Summary
This article provides a critical discussion of recent work on local government health care and health services in interwar England. A literature review examines case study approaches and comparative quantitative surveys, highlighting conventional and revisionist interpretations. Noting the differing selection criteria evident in some works, it argues that studies based upon a limited number of personal health services provide an insufficient basis for assessing local health activity and policy. There follows a regional study demonstrating various discrepancies between health financing data in local sources and those in nationally collated returns. These in turn give rise to various problems of assessment and interpretation in works relying on the latter, particularly with respect to services for schoolchildren and long-stay patients. The case study points to the importance of integrating poor law medical services in evaluations, and of learning more about the role of government subsidy in supporting expanding services.
Keywords: localgovernment, personalhealthservices, municipal, finance, decentralization, publicassistance
Interwar England as a Historical Example of Health Service Decentralization
The question of whether local autonomy or central control is preferable in health service organization has risen up the policy agenda in recent years.1 In low-income countries decentralization has been recommended by the World Bank as essential to sustainable health sector reform, with its potential to lessen bureaucracy, quicken decision making, engage local populations, and respond to demand.2 Yet recent case studies suggest weaknesses, such as insufficient local capacity, inequitable provision, and fragmentation.3 Localism is reviving in high-income nations too, whether to make services more patient responsive or to reinstate the "healthy city" as the site of preventive strategies.4 Again though, the evidence in favor of abandoning hierarchical structures is uncertain: equity and efficiency are not always enhanced, and lack of integration can militate against effective management.5
England's health services in the first half of the twentieth century offer a rich historical example of decentralization.6 Here local government had accumulated multiple health powers, ranging from provision of sanitary infrastructure to hospitals and clinics, financed both by local taxation (the "rates") and by state subsidy.7 This arrangement resulted from the independent emergence of local and national governing bodies in the distant past, and the subsequent delegation of powers and duties to localities, whose boundaries and functions were now determined by the center.8 The state's rationale for this was that welfare services needed to be shaped according to particular local factors, and that democratic accountability was best secured at this level.9 Indeed, when policy discussions began in the 1940s about establishing a comprehensive and universal health service, it was widely expected that this would be through local government structures.10 However, the National Health Service (NHS) Act of 1946 created instead a centralized, hierarchical administration in which local authorities surrendered all but residual public health functions to new regional bodies. The architect of the NHS, Labour politician Aneurin Bevan, argued that this was because they lacked financial and managerial capacity and had a track record of inequitable provision.11 To some contemporaries, however, this was the unwarranted abandonment of a cherished goal that instilled a democratic deficit in the NHS.12 Both they and subsequent historians suggested instead that Bevan's motive was political compromise with the doctors' trade association, which rejected a local government-led NHS.13 Thus the record of decentralized health provision in England during its interwar "zenith" remains contentious, and indeed has been subject to revisionist interpretation in recent years.
The purpose of the present article is not to develop a fresh evaluation but rather to address conceptual and methodological questions that are central to such appraisals. Early histories generally endorsed Bevan's criticisms, depicting local authority provision as inadequate and geographically patchy. However, recent studies have begun to redress this view by showing the achievements of progressive authorities and exploring subjects such as local choice, public hospital development, and relations between the locality and the center.14 Analysis of municipal health expenditure as recorded in official publications has been a central aspect of such work, both as a proxy for quality and effort in service delivery and as an indicator of local discretion in health policy.15 It is the challenge of using such data, and the robustness of the conclusions that may be drawn from it, that is the main focus here.
The analysis begins with a brief survey of the historiography and of the conceptual difficulties that underlie terms such as municipal medicine. The central sections present results of a regional study of local government health services in the southwest of England; this breaks new ground in revealing patterns of financing obscured in the national sources used hitherto. There then follows a discussion of the methodological problems that are exposed by this approach, and of some new questions it raises.
Local Government Health Services in England: The Literature
The chronology of the gradual accretion of local government health activities is well known. The largest units, the counties, had provided mental asylums since 1808, while the separate poor law administration operated medical facilities for "paupers" and shared in mental health provision.16 Over the course of the nineteenth century the major towns and smaller authorities gained responsibilities for preventive environmental services and isolation hospitals, with locally appointed medical officers of health (MOsH) overseeing them.17 By 1900 there were two main tiers: the counties, created in 1888, with the largest cities, the "county boroughs," distinct from the "administrative counties"; and the smaller urban and rural district councils, created piecemeal between 1872 and 1894. Legislation thenceforth conferred further health powers and duties, the full range falling only on the county boroughs. These included a school medical service (SMS) to provide inspection and treatment (1907, 1918); maternity and child welfare (MCW) facilities such as clinics, midwifery, and subsidized milk (1914, 1918); tuberculosis (TB) dispensaries and sanatoria (1912, 1921); venereal disease (VD) clinics (1912, 1916); institutional treatment for "mental deficiency" (1913, 1927); and housing improvement, through slum clearance and building subsidies (1919, 1923, 1924, 1930, 1935).18 The Local Government Act of 1929 terminated the poor law's separate administration, and handed responsibility for the now renamed "public assistance" to local authorities. Some then "appropriated" ex-poor law facilities to their health committees, for example developing infirmaries and workhouses into hospitals.19
Early historians of the NHS highlighted the same shortcomings of interwar local government health services asserted by Bevan. Lindsay and Eckstein stressed the "inequalities in service," as well as complexity, irrational distribution, and lack of sectoral integration.20 Pater emphasized low quality, poor coordination, and animosity between municipal and voluntary sectors (the latter was responsible for much acute hospital provision).21 Abel-Smith documented failings in joint working with the voluntary hospitals and the slow progress of appropriation from the poor law.22 These works set the tone for later readings. Webster's official history of the NHS acknowledged the achievement of progressive authorities but again observed geographical variability, inadequacy of resources, and muddled divisions of responsibility.23 Harris noted the "handicap of locality" in the SMS, particularly in areas of high unemployment, and also local disparities in slum clearance and new house building.24 Lewis and Webster claimed that the plethora of new duties had overstretched the MOsH, leading to neglect of public health's traditional "watchdog" and preventive functions.25 Dupree argued that centrism and regionalism were legitimate responses to the localism and particularism, that impeded service rationalization, emphasizing that variations in provision "mattered in terms of life and death."26
Recent years have seen some revision, concentrating on the achievement rather than limitations. Sheard and others showed how early growth of municipal hospital provision outside the Poor Law helped ease demand before the watershed of 1929.27 Powell argued that by the late 1930s the expansion of municipal general hospital provision had eroded geographical disparities created by voluntary institutions.28 He found growth to have been dynamic and the rate of appropriation impressive, given physical and resource constraints of the 1930s.29 The case for the "failure" of interwar public health was weakened by studies of the innovative work of urban MOsH, notably Welshman's discussion of Leicester.30 Focus on individual services showed the importance of local initiatives in community mental health care and MCW, and of the SMS in improving child health.31 The extent to which variation may have reflected political preferences rather than economic capacity was suggested by work on services, such as maternal and infant welfare and mental deficiency, and on cities, such as Sheffield and London.32
A central issue in any appraisal is the variations in expenditure between places, the reasons for these, and the extent to which they mattered.33 Though acknowledging some scope for local choice, Preston's analysis for 1911 found that it was the underlying level of taxable wealth which mainly determined urban differences, creating an "endemic structure of inequality."34 Lee noted that within an overall national rise in health care expenditure of 11.4 percent per annum, 1921-37, there was considerable, and largely consistent, "geographical unevenness" between cities, caused both by the taxable resource base and by "political ambition."35 Published local government financial statistics permitted disaggregation of "health" into subcategories and examination of whether policies were responsive to local electorates. Thomson observed higher expenditure on "mental deficiency" (i.e., learning disability) in Conservative authorities, which he attributed partly to eugenicist attitudes, while Powell's regression analysis revealed that Labour Party strength on local councils influenced expenditure levels on TB and MCW.36 Levene, Powell, and Stewart provided the most detailed temporal and spatial analysis of different categories of health expenditure in the county boroughs. This emphasized the overall expansion of the sector, provided rankings of cities and regions according to variations in spending, and highlighted the "investment choices" of local politicians and officials that these represented.37 Spending, they argued, was a reflection of devolved political preferences because it was borne principally by local taxation.38 Indeed, assuming that expenditure was a reasonable proxy for the quality of services, they viewed the upward trend between 1922 and 1936 (particularly for TB care, MCW, and mental deficiency) as indicative of the relative success of the sector. This cast "into sharp relief" the policy shift toward a highly centralized health service in the mid-1940s.39
In such work the point has been well made that individual case studies cannot capture the "great scope and variation" of local government health activity.40 Thus recent scholarship has aimed instead for a comprehensive view of the "urban system," and principally the county boroughs. Justifications range from the central role of cities in the crises of capitalism that welfare legislation ameliorated, to the representativeness of the county boroughs in terms of population health trends.41 More prosaically, because of their broader range of powers there are fuller published data for the county boroughs than for county and district councils. However, if these nationally collated statistics are to provide the desired integrative overview, the question arises of whether they accurately reflect local records of public health and health services.
