters.
Results:
The impact of smokeless form of tobacco use was significantly higher on all the periodontal health indicators, viz., plaque index, gingival index, calculus, clinical attachment loss, gingival recession, mobility, furcation, lesion, and probing pocket depth. Both duration and frequency of smokeless tobacco use significantly affected the periodontal health.
Conclusion:
The periodontal health of the general population in the region required immediate attention as majority of subjects irrespective of their habit status had onset of clinical attachment loss and gingival recession, more so amongst the smokeless tobacco users than smoking form of tobacco as well as than from non-tobacco users.
Keywords: Gul, oral hygiene status, Paan (betel quid), smokeless tobacco
INTRODUCTION
The relationship between smoking and oral health is known to all; its ill effect on periodontal tissues has also gained scientific evidence. In addition to smoking, smokeless tobacco has also evidently shown its effect on various oral tissues. Smokeless tobacco products have been in existence for thousands of years among populations in South America and Southeast Asia in varied forms such as Khaini, Gutkha, moist plug, Toombak, etc. Over time, these products have gained popularity throughout the world. Smokeless tobacco is consumed without burning the product and can be used orally and through nasal route. Oral smokeless tobacco products are placed in the mouth, cheek or lip and sucked (dipped) or chewed.[1]
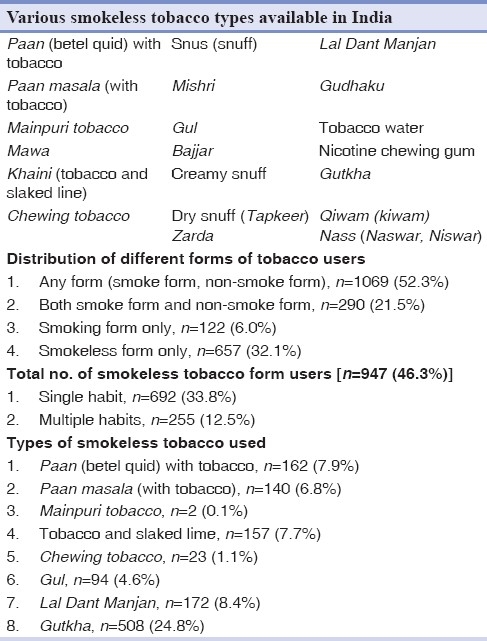
Epidemiological and clinical studies in various parts of the world with demographic variations have shown the effect of smokeless tobacco on oral tissues, and on periodontal health. Monten et al.[2] and Frithiof et al.[3] have shown the effects of “snuff” (moist or dry) on periodontal tissues. It has been seen that there are about 20 different smokeless tobacco forms available in India [Table 1]. Out of these, eight types of smokeless tobacco are commonly used in North India. Limited studies have been published so far, which revealed the association of different types of smokeless tobacco on various periodontal health indicators, including mobility and furcation, on North Indian population. Kumar et al.[4] had shown a significant impact on the severity of periodontal diseases among tobacco users as compared to non-users and the risk of periodontal pockets increased as the duration and frequency of tobacco consumption increased amongst the green marble mine laborers of Rajasthan in a population sample of 585, belonging to lower socioeconomic strata. Sood[5] also revealed higher prevalence of periodontal disease in different smokeless tobacco users; however, they did not consider the gingival recession (GR), mobility and furcation involvement as well as severity of loss of attachment and calculus. The present study has been undertaken to evaluate the effects of commonly used smokeless tobacco forms on periodontal health in Lucknow, India.
Table 1.
Various smokeless tobacco types available in India and distribution of various forms of tobacco users
MATERIALS AND METHODS
This cross-sectional study investigated the effect of commonly used smokeless tobacco on periodontal health in local population of Lucknow, for which 2045 individuals [males=1455 (71%), females=590 (28.9%)] were evaluated. Amongst them, 1069 individuals were found to be using some kind of tobacco; amongst the tobacco users, n=122 were smokers, n=657 were using only smokeless tobacco and n=290 were using both smokeless tobacco as well as tobacco in smoking form. Population of patients attending the outpatient department of Saraswati Dental College and Hospital, Lucknow, and the camps organized in schools, local community centers and nearby villages participated in the study.
Inclusion criteria
Population in the age group of 10-60 years (mean age =32.81±11.74 years) was evaluated. Dentate patients with at least one mandibular and one maxillary tooth on both sides of arch (both males and females) were included.
Questionnaire
After obtaining ethical clearance from local ethical committee, a questionnaire was distributed to all the participants and they were asked to complete it. The questionnaire included patient's demographics, routine oral hygiene practices, history of past and present tobacco use (current users, former users and non-users), duration (in years) and quantity (in packs) of smokeless tobacco used, location and duration of smokeless tobacco placement in mouth.