Conceptualizing Local Government Health Services
As a prelude to analysis, it is important to define the parameters of local government health activity more clearly, because earlier scholars have differed in their selection criteria. Authors of urban or regional case studies have taken a broad view. Welshman, for example, treated "municipal medicine" as incorporating all the services noted above (SMS, TB, MCW, VD, mental health, hospitals) along with some environmental health (slum clearance), while Thompson incorporated air quality, housing, water purity, sewerage, and recreational facilities as aspects of health policy.42 However, scholars adopting the comprehensive quantitative approach have framed the subject more narrowly, concentrating on the "personal health services," a contemporary term that included curative and preventive provision, but neither housing nor environmental health.43 Lee took "municipal medicine" to be "health care" supplied by local authority public health committees: hospitals, sanatoria, dispensaries, MCW, vaccination, and disease prevention.44 This, it should be stressed, does not capture all the personal health services, because the SMS and poor law medicine were funded under the education and poor relief budgets, respectively. Levene, Powell, and Stewart concentrated on the same categories, arguing further that environmental health had "receded in political significance" by the twentieth century.45 Here then it was not the potential effect of decentralized services on population health that mattered, but their perceived importance in debates about health system reform.
Of course, it might be argued that definitional boundaries are inevitably arbitrary, given that determinants of health range from access to medical services to income distribution and employment opportunities.46 In the context of English local government records, however, the selection problem is discrete. It hinges on whether to focus only on the personal health services (and if so, which) or whether to include housing and environmental health. There are three arguments that favor the more inclusive approach.
First, between 1918 and 1939 contemporary MOsH clearly understood their remits to be wide-ranging.47 A content review of their local annual reports demonstrates that their responsibilities fell into three broad areas: (1) the environment, which included sanitation (sewerage, refuse collection, pest control), fresh water supplies, parks, public baths, and toilets; (2) public housing programs, particularly through improvement orders and slum clearance; and (3) personal health services, including isolation hospitals, mental hospitals, some general acute hospitals, TB dispensaries and sanatoria, the SMS (most MOsH doubled as school medical officers), VD clinics, and MCW, such as midwives, clinics, and hospitals. A fourth and subsidiary area was the poor law/public assistance, which provided some domiciliary medical attendance as well as mental health and institutional care. Although after 1929 the public assistance and health committees were distinct, MOsH typically had an advisory role on the former and alluded briefly to the public assistance institutions (PAIs) in reports.
Second, the contextual literature suggests that environmental interventions and housing did matter to the health of local populations. Sanitation may not have been "the most dramatic manifestation" of public health work, but its failure could have serious ramifications, as interwar typhoid outbreaks revealed.48 And while the county boroughs had long completed their major capital works by the 1930s, some rural areas still lacked water mains. Technical handbooks affirmed that sewerage and waste disposal remained "practical public health problems."49 Arguably of more questionable benefit were parks and leisure facilities, although a respectable literature treats these as elements of health-related social capital.50 The impact of housing on physical and mental health is better attested, by both contemporaries and subsequent authors.51 In the interwar period a key rationale of slum clearance was to combat infectious diseases, particularly TB, by tackling domestic sanitation, overcrowding, and damp conditions (albeit that achievement fell short of the need).52 From the midcentury interest began shifting to housing as causal agent in chronic diseases, both somatic and emotional, with the risks to respiratory health from domestic smoke pollution now moving up the policy agenda.53 Viewed from the perspective of population health then, the personal health services were only one component of local action, and there is no a priori reason to suppose they were the most important.54 Various authors note for example the limited effects on outcomes of interwar Britain's "extravagant institutional provision" of TB sanatoria.55
Third, the supposition that only the personal health services were politically significant is not entirely true. Public housing policies may not have been driven solely by health—civic pride, poverty alleviation, and appeasement of social discontent were important too—but they were hardly politically neutral.56 Environment oscillated in political sensitivity through the century, attracting little heated debate in the interwar period but returning to prominence from the 1950s with the controversies surrounding clean air.57 And regardless of their political contentiousness, both areas were prominent aspects of the political economy of local government.
This last point may be illustrated through Figure 1, which shows the composition of health-related activities as measured by spending. It represents only the county boroughs, the local authority units with the full range of health responsibilities. The period is limited to the prewar years in which local expenditure data were recorded, with the statistics for public assistance unavailable before 1930-31, as the earlier poor law data were aggregated only to national and metropolitan levels.58 The health-related public assistance figures here are an approximation, composed of spending on institutional care and mental health; they exclude domiciliary attendance of the sick, which cannot be obtained from the data, and contain an unknown proportion of institutional residents who were neither sick nor infirm; the ambiguities of the health/social care boundary are discussed more fully below.59 SMS expenditure is not shown because it was not disaggregated from the total education budget in national statistics.
Figure 1.
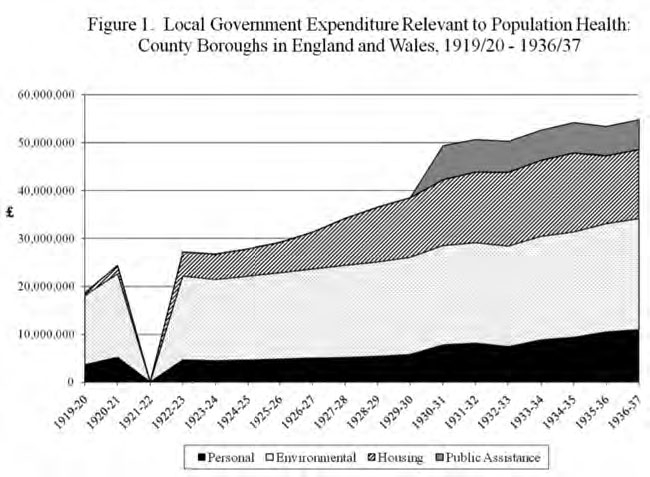
Local Government Expenditure Relevant to Population Health: County Boroughs in England and Wales, 1919/20-1936/37
Environmental health was the largest category of expenditure, partially borne by local taxation and partially by user fees (for waterworks and public baths/toilets). The graph also shows the growth in housing budgets, sustained by local taxation, central government grants, and rental income. As Figure 1 indicates, the personal health services commanded a comparatively small element of "health" expenditure, though they enjoyed a growing share of resources in the interwar period. Public assistance represented a significant part, though this was not expanding in the same manner as the other services.
In sum then, where research projects seek to explore the extent, causes, and impacts of variations in local government health interventions, there are good grounds for defining these broadly. This better reflects the inter-war roles of public health doctors and local officials whose remit included both personal and environmental services, and it brings to bear the full range of inputs that might have affected population health. Indeed, as one local case study has revealed, a party health platform might explicitly advocate housing reform as an alternative to spending on services such as vaccination and TB; in this sense breadth is a sine qua non for studies of local health choices.60 That said, the more limited focus on the personal health services clearly holds some interest, given their later salience in the NHS debates. The next sections therefore turn to the methodological difficulties involved in using financial records as a source for these latter activities.