Clinical examination
All the participants (n=2045) received an oral examination using diagnostics (mouth mirror, explorer, UNC 15 probe, cotton pliers and Naber's probe) instruments and the following parameters were assessed for any lesion/smokeless tobacco keratosis at cheek mucosa, vestibules, floor of mouth and palate. Plaque index[6] (PI) was assessed using mouth mirror and a dental explorer after air drying of teeth to assess plaque on Ramfjord teeth (16, 12, 24, 36, 32, 44) scoring four surfaces per tooth. When a designated tooth was missing, the closest tooth distal to the missing tooth was assessed.
Calculus index was measured using visual examination or by tactile examination using a mirror and sickle-type dental explorer (#23) and scored as follows: 0, absent or no calculus present; 1, mild or supragingival calculus covering not more than one-third of the exposed tooth surface; 2, moderate or supragingival calculus covering more than one third but not more than two-thirds of the tooth surface or the presence of individual flecks of subgingival calculus around cervical portion of the tooth or both; 3, severe or supragingival calculus covering more than two-thirds of the exposed tooth surface or a continuous heavy band of subgingival calculus around cervical portion of the tooth or both.[7] To calculate gingival index (GI), soft tissues surrounding each tooth were divided into four gingival scoring units: mesial-facial papilla, distal-facial papilla, facial margin and entire lingual gingival margin.
A blunt instrument, such as a periodontal probe, was used to assess the bleeding potential of the tissues around Ramjford teeth and each of the four gingival units was assessed according to the following criteria: score 0, absence of inflammation, or normal gingiva; score 1, mild inflammation; slight change in color, slight edema, no bleeding on probing; score 2, moderate inflammation; moderate glazing, redness, edema and hypertrophy, bleeding on probing; score 3, severe inflammation; marked redness and hypertrophy, ulceration and tendency to spontaneous bleeding.[8] The GI score for the area was obtained by totaling the scores around each tooth and dividing by the number of teeth examined. If the scores around each tooth are totaled and divided by four, the GI score for the tooth is obtained. Totaling of all the scores per tooth and dividing by the number of teeth examined provides the GI score per person. The GI may be used to evaluate a segment of the mouth or a group of teeth in the same way. Probing Pocket Depth (PPD) is the distance to which an ad-hoc instrument (UNC 15 probe) penetrates into the pocket. Calibrated UNC 15 probe was inserted parallel to the long axis of the tooth to measure the distance from the gingival margin to base of sulcus or pocket to the nearest millimeter, at four sites of a tooth, viz. mesio-buccal, buccal, disto-bucal, and mid-lingual, around all teeth. Deepest pocket in millimeter was considered amongst all PPD measurements. GR was scored as “present” if gingival margin was located apical to cemento-enamel junction (CEJ) at the buccal aspect of all the teeth. Clinical Attachment Loss (CAL) was determined by calculating the distance from a fixed reference point, CEJ, to the base of pocket or sulcus. Mobility was measured by holding the tooth firmly between the handles of two metallic instruments and effort was made to move it in all directions. All teeth were scored using the following criteria:[9] no mobility (score 0), slight mobility to touch (score 1), mobility of 1–2 mm (score 2) and obvious looseness with mobility >2 mm (score 3). Furcation involvement was detected using Naber's probe and scored according to criteria modified from Loeche et al.[9] as follows: no furcation involvement (score 0), slight indentation (score 1), pronounced indentation (score 2), through-and-through penetration but filled with soft tissue and might not be visible (score 3), through-and through-penetration and furcation was clinically visible (score 4).
Methodology
After taking informed consent of all the participants, they were asked to fill the questionnaire. Based on the voluntary reports of the smokeless tobacco users, participants were classified as: nonusers, who had never used smokeless tobacco or had used smokeless tobacco in the past but never more frequently than once a month; former users, who had used smokeless tobacco more than once a month in the past but had not used smokeless tobacco (ST) within the previous month; and current users, who had used smokeless tobacco more frequently than once a month and who had used smokeless tobacco within the previous month.[10] However, some of the respondents using certain brands of tooth pastes/powder (Gul, Lal Dant Manjan) did not consider it to be a tobacco-based product. Such participants were also considered as smokeless tobacco users (involuntary users). The amount of smokeless tobacco used was based on the number of packs or pieces. Because many participants were using more than one type of smokeless tobacco, the duration and quantity were calculated individually, as well as in combination in cases of combined users. After completing the questionnaire, all the participants underwent clinical examination for the above-mentioned parameters.
Statistical analysis
This was done by using Statistical Package for Social Sciences version 15. The following tests were used for the study: Percentages, proportions, mean and standard deviation, and Chi-square test (to determine the presence of association between the risk factor and the outcome). Odd's ratio (OR)/cross-product ratio (to deduce the strength of association between the risk factor and outcome) at 95% confidence interval was calculated as well. Student's “t” test was used to test the significance of two means, and the level of significance “P” at different confidence levels was interpreted as follows: P>0.05 not significant, P<0.05 significant, P<0.01 highly significant, and P<0.001 very highly significant.