Personal Health Services under Local Government: A Regional Example
The discussion that follows draws on a study of health expenditure in a region of the southwest of England. It contains two large counties, Somerset and Gloucestershire, and three county boroughs, Bristol, Bath, and Gloucester. The counties were principally agricultural with declining coal industries, some tourism (Somerset), and textiles (Gloucestershire). Bristol had a population of about four hundred thousand and ranked the seventh largest city in England; it was the major seaport of the west, and its economy combined manufacturing, engineering, services, and distribution. Gloucester and Bath were both smaller, about fifty thousand and seventy thousand, respectively; the former was a river port, the latter a spa town with a large middle class. About three in five of the region's population resided in the administrative counties rather than the cities lying within them. Hence their inclusion permits consideration of whether the majority experience of rural and small-town dwellers differed from that of the more heavily studied urbanites.
There are two sets of sources through which local health expenditure, and by extension activity, may be gauged. The national collation of Annual Local Taxation Returns, renamed in 1934-35 the Local Government Financial Statistics (LGFS), includes a systematic categorization and tabulation of the personal health services for each county and county borough. However, because this return reports only a council's health committee spending, which was a component of its general rate fund account, the SMS and (from 1930) public assistance health expenditures are invisible, subsumed within the separate education and public assistance budgets. At local level however, each authority's treasurer's department produced annual abstracts, in which all accounts of the different spending departments were presented in considerable detail.61 From these it is possible to calculate, on a case-by-case basis, the education and public assistance components of personal health services spending, and thus to assess the significance of their absence from the LGFS.
Figure 2 draws on these local abstracts to show the combined five authorities' real per capita health expenditure between the financial years 1920-21 and 1939-40. The most striking feature is the steep rise in spending on the general rate fund, much observed at the national level by Lee and others because it corresponds to the data in the LGFS. This was mainly on curative services: TB and MCW programs, hospitals, VD clinics, and mental deficiency institutions. Crucially though, the apparently sharp increases in the 1930s were not all new expenditures. They also reflected various budgetary transfers from the public assistance committees (PACs) to health committees following the Local Government Act. These were the appropriations of Bristol's poor law hospital, Southmead, from 1930-31; two Somerset PAIs as mental deficiency institutions from 1931-32; a babies home hitherto under Bristol's PAC but administered by the health committee, and jointly funded from 1935-36; Gloucester's City General Hospital from 1936-37; and a Gloucestershire PAI as a maternity home from 1937-38.62 Complicating matters further, between 1933-34 and 1938-39, Bristol's Southmead Hospital charged its work to the rate fund account (under the general hospital, TB, mental deficiency, and maternity budgets), the education committee, and the PAC. Thus Bristol's recorded "general hospital" spending in the national LGFS was an artificially low figure for these years, apparently arrived at by totaling the costs of treatment of non-public assistance cases and of rents and recoupments; on average 47 percent of the true costs came from public assistance.
Figure 2.
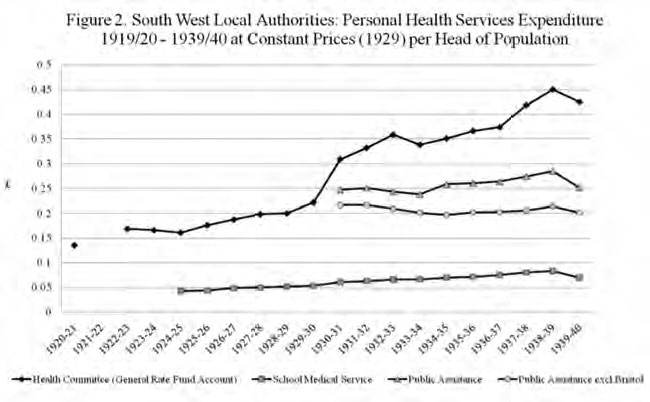
South Wast Local Authorities: Personal Health Services Expenditure 1919/20-1939/40 at Constant Prices (1929) per Head of Population
Of the health services activity unrecorded in the LGFS, SMS expenditure similarly grew, doubling in real terms, until budgets were squeezed during the Second World War. This spending was on schools for blind, deaf, "defective," and epileptic children and on medical inspection and treatment, so clearly merits inclusion alongside other personal health services.63 The SMS's institutional remit meant that some mental deficiency expenditure went unrecorded on the rate fund account. For example, Somerset County Council charged Yatton Hall to the rate fund, Street Special School to education, and Sandhill Park to both.64 Hence the LGFS figures understate actual mental deficiency work.
Public assistance health spending requires some elaboration before trends are discussed. It fell into three main categories, mental hospitals, the infirmary component of PAIs, and the medical aspect of domiciliary care. The latter has been omitted because in addition to remuneration of medical officers, drugs, and medicines, it included payments to sick people that were not disaggregated within the total "outdoor relief" budget. Mental hospital costs were substantial, accounting for around 45 percent of the graph's "public assistance" series, and clearly do merit inclusion. Mental hospital finances were shared between PACs and health committees, with the rate fund accounts (the portion visible in the LGFS) covering building expenses such as loan charges and material upkeep, and the PAC paying running costs, principally medical and nursing salaries and wages, clothing, drugs, fuel, and provisions. The other aspect, the infirmary element of the PAIs, is less straightforward because these institutions combined health and social care functions. Descended from the Victorian poor law workhouses, by the early twentieth century, they typically accommodated a mix of the "able-bodied" poor (vagrants, older people), the "infirm" (physically weak), mental patients, and the non-able-bodied poor (predominantly older sick people). Why do these deserve consideration as "municipal medicine"?
Examination of the regional evidence suggests that by the 1930s PAI health functions were such that they too should be included, albeit with some provisos. There were thirty-five PAIs in the region in 1900, of which only five were in the county boroughs. In 1948, the majority, twenty-two, entered the NHS as hospitals, of which twelve were geriatric, two maternity, three mental, three general, and two of an unknown type. Of the remainder, four had closed, the fate of a further four has not been ascertained (probably these too closed), while only three became old people's homes and two entered as "joint use" institutions, still combining health and social care under the NHS.65 These outcomes suggest that an interwar transition from workhouse to hospital occurred, which went beyond the five formal appropriations noted already. In Somerset, for example, the early 1930s saw the closure of most "casual wards" for the vagrant poor, and total numbers of "casuals" plummeted from 65,425 in 1931 to 12,535 in 1934 and about 3,696 in 1937.66 Official terminology began to change accordingly from 1932, with statistical returns now recording "patients" rather than "persons."67
Despite this, the PAIs undoubtedly retained some residents who were not sick, and the question arises of whether these can be quantified and expenditure duly adjusted downward. One strategy might be to estimate this based on the classification of beds as either "infirmary" (health) or "house" (social care) in PAC reports and elsewhere. Unfortunately, bed categories reflected administrative perceptions of care needs rather than the health status of "patients." In Bristol for example, Stapleton and Eastville PAIs had only 230 and 176 "aged or chronic sick" beds, out of 975 and 763, respectively.68 However, Stapleton's annual returns reveal that on average 78 percent of all residents (1932-42) were certified under the lunacy or mental deficiency acts. Essentially then, this was a long-stay hospital for older and mentally ill people, but with varying levels of nursing and medical requirements; it entered the NHS as such, renamed Manor Park Hospital in 1956.69 Similarly, Eastville's "house" beds accommodated "infirm" older people, but also "blind persons," "epileptics," and patients awaiting transfer to Southmead or Stapleton; such admissions were principally for skin conditions, septic feet, abscesses, chest conditions, and mental illness.70 As in the city, so in the rural PAIs. Visits by Somerset's MOH revealed that "mental cases" who were "generally bodily fit . . . have been included in the House figures," and officials agreed that "the able-bodied inmate who is not a mental case is very rare."71 Bed classification is therefore not a reliable gauge.