RESULTS
Maximum incidence of smokeless tobacco consumption was observed in the age group 21–30 years (39.4%), whereas minimum consumption was observed in the age group 10–20 years (7.5%). The peak smokeless tobacco consumption was observed between the ages 21 and 40 years. Recording of oral hygiene measures included in this study showed majority of subjects (n=1961) used tooth brushing as the oral hygiene measure, while some used datoon (n=30; 1.5%) for cleaning their teeth and others used their finger (n=54; 2.6%) with or without tooth powder.
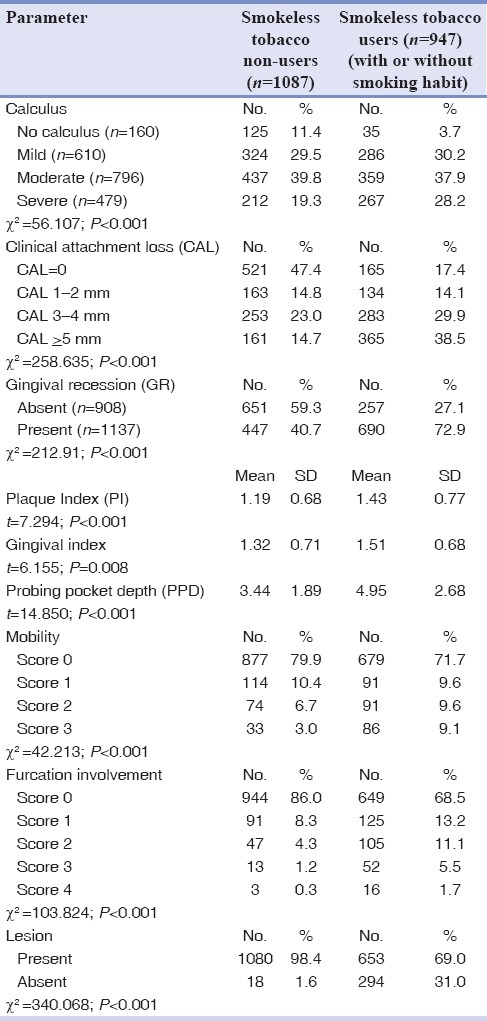
More than half (52.3%) of the subjects were users of any form of tobacco (smoke form, smokeless form). There were 290 (21.5%) subjects who had both smoke and smokeless forms of tobacco habits. A total of 122 (6.0%) subjects had the habit of smoking only, while 657 (32.1%) subjects had the habit of using smokeless form only. Among the different types of smokeless tobacco used, Gutkha was the most common (n=508; 24.8%). There were 15/94 (15.96%) Gul users who were using it involuntarily, whereas amongst Lal Dant Manjan users, the proportion of involuntary users was 65/172 (37.79%). Both the incidence as well as severity of calculus was significantly higher amongst smokeless tobacco users as compared to non-users (P<0.001) [Table 2]. Similarly, CAL, GR, mobility, furcation and lesions were significantly higher amongst smokeless tobacco users as compared to those not consuming smokeless tobacco (P ≤ 0.001). The mean values for PI, GI and PPD (in mm) showed a statistically significant difference between users and non-smokeless tobacco users (P<0.001). The incidence and severity of calculus, CAL, GR, mobility, furcation and lesions were found to be significantly higher amongst subjects with longer duration (>5 years) of use as compared to those with shorter duration of use (P<0.001). Similar trends were obtained for PI, GI and PPD too.
Table 2.
Association of smokeless tobacco with different periodontal health indicators in comparison to non-smokeless tobacco users
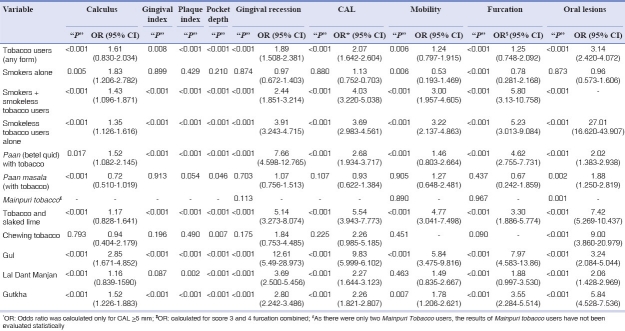
The OR for severe form of calculus was maximum for Gul (OR=2.85), whereas for Paan masala (with tobacco), the same was observed to be minimum (OR=0.72). Among the different habits, the mean GI for users was observed to be significantly higher as compared to that for non-users except for smokers alone (P=0.899), Paan masala (with tobacco) (P=0.913), chewing tobacco (P=0.196) and Lal Dant Manjan (P=0.087) users, though among these too, Lal Dant Manjan had higher mean GI as compared to that in non-users. Among the different habits, the mean PI for tobacco users was observed to be significantly higher as compared to that for non-users except for smokers alone (P=0.429), Paan masala users (with tobacco) (P=0.054) and chewing tobacco users (P=0.490). For each of these categories, the mean plaque indices of users were lower as compared to others. Among the different types of habits, the mean pocket depth was observed to be significantly higher amongst users as compared to others, except for smokers alone (P=0.210) where no significant difference between two users and others could be seen though the mean value of users was higher as compared to that of non-users. Although overall, a majority of subjects (55.6%) had GR, however, among different types of tobacco habits, the proportion of subjects showing GR was significantly higher as compared to others, except for smokers alone, Paan masala, Mainpuri tobacco and chewing tobacco users, where the difference between those having GR and those not having GR was not significantly different from that of non-users (P>0.05). The proportion of moderate to severe forms of CAL was observed to be significantly higher amongst users as compared to non-users. However, this difference was not significant statistically for smokers alone, Paan masala users and those using chewing tobacco. The incidence and severity of mobility was seen to be varying in different tobacco habits, showing a higher incidence and severity as compared to non-users for almost all categories of tobacco use, except Paan masala, Mainpuri tobacco, chewing tobacco and Lal Dant Manjan users, where though the incidence was higher as compared to that of overall subjects, the difference was not significant statistically as compared to non-users (P>0.05). Amongst smokers alone, though the incidence was higher as compared to others, the severity was significantly lower as compared to others (P=0.006). The OR for severity was above unity (>1) for all the habits except for smokers alone where the OR was 0.53. Maximum odds were observed for Gul (OR=5.84). Both the incidence and severity of furcation were observed to be significantly higher amongst smokeless tobacco users as compared to non-users except for Paan masala and Mainpuri tobacco users. Apart from smokers alone, for all the tobacco habits, the incidence of lesions was significantly higher as compared to non-users. Smoking along with tobacco had the maximum hazard for