An alternative strategy for estimating the "social care" element might be to apply the proportions recorded in potentially more reliable cross-sectional surveys toward the end of the period. In Gloucestershire for example an institutional planning exercise classified 29 percent of PAI residents in December 1937 as "able-bodied," "old people," or "children," and the rest sick, infirm, or maternity patients.72 In 1948 in Somerset, exactly the same proportion, 29 percent, were transferred into old people's homes, with the remainder going into NHS hospitals.73 Tempting as it would be to use this figure for downward adjustment, its applicability throughout the period is uncertain, and again these classifications may have depended more upon assessments of whether a person required active nursing and doctoring rather than upon their diagnosis. Ultimately the boundary between health and social care is hopelessly blurred, for "the old and infirm grade insensibly into the sick."74 Thus any taxonomy is open to criticism. To classify all as "health" may be to collude with contemporaries who imposed a medical model onto states of impairment that were socially constructed.75 But equally, classifying all as "social care" may be to collude with those who incarcerated vulnerable older people in underresourced institutions where they languished without active medical therapy.76 On balance the decision here is to treat the whole PAI budget as health expenditure, deducting the costs of vagrancy where specified. Although unsatisfactory because it overinflates the hospital function (assuming this can ever be meaningfully disentangled from "care"), the local qualitative evidence suggests that in this region the PAIs were now predominantly health service institutions. The alternative, to exclude all non-mental hospital PAC expenditure, seems untenable.
With these caveats in mind, Figure 2 suggests that the public assistance budget did not increase in similar fashion that of other services. Indeed it fell in both the early 1930s and the 1940s, and these real declines cannot be attributed to appropriations because some occurred in years in which none took place. The gradual rise in the later 1930s was an artifact caused by one authority, Bristol, and partly reflects the unusual cost-sharing arrangement described above for its municipal general hospital. When Bristol is excluded, public assistance fell until the mid-1930s, not regaining its 1930 level until 1939-40. Thus the overall implication of the graph is that while local health care expenditures and activities targeted at children, mothers, and working-age adults were growing significantly, those for older people and the mentally ill were not.
The southwest region data also permit a detailed examination of the income that sustained such spending. This is important to the assessment of local health services. If principally funded by the rates, they may be understood as an embodiment of the will of local taxpayers; if by cost recovery from users ("recoupments"), then they were more akin to public utilities like water and gas; if by grants from the central government, then they were essentially local agents of national policy.
Table 1 shows the proportion of different health budgets not funded by the proceeds of local taxation, breaking income sources into recoupments (mostly user fees charged to patients or relatives) and direct Treasury grants. It suggests that each of these three readings is applicable to some extent, depending on the service. Rows 1-6 show health committee rate fund account income during the 1920s as recorded in the LGFS. User fees did not play a great part, other than for MCW in Bath and VD and MCW services in Gloucester. However, Treasury grants significantly underpinned activity. In this period they were given on a percentage basis according to the amount of rate-borne spending, meeting slightly less than half of MCW budgets and between one-half and two-thirds of TB, VD, and mental deficiency care. The series cannot be continued after 1929 when the Local Government Act, converted these state subventions to a single block grant whose subsidy to specific health budgets was not itemized. However, it seems plausible that the trajectories of expansion underpinned by grant income in the 1920s were continued in the 1930s. A key factor was the generosity of the block grant system, which introduced a new population-weighting formula to make resource allocation more responsive to need, while at the same time protecting places that would lose under the new system.77 Thus, for example, after 1929 Bristol lost £287,843 from the old grant and rating system, but gained £337,678 through the new weighting and protection formula, providing a fillip to spending capacity.78
Table 1.
Recoupments and Treasury Grants in Support of Health Expenditures, Southwest Local Authorities
| a. Mean % of budget from recoupments | b. Mean % of budget from treasury | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Som | Glos | Bath | Bristol | Glos | Som | Glos | Bath | Bristol | Glos | ||||||||||||||||
| CC | CC | CB | CB | CB | CC | CC | CB | CB | CB | ||||||||||||||||
| Note: MCW: maternity and child welfare; MD: mental deficiency; MH: mental hospital and mental deficiency; PA/MH: public assistance mental health; PAI: public assistance institutions; PH: total public health; SMS: school medical service; TB: tuberculosis; VD: venereal disease. Som CC: rows 3-8, from 1924-25 only; Glos CC: row 3 from 1921-22, row 5 from 1923-24, row 8 until 1942-43; Bristol: row 8 to 1939-40, rows 9 (including Southmead) 10 to 1938-39; Glos CB: row 8, 1931-32 to 1944-45, 1931-32 to 1936-37; row 9, 1931-32 to 1944-45; row 10, 1931-32 to 1937-38. In the CBs PH (row 1) is the sum of ID hospitals, TB, MCW, VD, notification, welfare of the blind, salaries of MOHs. NB, the absence of tuberculosis and mental deficiency data for Gloucestershire and Gloucester arises because the county and county borough operated joint committees with single accounts. | |||||||||||||||||||||||||
| Sources: As Figure 2, except PH and MH (rows 1 and 2) Ministry of Health, Annual Local Taxation Returns, England and Wales, 1919-20 to 1929-30. | |||||||||||||||||||||||||
| 1 | PH (1919-20 to 1929-30) | 8 | 5 | 12 | 5 | 27 | 41 | 23 | 30 | 32 | 11 | ||||||||||||||
| 2 | MH (1919-20 to 1929-30) | 5 | 2 | 3 | 5 | n/a | 28 | 0.13 | 18 | 39 | n/a | ||||||||||||||
| 3 | MCW (1919-20 to 1929-30) | 27 | 3 | 12 | 44 | 53 | 38 | 49 | 42 | ||||||||||||||||
| 4 | TB (1919-20 to 1929-30) | 3 | 5 | n/a | 54 | n/a | 59 | 54 | n/a | ||||||||||||||||
| 5 | VD (1919-20 to 1929-30) | 0 | 4 | 38 | 64 | 76 | 75 | 73 | 43 | ||||||||||||||||
| 6 | MD (1919-20 to 1929-30) | 5 | 5 | n/a | 47 | n/a | 42 | 52 | n/a | ||||||||||||||||
| 7 | SMS (1919-20 to 1929-30) | 11 | 3 | 6 | 7 | n/a | 62 | 61 | 53 | 56 | n/a | ||||||||||||||
| 8 | SMS (1919-20 to 1944-45) | 12 | 2 | 15 | 7 | 4 | 55 | 59 | 49 | 52 | 51 | ||||||||||||||
| 9 | PAI (1930-31 to 1939-40) | 4 | 22 | 30 | 35 | 0 | 0 | 0 | 0 | 0 | |||||||||||||||
| 10 | PA/MH (1930-31 to 1939-40) | 16 | 14 | 14 | 19 | 0 | 0 | 0 | 0 | 0 | |||||||||||||||
The SMS (rows 7-8) was also heavily supported by the Exchequer, which made an education grant to each authority and drew more modestly on recoupments from other local education committees, sales of work, and parental contributions.79 No direct state grants were recorded on the public assistance accounts (rows 10-11) for the PAIs and mental health.80 Here there was no trajectory of grant-supported expansion already under way and nothing beyond the recoupments, recovered at varying levels from patients and relatives. Thus when these income data are considered alongside Figure 2, it seems plausible to conclude that for this region the areas of local government health activity that displayed the most vigorous growth were those well supported by central funds.
The LGFS and the Local Abstracts Compared: Do the Discrepancies Matter?
This comprehensive picture of personal health services expenditures in a single region has revealed that local sources yield significant differences from the returns in the LGFS, and these discrepancies may now be summarized. Table 2 shows the proportion of such spending in the region's abstracts that was also represented in the LGFS. This reveals that when the SMS and public assistance are included the difference is substantial (though again the imprecision of the PAI "health" spending must be borne in mind). The LGFS include only about 40 percent of expenditure in the southwest authorities in the early 1930s, other than in Bristol, which had rapidly appropriated a large PAI. This then rose in the course of the 1930s as PA spending slowed relative to health spending on the rate fund account. Even so, by the late 1930s the "missing" portion remained large, notably in Bath, which chose not to appropriate its PAI.
Another way of viewing the discrepancies is to consider the more specific cost-sharing arrangements for mental hospitals. Figure 3 displays for the five authorities the proportion of institutional costs visible in the LGFS and those furnished from other funds. For good measure it also includes two other southern English county boroughs, Portsmouth and Southampton, as confirmation that the region's experience was not idiosyncratic. Organizational structures varied: for example, in Portsmouth only a small fraction (the loan charges) showed up in the LGFS public health budget, while the bulk was met by the mental health committee, which charged the major part to public assistance (the remainder coming from private patients, services personnel, and the criminal justice system). Bristol similarly established a separate mental health committee whose accounts excluded the small sums appearing in the LGFS, which consisted of loan charges and various maintenance costs for its Barrow Gurney and Fishponds sites. The other cities divided costs between public health and public assistance. The chart shows the extent to which public assistance budgets dominated the funding of mental hospitals and emphasizes the role of the poor law as the portal through which individuals became mental patients.
Figure 3.
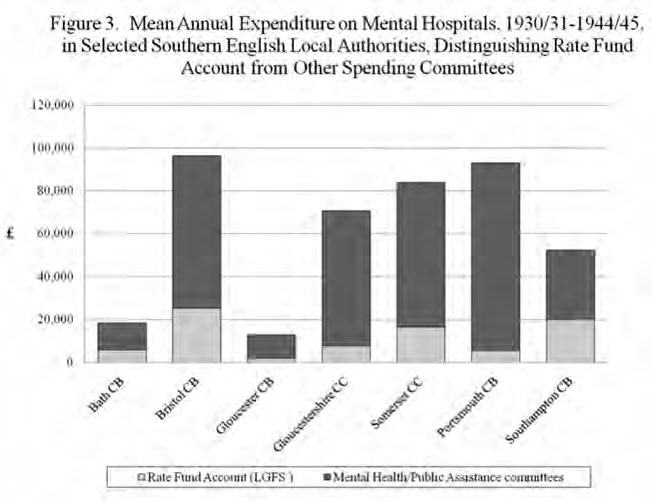
Mean Annual Expenditure on Mental Hospitals, 1930/31-1944/45, in Selected Southern English Local Authorities, Distinguishing Rate Fund Account from Other Spending Committees
Table 2.
Proportion of Personal Health Services Expenditures Shown in Local Government Financial Statistics: Southwest Authorities
| County boroughs | County councils | ||||
|---|---|---|---|---|---|
| Bath | Gloucester | Bristol | Somerset | Gloucestershire | |
| (%) | (%) | (%) | (%) | (%) | |
| Sources: As Figure 2; after 1936–37, the percentages refer to the health committee data on general rate fund accounts in the abstracts, which in previous years were identical to Local Government Financial Statistics figures. | |||||
| 1930–31 | 37 | 60 | 38 | 37 | |
| 1931–32 | 39 | 61 | 40 | 37 | |
| 1932–33 | 44 | 45 | 62 | 42 | 38 |
| 1933–34 | 44 | 46 | 60 | 44 | 39 |
| 1934–35 | 45 | 48 | 56 | 46 | 39 |
| 1935–36 | 46 | 47 | 58 | 46 | 40 |
| 1936–37 | 46 | 64 | 57 | 46 | 42 |
| 1937–38 | 49 | 64 | 58 | 49 | 44 |
| 1938–39 | 49 | 64 | 59 | 50 | 44 |
| 1939–40 | 45 | 68 | 64 | 49 | |
| 1940–41 | 34 | 78 | 48 | ||
Discussion
What are the implications of this local example for studies that use expenditure data to develop a national comparative overview? The comments that follow are directed principally at the work of Lee and of Levene, Powell, and Stewart, in this journal and elsewhere.
First, it is misleading to represent personal health services data drawn from the LGFS as capturing the totality of "municipal medicine" delivered by a given authority. They attest to only part of that activity and in some places less than half of it. This is not a trivial point, for if places are to be ranked according to their health efforts, or to have their spending priorities subjected to comparative assessment, this can be meaningfully done only in light of the whole range of these activities. For example, Levene et al. conducted a correlation exercise between rateable value and "public health expenditure" per head on the general rate fund account in the different county boroughs; they concluded that such a correlation "almost disappeared" after 1930, with the implication that local choice, not underlying prosperity, determined variation.81 Similarly they compared high- and low-spending boroughs according to the percentage of "county borough expenditure that went on health," at both individual and regional levels.82 But in the absence of health spending under education and public assistance, it is hard to see how these exercises can be a gauge of comparative "health" policy. There is also the more minor problem of distinguishing the relative significance of different types of expenditure: Lee assumed the largest category of "community care" was MCW, while Levene et al. thought TB schemes "always attracted the highest levels of investment." In the region, however, the school medical budget was close to and sometimes outstripped both.83
Second, without consideration of the interplay between health committee and public assistance budgets it is possible to misrepresent the course of health spending. Lee made no attempt to estimate the cumulative impact of transfers of poor law institutions on the "very rapid growth" of hospital expenditure in the 1930s, while Levene et al. assumed that the "transferred services are general hospitals and vaccination," and that by stripping these out the trend in new spending would be revealed.84 This is erroneous. The Local Government Act also aimed to ensure that mental deficiency, MCW, care of the blind, and tuberculosis services should be provided "otherwise than by way of poor relief."85 The regional case illustrated MCW and mental deficiency budgetary transfers, and these could be augmented by looking elsewhere. For instance, a hike in gross TB expenditure in Liverpool between 1934-35 (£143,544) and 1935-36 (£180,923) reflected the transfer of Cleaver Sanatorium.86 Therefore, without some idea of public assistance health expenditure as well, both before and after 1929, it is impossible to derive accurately trends in overall activity or compare spending between heads.
Third, and related to this, cost sharing across budgets could obscure trajectories of municipal general hospital spending. In their discussions of growth in this sector Levene et al. compared the sums committed by different county boroughs, on the assumption that these were captured under rate fund expenditure.87 Yet Bristol's Southmead was partially funded under public assistance, and hence the LGFS figure understated the true level of local commitment. More examples are needed to establish whether this was commonplace or idiosyncratic.
Fourth, and again related, the spreading of mental health costs across different budgets has also given rise to interpretative problems. Thomson's speculations about why Conservative authorities were more committed to mental deficiency were predicated on rankings of general rate fund account expenditure correlated with party strength. However, as he himself acknowledged, much activity took place under the education and PA committees, and the regional case reveals this was not visible in the LGFS data. The true relationship with party commitment is thus unobtainable at the national level. With respect to mental hospitals, Levene et al. presumed this component of the general rate fund was "spending on patients and on running costs," undertaking elaborate ranking and correlation exercises to compare performance between places.88 Observing the declining share of mental health spending against the rise of mental deficiency in the 1930s, they speculated that this represented a reclassification of cases.89 But unless the examples examined here are entirely anomalous, it arises instead because their figures were incomplete and represented only infrastructure costs.