development of lesions. It was observed that smokeless tobacco keratosis alone or in combination was the most common lesion, followed by oral sub-mucous fibrosis. The locational use of some of the smokeless tobacco habits was specified by the respondents. Maximum locational use was specified for the use of tobacco and slaked lime (68.2%), whereas no specific location was specified for Mainpuri tobacco and Lal Dant Manjan. For Paan with tobacco, buccal sides were the most commonly specified locations, and for tobacco with slaked lime, anterior side was the most commonly cited site. For chewing tobacco, Gutkha and Gul too, buccal side was the most common site involved. The site of lesion matched with the location of use in more than half (56.62%) of the cases with lesions. In 154 (43.38%) subjects, such matching could not be done [Table 3].
Table 3.
Association of various types of smokeless tobacco with different parameters
DISCUSSION
The rationale of this cross-sectional survey was to examine the effect of commonly used different types of smokeless tobacco in India on periodontal health of smokeless tobacco users as compared with the non-tobacco users and to investigate the relationship between the type of smokeless tobacco and the severity of periodontal destruction in a Lucknow-based population where the practice using of smokeless tobacco is fast growing.
The range of age group in the present study represents the effects of smokeless tobacco use on periodontium among the children, adolescents, adults and elderly, as it has been seen that the use of any kind of tobacco started as early as 10 years of age. According to Kumar et al.,[4] majority of smokeless tobacco users (60%) started consuming tobacco before 21 years of age and about 22% started before the age of 15 years. Peak incidence of smokeless tobacco consumption was observed in the age group between 21 and 30 years (39.4%) in this study. Increasing demand and usage amongst young adults and in older women living in rural southern areas in United States have been reported by many. Although the cause related to the increased prevalence of smokeless users is not a part of the present study, stressors like poor family relation and low school satisfaction,[10] poor grades in school and peer group pressure amongst the adolescents and young adults have been reported by many earlier studies.[11]
Among the smokeless tobacco users, males (85.3%) have been found to be associated with the habit of smokeless tobacco 5.8 times more in comparison to the total number of female (14.7%) smokeless tobacco users. Similar observations were made by Bala et al.[12] who observed the use of Paan masala to be around four times higher in males as compared to females, whereas the consumption of tobacco was also observed to be more than twice amongst males as compared to females. In a study on tobacco use in rural area of Bihar, India, by Sinha et al.,[13] tobacco use was found to be 78% in men and 52% among women. The gender wise differences in tobacco use are dependent on the regional or local issues. In the present study, higher prevalence of use of tobacco amongst males has been attributed to the fact that the concentration of economic power is in the hands of males and is also due to their proneness to stress situations and the assumption that tobacco use helps them to carry out their occupational tasks with more concentration. Based on this hypothesis, Chu et al.[14] evaluated the periodontal health status of male smokeless tobacco users from a rural population. During the survey, participants were found to use more than one type of smokeless tobacco. Hence, the effect is evaluated in unison and combination of various smokeless tobaccos is also compared with only smokeless tobacco users.
Although Indian legislation prohibits the use of tobacco as an ingredient in dental care products, however, various tobacco products are used as dentifrices in different parts of India and such products are available in the form of powder or paste, which are applied most commonly with the index finger to teeth and gums.[15] Sinha et al.[15] reported that 6–68% students are currently using tobacco-containing oral care product. Hence, many of the participants were unaware of the habitual use of smokeless tobacco. Such individuals, either using “Lal Dant Manjan” (n=65) or “Gul Manjan” (n=15), which have been reported to contain 9.3–248 mg of tobacco per gram of the tooth powder, are included under involuntary smokeless tobacco users. So, the total number of any form of tobacco users includes both voluntary and involuntary users (n=1069) and represents 52.3% of the total participants. Amongst them, 32.1% have the habit of using smokeless tobacco alone, followed by 21.5% subjects having both smokeless and smoke habits, whereas the frequency of “alone smokers” is 6% of the total participants. Also, in contrast to Sinha et al.'s report[13] and other reported data, in this study, we could not find any participant using “tobacco gargles” as the form of smokeless tobacco users.
Ten percent of the total participants are the “former smokeless tobacco users in the present study, but in contrast to the “replacement users” reported by Bergstrom et al.,[16] the present study does not reveal any such case. However, involuntary users (who do not consider themselves as tobacco users) represent 6.4% of the total population.
Among the different types of smokeless tobacco, Gutkha was the most commonly used smokeless tobacco form, followed by Lal Dant Manjan, Paan, Khaini, Paan masala, Gul, chewing tobacco and Mainpuri tobacco. Single users and multiple users have also been evaluated in the study and results show that among different types of smokeless tobacco forms, Gutkha in combination [single (Gutkha with one type), double (Gutkha with two different types), and triple (Gutkha with three different types)] was the most commonly used smokeless tobacco form. However, most of the studies published except the one by Sood[5] are concentrated around snuff-users. These include the studies of Geer and Poulson,[17] Offenbacher and Weathers,[18] Hart et al.,[19] Johnson and Slach,[20] and Rolandson et al.[21] This is in contrast to the present study, where we did not find any snuff-user in the local population. Also, to make the calculations simple and more meaningful, amongst all the smokeless tobacco combinations, prominent component users were grouped as Paan (betel quid) group; Paan masala; Mainpuri group; tobacco with slaked lime; chewing tobacco; Gul group, Lal Dant Manjan, and Gutkha group, and association with the various periodontal health indicators were calculated. The difference in different forms of smokeless tobacco can be attributed to the difference in time, availability and changing preferences of the individuals.
Results of PI, CI, and GI in our study indicated that despite the daily oral cavity cleaning habits, either by tooth brushing, datoon, and finger, the smokeless tobacco users had poorer oral hygiene, followed by alone smokeless users, smokers alone and non-tobacco users. Amongst the smokeless tobacco users, Gul users revealed the highest percentage of severe form of calculus, followed by Khaini (tobacco and slaked lime), Lal Dant Manjan, Paan (betel quid), Gutka, chewing tobacco, and Paan masala users. Only two Mainpuri users were found, and both smokeless tobacco users presented severe form of calculus and revealed no significant association with calculus severity.
Greater gingival inflammation was seen in smokeless tobacco users and alone smokeless tobacco users than non-tobacco users. These results are in contrast to report of Robertson et al.,[22] but similar to that of Chu et al.[14] A site-specific study by Poore et al.[23] revealed significantly higher gingival inflammation at smokeless tobacco placement sites as compared to non-users. The mechanism of action, as explained by Mavropoulos et al.,[24] was neurogenic inflammation induced by activation of sensory nerves and the subsequent release of vasodilatory peptides from their peripheral endings, known as “axon reflex”. Bleeding on probing has been shown to be an important risk predictor for increased attachment loss, if present at regular intervals,[25] or its absence is a good indicator of periodontal disease stability.[26] Similar to the report by Chu et al.,[14] in the present study population was also measured the effect of time duration in years of smokeless tobacco use. Dose–response relationship seems to exist between smokeless tobacco use and severity of injury to the periodontium, as was shown by Hirsch et al.[27] and Grady et al.[28] Results of the present study also show statistically significant higher incidence and severity of calculus score, CAL, GR, mobility, furcation and oral lesions as well as mean PI score, GI and PPD score amongst longer duration (>5 years) users as compared to shorter duration (1–5 years and ≤1 year) users.
Average PPD was more in smokeless tobacco users, followed by alone smokeless tobacco users, smokers alone and non-tobacco users, and this decreasing trend was statically significant (P<0.001). Incidence of GR was also found to be the highest amongst smokeless tobacco users, followed by alone smokeless users, smokers alone and non-tobacco users. Although no exact association and correlation is a part of the study, combined effect of horizontal tooth brushing habit and effect of smokeless tobacco alone or in combination with smoking might be responsible for greater periodontal destruction in smokeless tobacco users as discussed by Robertson et al.[29] Amongst the smokeless tobacco users, highest proportion of GR was observed with Gul (93.6%) users, followed by Paan (betel quid) chewers, Khaini, Lal Dant Manjan, Ghutkha, Paan masala users, but in contrast no GR was seen in Mainpuri users.