Accurate presentation of mental hospital work also matters because it underlines the ongoing dependency of sufferers of mental distress on poor law arrangements. Bartlett has convincingly urged historians of nineteenth-century madness to treat the public asylum as an aspect neither of humanitarianism nor of medical professionalization, but essentially "as a Poor Law institution."90 From the early twentieth century this characterization is more easily overlooked: the 1924-26 Royal Commission on Lunacy and Mental Disorder recommended removing the distinction between private and pauper patients, then legislation in 1930 opened the asylums to voluntary admissions, shifted responsibility to county and county borough councils, and abolished poor law terminology.91 There was however no elevation of mental hospitals to the status of the acute general hospitals; within the NHS they remained underresourced, poorly staffed, and of low priority until a spate of scandals publicized this neglect in the 1960s and 1970s.92 Later, in the era of deinstitutionalization some commentators regarded the stigma and material hardship of recipients of community care as tantamount to pauperdom, emphasizing the continuities running through the century.93
Fifth, neglect of the income sources driving expenditure trends can obscure the extent to which the golden age of municipal medicine was created by central government. Perhaps because of their emphasis on localism and choice Levene et al. downplayed the role of Treasury support, observing only that the new block grant system in the 1930s "did not adversely affect" health services expenditure.94 This reading is plausible enough because unlike the earlier percentage grants, the block grant appears as a single lump sum on the rate fund account, so its precise impact on individual services is irrecoverable. However, it is more probable that the beneficial effect described for Bristol obtained more broadly. While the redistributive effects of the weighted population formula were in practice limited, the grant's overall level was considerably higher than the Treasury had intended.95 The amount was set in 1930 and fixed for three years, just before a dip in local rate-borne expenditure occasioned by the recession. Thus grant aid initially remained higher than it would have been under the former system of percentage grants (where state aid was proportionate to local spending). The principle of fixity over three-year spending tranches continued during a period of falling prices followed by mild inflation, so that through the 1930s the block grant "represented a net subsidy to local government compared to if . . . percentage grants had continued."96 It therefore seems likely that the scale of Exchequer support to health observable in the 1920s continued to influence 1930s spending patterns. Indeed, Levene et al.'s own results confirm this, with the spending growth on those services historically grant aided (VD, TB, MCW, mental deficiency) positively correlated with each other, while Powell observed a correlation in 1936-37 between MCW expenditure and level of block grant.97 Instead of "investment choices," then, we might think of the system as combining elements of genuine devolution with "delegation" (where local authorities act as agents of central government policy).98 Indeed the contribution of local revenues to all local authority current expenditure fell from 70 percent in 1920 to 56 percent in 1938, as dependence on central government grants rose.99
Finally, concentration on the urban scene risks overlooking related or contrary developments in the surrounding areas. Some issues are minor and technical, such as the neglect of joint county/county borough committees, like those of Gloucestershire and Gloucester for TB and mental deficiency, where the LGFS statistics represent contributions to these pooled funds.100 The larger point is that the county experience directs attention to services in PAIs. Levene's later study of ex-poor law institutions remaining under public assistance in the county boroughs is suggestive of a lack of development compared to the municipal acute sector.101 However it was in the counties where appropriation advanced least. Qualitative evidence amply supports the assumption that flat expenditure signaled an inadequate service. The hospital surveys conducted in the 1940s used terms like "imperfections and frank defects," "little to recommend it," "poor quality," "falls short of present-day requirements," and "inherent deficiencies" to describe Somerset's institutions, many of which dated back to the mid-nineteenth century.102 Meanwhile, as with mental hospitals, the population at need was growing, as older people increasingly survived acute illness to live on with chronic conditions.103 Thus the two county councils' experiences conform to Bevan's critique of many local authorities as too poor and "helpless" to modernize hospitals that were "monstrous buildings, a cross between a workhouse and a barracks."104
Conclusion
Establishing the optimal balance between central direction and local autonomy is an important problem in health services research. In the British case policy debate on this subject has been recurrent since the start of NHS, with a recent intensification of political rhetoric about devolving power and reviving democratic legitimacy.105 Historians too have sought to reappraise the record of local government health services before the NHS, interrogating the Bevanite claim that greater equity and efficiency were compromised by local control. Research designs have ranged from case studies to comparative national surveys that use the rich data set of local government financial statistics to gauge levels of activity. The picture emerging is of a sector experiencing vigorous growth, where spatial variation was in part determined by underlying prosperity, but also by local choice. To advance further, work is now needed to illuminate how, or indeed whether, voter preferences were translated into policy trajectories, and, most importantly, to explore the performance of the local state in improving health outcomes.
The regional study presented here has highlighted various conceptual and methodological issues that might inform this ongoing work. It was argued first that analysis of local health policies, and their relationship with trends in health indicators, ought to proceed from a broad definition of local government health activity. Inclusion of environmental interventions and housing alongside curative services better reflects the range of activities undertaken by health departments, and captures all the policy levers available to local officials seeking to raise population health. The case of the southwest was then used to comment on studies limited to the personal health services that draw on national summary statistics. Comparison with local data suggested that the latter gave only a partial picture, and in particular understated services for schoolchildren, mental hospital patients, and people with chronic illnesses. It also revealed various technical budgetary issues that complicate the use of the nationally collated data as a precise measure of different categories of expenditure.
The assumption here has been that generalization from the case study about the differences between local and national financial records is justified, though work on treasurers' abstracts and public assistance data elsewhere may refute this, or complicate the picture further. Where generalization is clearly not warranted is from the analysis of southwest-specific income and expenditure trends. Nonetheless, the regional case raises intriguing questions for future research. Here spending on the public assistance element of the health budget was less buoyant than in other sectors, despite growing need for long-term care. If this pattern obtained elsewhere, particularly in places outside the main urban centers, then Bevan's argument about local failure to develop services may gain credibility. Consideration of income sources highlighted the importance of central subsidy to the growth areas of local government health work. Again, if future work confirms the broadly positive impact of the grant system, this too would throw into sharp relief the abandonment of localism in 1948, though emphasizing continuity rather than rupture.
Acknowledgments
The research on which this article is based was sponsored by the Wellcome Trust (award no. 070880/Z/03), whose support is gratefully acknowledged.
Biography
Martin Gorsky is senior lecturer in the Contemporary History of Public Health in the Centre for History in Public Health at the London School of Hygiene and Tropical Medicine. His research interests lie in the history of public health and health services in Britain, Europe, and America in the nineteenth and twentieth centuries. He has published widely on the development of the British voluntary hospitals and of mutual associations such as friendly societies and hospital contributory schemes.
Footnotes
World Health Organization. The World Health Report 2000. Health Systems: Improving Performance. Geneva: WHO; 2000. pp. xvipp. 68–69. Mills Anne, Vaughan J. Patrick, Smith Duane. L., Tabibzadeh Iraj. eds., Health System Decentralization: Concepts, Issues and Country Experience Geneva: WHO; 1990. Mills Anne. Decentralization and Accountability in the Health Sector from an International Perspective: What Are the Choices? Pub. Admin. Dev. 1994;14:281–292.
Hutchinson Paul, Akin John, Ssengooba Freddie. The Impacts of Decentralization on Health Care Seeking Behaviors in Uganda. Internat. J. Health Planning Mgmt. 2006;21:239–270. doi: 10.1002/hpm.848.
Hutchinson Paul, Akin John, Ssengooba Freddie. The Impacts of Decentralization on Health Care Seeking Behaviors in Uganda. Internat. J. Health Planning Mgmt. 2006;21:239–270. doi: 10.1002/hpm.848. Wang Yan, Collins Charles, Tang Shenglan, Martineau Tim. Health Systems Decentralization and Human Resources Management in Low and Middle Income Countries. Pub. Admin. Dev. 2002;22:439–453.
Saltman Richard B., Bankauskaite Vaida, Vrangbaek Karsten. eds., Decentralization in Health Care: Strategies and Outcomes Maidenhead, UK: Open University Press; 2007. Ashton John. ed., Healthy Cities Milton Keynes, UK: Open University Press; 1992.
Wyss K., Lorenz N. Decentralization and Central and Regional Coordination of Health Services: The Case of Switzerland. Internat. J. Health Planning Mgmt. 2000;15:103–114. doi: 10.1002/1099-1751(200004/06)15:2<103::AID-HPM581>3.0.CO;2-S.
The concept is not used here to signify the devolving of powers once held by the center, cf. Dunlop Judith M. Social Policy Devolution: A Historical Review of Canada, the United Kingdom, and the United States (1834-1999) Soc. Work Pub. Health. 2009;24:191–209. doi: 10.1080/19371910802595281.
Finer Herman. English Local Government 3rd ed. 1933. repr., London: Methuen; 1946. 377–392. 462–466.
Finer Herman. English Local Government 3rd ed. 1933. repr., London: Methuen; 1946. 5 20–21.
Ministry of Health. A National Health Service. London: HMSO; 1944. p. 12.p. 14.
Webster Charles. The Health Services since the War: Volume I, Problems of Health Care, the National Health Service before 1957. London: HMSO; 1988. p. 21.p. 24.
Bevan Aneurin. 422 HC Deb. Apr 30, 1946. 5s. cols. 48-49. Webster Charles. Birth of a Dream: Bevan and the Architecture of the National Health Service in The State of the Nation: The Political Legacy of Aneurin Bevan ed. Goodman Geoffrey. London: Victor Gollancz; 1998. 106–229. National Archives: Public Record Office MH 80/34, Bevan A. Draft Cabinet Paper: National Health Service. The Future of the Hospital Service. p. 4.
Bevan A. Draft Cabinet Paper: National Health Service. The Future of the Hospital Service. p. 4. Klein Rudolf. The New Politics of the NHS: From Creation to Reinvention 5th ed. 1983. repr., Oxford: Radcliffe; 2006. 13–15.
Campbell John. Nye Bevan and the Mirage of British Socialism. London: Weidenfeld & Nicolson; 1987. pp. 176–179. Lowe Rodney. The Welfare State in Britain since 1945 1993. repr., Basingstoke: Palgrave Macmillan; 2005. 184–185. Stewart John. Ideology and Process in the Creation of the British National Health Service. J. Policy Hist. 2002;14:113–134.
Levene Alysa, Powell Martin, Stewart John. Investment Choices? County Borough Health Expenditure in Inter-War England and Wales. Urb. Hist. 2005;32:434–458. Levene, Powell, Stewart The Development of Municipal General Hospitals in English County Boroughs in the 1930s. Med. Hist. 2006;50:3–28. doi: 10.1017/s002572730000942x. Taylor Becky, Powell Martin, Stewart John. Central and Local Government and the Provision of Municipal Medicine, 1919-39. Engl. Hist. Rev. 2007;122:397–426.
Levene Alysa, Powell Martin, Stewart John. Patterns of Municipal Health Expenditure in Interwar England and Wales. Bull. Hist. Med. 2004;78:635–669. doi: 10.1353/bhm.2004.0130.
Crowther M. A. The Workhouse System, 1834-1929: The History of an English Social Institution. London: Methuen; 1981. pp. 156–190.
Cherry Steven. Medical Services and the Hospitals in Britain, 1860-1939. Cambridge, UK: Cambridge University Press; 1996. pp. 41–78. Hardy Anne. Health and Medicine in Britain since 1860. Basingstoke: Palgrave; 2001. pp. 9–39.
Harris Bernard. The Health of the Schoolchild: A History of the School Medical Service in England and Wales. Buckingham: Open University Press; 1995. Harris . The Origins of the British Welfare State: Society, State, and Social Welfare in England and Wales, 1800-1945. Basingstoke: Palgrave Macmillan; 2004. pp. 178–179.pp. 234–240. Marks Lara. Metropolitan Maternity: Maternal and Infant Welfare Services in Early Twentieth-Century London. Amsterdam: Rodopi; 1996. Political and Economic Planning (PEP) Report on the British Health Services. London: PEP; 1937. pp. 276–293. chap. iv. Bryder Linda. Below the Magic Mountain: A Social History of Tuberculosis in Twentieth-Century Britain. Oxford: Clarendon Press; 1988. pp. 36–45.pp. 70–96. Thomson Mathew. The Problem of Mental Deficiency: Eugenics, Democracy and Social Policy in Britain c.1870-1959. Oxford: Clarendon Press; 1998. Yelling J. A. Slums and Redevelopment: Policy and Practice in England 1918-45, with Particular Reference to London. London: UCL Press; 1992.
Abel-Smith Brian. The Hospitals, 1800-1948: A Study in Social Administration in England and Wales. Cambridge, Mass.: Harvard University Press; 1964. pp. 352–383. Mohan John. Planning, Markets and Hospitals. London: Routledge; 2002. pp. 37–42.
Lindsay Almont. Socialized Medicine in England and Wales: The National Health Service, 1948-1961. Chapel Hill: University of North Carolina Press; 1962. pp. 17–21. Eckstein Harry. The English Health Service: Its Origins, Structure, and Achievements. Cambridge, Mass.: Harvard University Press; 1964. pp. 29–33. quotation on 31.
Pater John E. The Making of the National Health Service. London: King Edward's Hospital Fund for London; 1981. pp. 19–20.
Abel-Smith Hospitals. n. 19), chap. 23.
Webster Health Services. pp. 5–9. n. 10.
Harris Health of the Schoolchild. pp. 112–115. n. 18. Harris Origins of the British Welfare State. pp. 251–253.pp. 259 n. 18.
See Gorsky Martin. Public Health in Interwar Britain: Did It Fail? Dynamis. 2008;28:175–198. doi: 10.4321/s0211-95362008000100008.
Dupree Marguerite. The Provision of Social Services in The Cambridge Urban History of Britain, 1840-1950, Vol. III ed. Daunton Martin. Cambridge, UK: Cambridge University Press; 2000. 351–394. quotation on 391.
Sheard Sally. Reluctant Providers? The Politics and Ideology of Municipal Hospital Finance 1870-1914 in Financing Medicine: The British Experience since 1750 ed. Gorsky Martin, Sheard Sally. London: Routledge; 2006. 112–129. Willis Tim. The Bradford Municipal Hospital Experiment of 1920: The Emergence of the Mixed Economy in Hospital Provision in Inter-War Britain in Gorsky, Sheard Financing Medicine 130–144. Gorsky Martin. 'Threshold of a New Era': The Development of an Integrated Hospital System in Northeast Scotland, 1900-39. Soc. Hist. Med. 2004;17:247–267.
Powell Martin. Hospital Provision before the NHS: Territorial Justice or Inverse Care Law? J. Soc. Policy. 1992;21:145–163. Powell A Tale of Two Cities: A Critical Evaluation of the Geographical Provision of Health Care before the NHS. Pub. Admin. 1992;70:67–80.
Powell Martin. An Expanding Service: Municipal Acute Medicine in the 1930s. Twent. Cent. Brit. Hist. 1997;8:334–357. doi: 10.1093/tcbh/8.3.334.
Welshman John. Municipal Medicine: Public Health in Twentieth Century Britain. Bern: Peter Lang; 2000. Welshman The Medical Officer of Health in England and Wales, 1900-1974: Watchdog or Lapdog? J. Pub. Health Med. 1997;19:443–450. doi: 10.1093/oxfordjournals.pubmed.a024675. Gorsky Public Health in Interwar Britain. n. 25.
Thomson Problem of Mental Deficiency. pp. 149–179. n. 18. Marks Metropolitan Maternity. n. 18. Harris Health of the Schoolchild. pp. 109–112. n. 18.
Marks Metropolitan Maternity. pp. 158–160.pp. 190–191. n. 18. Thomson Problem of Mental Deficiency. p. 223. n. 18. Willis Tim. Contributing to a Real Socialist Commonwealth: Municipal Socialism and Health Care in Sheffield (1918-1930) in Der Munizipalsozialismus in Europa ed. Kühl U. Munich: Oldenbourg; 2001. 101–115. Stewart John. 'For a Healthy London': The Socialist Medical Association and the London County Council in the 1930s. Med. Hist. 1997;41:417–436. doi: 10.1017/s002572730006302x.
Daunton Martin. Book Review: Lara V. Marks, 'Metropolitan Maternity: Maternal and Infant Welfare Services in Early-Twentieth-Century London,'. Med. Hist. 1998;42:251–252.
Preston Brian. Rich Town, Poor Town: The Distribution of Rate-Borne Spending Levels in the Edwardian City System. Trans. Inst. Brit. Geog. 1985;10:77–94. quotation on 86.