Attachment loss is an important component of the periodontal disease measure that defines past history of the disease and is especially pertinent in the assessment of current exposure to tobacco. Present study revealed CAL of more than 5 mm in majority of smokeless tobacco users, followed by alone smokeless tobacco users, smokers alone and non-tobacco users. Similar trends were also seen amongst the mobility (score 3), furcation involvement (score 3), and presence of soft tissue lesion in the oral cavity, but furcation involvement of score 4 represented equal distribution amongst only smokeless tobacco users and smokers alone and was the highest in smokeless tobacco users. Chemical injury to thin areas of gingiva, chronically exposed to the smokeless tobacco, in addition to smokeless tobacco induced epithelial proliferation that bridges the narrow lamina propria of sites with an alveolar dehiscence might have resulted in loss of periodontal tissue.[29]
Amongst various smokeless tobacco users, Gul users, Khaini users, Lal Dant Manjan, Gutkha and Paan users present higher mean GI, higher mean PI and higher mean PPD as compared to non-Gul users, non-Khaini users, non-Lal Dant Manjan users, non-Gutkha users and non-Paan users, respectively. Although the individuals having the habit of chewing tobacco have higher mean GI score and higher mean PPD as compared to non-users, they have lower mean PI score as compared to non-users. Also, in contrast, Paan masala users revealed mean GI score almost equal to non-users, lower mean PI score but higher mean PPD as compared to non-Paan masala users.
In contrast to Paan masala group, where majority of the respective participants revealed attachment loss of 3–4 mm, amongst Khaini users (tobacco and slaked lime), Gul users, Paan (betel quid) users, and Gutkha users, majority of the respective participants revealed CAL of more than 5 mm (severe attachment loss), followed by 3–4, 1–2 mm and no CAL. Amongst chewing tobacco users and Lal Dant Manjan users, majority of the respective participants revealed CAL of more than 5 mm, followed by attachment loss of 3–4 mm, no attachment loss, and 1–2 mm attachment loss. Proportion of moderate to severe form of attachment loss was observed to be significantly higher amongst most of smokeless tobacco users except Paan masala and chewing tobacco groups.
Also, amongst the entire smokeless tobacco users group, no mobility was seen in majority of the respective participants and was followed by score 1, score 2 and score 3 in Paan (betel quid) and Paan masala groups. Higher incidence and severity of mobility (score 3) was seen in almost all the categories except Paan masala, Mainpuri tobacco chewers, Lal Dant Manjan group and Gutkha group as compared to non-users. Although the incidence was higher amongst these groups, the difference was not statistically significant as compared to non-users. Amongst the entire smokeless tobacco users group, no furcation involvement was shown by majority of the users, but, the incidence and severity were seen to be significantly higher amongst smokeless tobacco users than non-users.
It has also been found in this study that no lesion was observed amongst the non-tobacco users; however, majority of total smokeless tobacco users, followed by alone smokeless tobacco users and smokers alone, revealed some tobacco-related lesion, and amongst them smokeless tobacco keratosis represented the highest frequency of 6.2% of the total population, followed by oral submucous fibrosis and leukoplakia like lesion (2.5%). Thus, an inference can be drawn from the present study that the oral lesions presented are associated with some kind of tobacco users. Geer and Poulson,[17] Robertson et al.[22] and Poulson et al.[30] suggested that white oral keratotic lesions are observed in 50–60% of smokeless tobacco users, and revealed that such lesions are commonly found in areas of mouth where the smokeless tobacco is placed. Amongst the smokeless tobacco users, highest proportion of oral lesions was observed amongst chewing tobacco group, followed by Khaini, Ghutkha, Gul, Lal Dant Manjan, Paan masala users. Both Mainpuri users revealed oral lesions; however, no specific location was observed in contrast to Khaini group (tobacco and slaked lime) where majority revealed anterior vestibule as the specified location for placement. Buccal side as the specific location for the placement of the smokeless tobacco was seen amongst majority of tobacco chewers, followed by Gutkha users, Paan masala users and Paan (betel quid) with tobacco users. Ahmad et al.[31] showed that Gutkha was the most commonly used in most of oral submucous fibrosis cases and also established an association between the lesion side and the site of placement.
Present study is in confirmation with the already published data revealing the effect of snuff (smokeless tobacco) in European and American populations, that smokeless tobacco, used by the local population of Lucknow in various forms, is injurious to periodontal health. Most of the studies so far have been carried out in the later part of the 20th century, whereas Gutkha as a popular product has assumed significance in the late 1990s and later. The convenience of handling and consumption of Gutkha too makes it a popular choice. Apart from that, Paan Quid with tobacco is a popular traditional practice in Lucknow. Paan eating was taken to its zenith of cultural refinement in the pre-partition era in North India, mainly Lucknow, where Paan eating became an elaborate cultural custom and was seen as a ritual of utmost sophistication.[32]
Thus, periodontal health of the general population in the region of Lucknow required immediate attention as majority of subjects irrespective of their habit status had the onset of CAL and GR, more so amongst the users of non-smoking form of tobacco. The impact of smokeless form of tobacco use was significantly higher on all the periodontal health indicators, viz. calculus, CAL, GR, mobility, furcation, lesion, PI, GI and PPD. Both duration and frequency of smokeless tobacco use significantly affected the periodontal health. Among the different forms of smokeless tobacco use, Gul was found to be having maximum risk of affecting periodontal health as compared to other forms of smokeless tobacco use, but it would be pertinent to mention that majority of Gul users were consuming some other form of smokeless tobacco too. Also, use of Paan masala (with tobacco) had minimum effect on periodontal health as compared to other smokeless tobacco forms, but great majority (82.2%) of Paan masala (with tobacco) users had no other form of smokeless tobacco consumption. As compared to smoke form, the smokeless tobacco form had a greater adverse effect on periodontal health.
The results of present study can act as a motivation to the users of tobacco to quit the habit of taking smokeless tobacco as well as various health agencies can be suggested to control the use of different forms of smokeless tobacco, especially Gul, Khaini (tobacco and slaked lime) Lal Dant Manjan, Paan (betel quid), and Gutkha.
CONCLUSION
Within the limitations of the present study, the following findings were made during its course. More than half (52.3%) of the total participants were having some kind of tobacco habit, and 32.1% subjects had the habit of using smokeless tobacco alone, followed by 21.5% subjects who used both smoke and smokeless tobacco, whereas 6% subjects had the habit of smoking alone. Incidence and severity of calculus, CAL, GR, mobility, furcation and lesions as well as mean PI, GI and PPD were significantly higher statistically amongst longer duration (>5 years) smokeless tobacco users as compared to non-tobacco users. It was also found in the study that no lesion was observed amongst the non-tobacco users; however, 37.5% of smokeless tobacco users, 25.4% users of smokeless tobacco alone and 14.8% of smokers alone revealed some tobacco-related lesion, and amongst them, smokeless tobacco keratosis represented the highest frequency of 6.2% of the total population. Amongst the smokeless tobacco users, highest proportion of oral lesions was observed amongst chewing tobacco group (60.9%), followed by Khaini (51.0%), Gutkha (35.4%), Gul (35.1%), Lal Dant Manjan (25.6%) and Paan masala (24.3%).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Dobe M, Sinha DN, Rahman K. Smokeless Tobacco Use and Its Implications in WHO South East Asia Region. Indian J Public Health. 2006;50:70–5. [PubMed] [Google Scholar]
- 2.Montén U, Wennström JL, Ramberg P. Periodontal conditions in male adolescents using smokeless tobacco (moist snuff) J Clin Periodontol. 2006;33:863–8. doi: 10.1111/j.1600-051X.2006.01005.x. [DOI] [PubMed] [Google Scholar]
- 3.Frithiof L, Anneroth G, Lasson U, Sederholm C. The snuff- induced lesion. A clinical and morphologic study of a Swedish material. Acta Odontol Scand. 1983;41:53–64. doi: 10.3109/00016358309162303. [DOI] [PubMed] [Google Scholar]
- 4.Kumar S, Prabu D, Kulkarni S, Dagli RJ. Tobacco as risk factor for periodontal disease in green marble mine laborers of Rajasthan, India. Brazilian J Oral Sci. 2008;7:1641–7. [Google Scholar]
- 5.Sood M. A study of epidemiological factors influencing periodontal diseases in selected areas of district Ludhiana, Punjab. Indian J Community Med. 2005;30:2. [Google Scholar]
- 6.Silness P, Loe H. Periodontal disease in pregnancy. Acta Odontol Scand. 1964;22:121. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 7.Greene JC, Vermillion JR. The Simplified Oral Hygiene Index. J Am Dent Assoc. 1964;68:7. doi: 10.14219/jada.archive.1964.0034. [DOI] [PubMed] [Google Scholar]
- 8.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence And Severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 9.Loesche WJ, Giordano JR, Soehren S, Kaciroti N. The non surgical treatment of patients with periodontal diease: results after five years. J Am Dent Assoc. 2002;133:311–20. doi: 10.14219/jada.archive.2002.0170. [DOI] [PubMed] [Google Scholar]
- 10.Stevens MM, Freeman DH, Jr, Mott LA, Youells FE, Linsey SC. Smokeless tobacco use among children the New Hampshire study. Am J Prev Med. 1993;9:160–7. [PubMed] [Google Scholar]
- 11.Mukherjee K, Hadaye RS. Gutkha consumption and its determinants among secondary school male students. Indian J Community Med. 2006;31:177. [Google Scholar]
- 12.Bala DV, Bodhiwala IN, Patel DD, Shah PM. Epidemiological Determinants of Tobacco Use In Gujarat State, India. [Last accessed on 2011, Jan 01];Indian J Comm Med. 2006 31 Available from: http://www.indmedica.com/journals.php?journalid=7andissueid=79andarticleid=1055andaction=article . [Google Scholar]
- 13.Sinha DN, Gupta PC, Pednekar MS. Tobacco use in a rural area of Bihar, India. Indian J Community Med. 2003;27:167–70. [Google Scholar]
- 14.Chu YH, Tatakis DN, Wee AG. Smokeless tobacco and periodontal healthy in a rural male population. J Periodontol. 2010;81:848–54. doi: 10.1902/jop.2010.090310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sinha DN, Gupta PC, Pednekar MS. Use of tobacco products as dentifrice among adolescents in India. Questionnaire study. BMJ. 2004;328:323–4. doi: 10.1136/bmj.328.7435.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bergstrom J, Keilani H, Lundholm C, Radestad U. Smokeless tobacco (Snuff) use and periodontal bone loss. J Clin Periodontol. 2006;33:549–54. doi: 10.1111/j.1600-051X.2006.00945.x. [DOI] [PubMed] [Google Scholar]
- 17.Greer RO, Jr, Poulson TC. Oral tissue alterations associated with the use of smokeless tobacco by teen-agers. Part I. Clinical findings. Oral Surg Oral Med Oral Pathol. 1983;56:275–84. doi: 10.1016/0030-4220(83)90009-9. [DOI] [PubMed] [Google Scholar]
- 18.Offenbacher S, Weathers DR. Effects of smokeless tobacco on periodontal, mucosal and caries status of adolescent males. J Oral Pathol Med. 1985;14:169–81. doi: 10.1111/j.1600-0714.1985.tb00480.x. [DOI] [PubMed] [Google Scholar]
- 19.Hart GT, Brown DM, Mincer H. Tobacco use and dental disease. J Tenn Dent Assoc. 1995;75:25–7. [PubMed] [Google Scholar]
- 20.Johnson GK, Slach NA. Impact of tobacco use on periodontal health. J Dent Edu. 2001;65:313–21. [PubMed] [Google Scholar]
- 21.Rolandsson M, Hellqvist L, Lindqvist L, Hugoson A. Effects of snuff on the oral health status of adolescent males: a comparative study. Oral Health Prev Dent. 2005;3:77–85. [PubMed] [Google Scholar]
- 22.Robertson PB, Walsh MM, Greene JC. Oral effects of smokeless tobacco use by professional baseball players. Adv Dent Res. 1997;11:307–12. doi: 10.1177/08959374970110030101. [DOI] [PubMed] [Google Scholar]
- 23.Poore TK, Johnson GK, Reinhardt RA, Organ CC. The effects of smokeless tobacco on clinical parameters of inflammation and gingival crevicular fluid prostaglandin E2, Interleukin-1a, and Interleukin- 1b. J Periodontol. 1995;66:177–83. doi: 10.1902/jop.1995.66.3.177. [DOI] [PubMed] [Google Scholar]
- 24.Mavropoulos A, Aars H, Brodin P. The acute effects of smokeless tobacco (snuff) on gingival blood flow in man. J Periodont Res. 2001;36:221–6. doi: 10.1034/j.1600-0765.2001.036004221.x. [DOI] [PubMed] [Google Scholar]
- 25.Lang NP, Joss A, Orsanic T, Gusberti FA, Siegrist BE. Bleeding on probing. A predictor for the progression of periodontal disease? J Clin Periodontol. 1986;13:590–6. doi: 10.1111/j.1600-051x.1986.tb00852.x. [DOI] [PubMed] [Google Scholar]
- 26.Tu YK, Gilthorpe MS, Griffiths GS, Maddick IH, Eaton KA, Johnson NW. The application of multilevel modeling in the analysis of longitudinal periodontal data – Part I: Absolute levels of disease. J Periodontol. 2004;75:127–36. doi: 10.1902/jop.2004.75.1.127. [DOI] [PubMed] [Google Scholar]
- 27.Hirsch JM, Heyden G, Thilander H. A clinical, histomorphological and histochemical study on snuff-induced lesions. J Oral Pathology. 1982;11:387–98. doi: 10.1111/j.1600-0714.1982.tb00180.x. [DOI] [PubMed] [Google Scholar]
- 28.Grady D, Greene J, Daniels JE, Ernster VL, Robertson PB, Hauck W, et al. Oral mucosal lesions found in smokeless tobacco users. J Am Dent Assoc. 1990;121:117–23. doi: 10.14219/jada.archive.1990.0139. [DOI] [PubMed] [Google Scholar]
- 29.Robertson PB, Walsh M, Greene J, Ernster V, Grady D, Hauck W. Periodontal Effects Associated With the Use of Smokeless Tobacco. J Periodontol. 1990;61:438–43. doi: 10.1902/jop.1990.61.7.438. [DOI] [PubMed] [Google Scholar]
- 30.Poulson TC, Lindenmuth JE, Greer RO., Jr A comparison of smokeless tobacco in rural and urban teenagers. CA Cancer J Clin. 1984;34:248–61. doi: 10.3322/canjclin.34.5.248. [DOI] [PubMed] [Google Scholar]
- 31.Ahmad MA, Ali SA, Ali AS, Chaubey KK. Epidemiological and etiological study of oral submucous fibrosis among gutkha chewers of Patna, Bihar. J Indian Soc Pedod Prev Dent. 2006;24:84–9. doi: 10.4103/0970-4388.26022. [DOI] [PubMed] [Google Scholar]
- 32.Sharar AH. Preparing and serving betel leaf. Lucknow Omnibus: Oxford University Publications; 2001. Betel leaf, apturtemances and tobacco; pp. 219–23. [Google Scholar]