Lee Roger. Uneven Zenith: Towards a Geography of the High Period of Municipal Medicine in England and Wales. J. Hist. Geog. 1988;14:260–280. doi: 10.1016/s0305-7488(88)80222-6. esp. 269, quotations on 271.
Thomson Problem of Mental Deficiency. pp. 223–224. n. 18. Powell Martin. Did Politics Matter? Municipal Public Health Expenditure in the 1930s. Urb. Hist. 1995;22:360–379.
Levene, Powell, Stewart Investment Choices? p. 457. n. 14. Levene, Powell, Stewart Patterns of Municipal Health Expenditure. pp. 641–643.pp. 647pp. 649 n. 15.
Levene, Powell, Stewart Patterns of Municipal Health Expenditure. p. 642. n. 15. (referencing Powell Did Politics Matter? p. 363. n. 36.
Levene, Powell, Stewart Municipal Health Expenditure. p. 649. n. 15. Levene, Powell, Stewart Investment Choices? p. 435. n. 14.
Levene, Powell, Stewart Investment Choices? p. 437. n. 14.
Lee Uneven Zenith. pp. 261–263. n. 35. Levene, Powell, Stewart Patterns of Municipal Health Expenditure. p. 639. n. 15.
Welshman Municipal Medicine. n. 30. Thompson Steven. Unemployment, Poverty and Health in Interwar South Wales. Cardiff: University of Wales Press; 2006. pp. 102–154.
Levene, Powell, Stewart Patterns of Municipal Health Expenditure. p. 636. n. 15. Levene, Powell, Stewart Investment Choices? p. 436. n. 14. Ministry of Health. National Health Service. p. 6. n. 9.
Lee Uneven Zenith. p. 269. n. 35. n33. his underlying source is Foster Christopher D., Jackman Richard, Perlman Morris. Local Government Finance in a Unitary State. London: Allen & Unwin; 1980. pp. 102–109. appendix 1.4.A1.
Levene, Powell, Stewart Patterns of Municipal Health Expenditure. p. 636. n. 15.
Marmot Michael. Fair Society, Healthy Lives. London: Marmot Review; 2010.
For example, Bath Record Office (BRO) City of Bath, Annual Report of the Medical Officer of Health and of the Chief Sanitary Inspector, 1919-46. Bristol Record Office (BrRO) City and County of Bristol Annual Report of the Medical Officer of Health, 1918-36, City and County of Bristol: Annual Report of the Department of Public Health, 1936-46 (Bristol MOH) 33416 13a-24. Gloucestershire Archives (GA), CM/R1/ 14/41/2. Gloucestershire County Council, Annual Report of the Medical Officer of Health for the Administrative County of Gloucester, 1921-38. and GA 14/37/5 IPB. Annual Reports of the Medical Officer of Health for the City and Port of Gloucester, 1919-45. Somerset Archive and Record Service (SARS), C/PHH/76. Somerset County Council, Report of the Medical Officer of Health, 1918-46 (Som CC MOH)
Harris Origins of the British Welfare State. p. 241. n. 18. anon. The Croydon Typhoid Inquiry. Brit. Med. J. 1938 Feb 19;1:404–407. quotation on 404; Thompson Unemployment, Poverty and Health. pp. 140–141. n. 42.
Som CC MOH. 1929. pp. 42–43. 1930, 35-69; 1945, 31; Savage William. Practical Public Health Problems. London: J. A. Churchill; 1941.
See Marmot Fair Society. pp. 77–81.pp. 130–132. n. 46.
PEP. Report. pp. 36–42. n. 18. see, e.g., Gove Walter R., Hughes Michael, Galle Omer R. Overcrowding in the Home: An Empirical Investigation of Its Possible Pathological Consequences. Amer. Sociol. Rev. 1979;44:59–80. Wanyeki Ian, Olson Sherry, Brassard Paul, Menzies Dick, Ross Nancy, Behr Marcel, Schwartzman Kevin. Dwellings, Crowding, and Tuberculosis in Montreal. Soc. Sci. Med. 2006;63:501–511. doi: 10.1016/j.socscimed.2005.12.015.
Hardy Health and Medicine. p. 88.p. 100. n. 17. Wilson Scott. The Public Health Services in Improving the Common Weal: Aspects of Scottish Health Services 1900-1984 ed. McLachlan Gordon. Edinburgh: Edinburgh University Press; 1987. 277–321. McFarlane Neil. Hospitals, Housing, and Tuberculosis in Glasgow, 1911-51. Soc. Hist. Med. 1989;2:59–85. doi: 10.1093/shm/2.1.59. Shapely Peter. The Politics of Housing: Power, Consumers and Urban Culture. Manchester: Manchester University Press; 2007. pp. 122–128.
See Jackson Mark. ed., Health and the Modern Home New York: Routledge; 2007
Nolte Ellen, McKee Martin. Population Health in Europe: How Much Is Attributable to Health Care? World Hosp. Health Serv. 2004;40:12–14.
Hardy Health and Medicine. p. 90. n. 17. Webster Charles. Public Health in Decline. Health Matters. 1992;11:10–11. quotation on 10; McFarlane Hospitals, Housing, and Tuberculosis. n. 52. Bryder Below the Magic Mountain. pp. 197–198.pp. 258–260. n. 18. Niemi Marjaana. Public Health and Municipal Policy Making: Britain and Sweden, 1900-1940. Aldershot: Ashgate; 2007. pp. 113–158.
Shapely Politics of Housing. n. 52.
Ashby Eric, Anderson Mary. The Politics of Clean Air. Oxford: Oxford University Press; 1981.
There are no published data for 1921-22.
Local returns of "outdoor relief," later "domiciliary assistance," consulted here include details of drugs, medicines, and medical officers' salaries, but do not distinguish financial aid to maintain the sick in the home from doles given to the healthy.
Willis Contributing to a Real Socialist Commonwealth. pp. 105–107. n. 32.
For example, BRO. City of Bath, Abstract of Accounts . . . 1921. 1945. BrRO. City and County of Bristol: Epitome and General Statistics of the City Accounts for the Year Ended . . . 1921. 1947. GA. Gloucestershire County Council, Abstract of Accounts, 1918-47, City of Gloucester, Abstract of Accounts . . . 1931. 1944. SARS, C/F/217. Administrative County of Somerset: An Abstract of the Accounts of the County Council . . . 1924. 1946.
Somerset: Shepton Mallet, Long Ashton PAIs; Gloucestershire: Tetbury PAI became Cotswold Maternity Home and Children's Hospital; Bristol Babies Home: see Bristol MOH. 1934. pp. 4–5. n. 47. Bristol Abstract. 1935. 1936. p. 40.p. 90. n. 61. (appropriated under the Maternity and Child Welfare Act 1918).
Though arguably health related, school meals are excluded here.
Somerset Abstract. 1927. 1928. n. 61.
The original data set was compiled from "Return showing in respect of each Union and Parish the number of persons over 60 years of age in Receipt of Relief from the Guardians on 1st September 1903," British Sessional Papers House of Commons 1904, lxxxii, 453-65, and subsequent institutional histories traced principally in GA CW/M1/2. Gloucestershire County Council Public Assistance Department, Report of the County Public Assistance Officer as to Institutional Accommodation in the Administrative County of Gloucester. 1937. GA CW/M1/2-3. Public Assistance Committee Minutes. 1938. 1948. passim. SRO C/WS/1/5. Public Assistance Reports. passim. SRO C/WS/2/57, Glass W. T. The National Health Service Act, 1946. The National Assistance Bill: Public Assistance Institutions. Report of the Public Assistance Officer. Jan 01, 1948. SRO C/WS/2/37. Somerset Public Assistance Homes for Old People 1943-54. and the South West Regional Health Authority Hospital Management Committee returns at BrRO 40837/1 Avon, 40837/5 Gloucestershire, 40837/6 Somerset.
Closures: SARS C/WS/PA 1. Somerset County Council: Public Assistance Committee Minute Book from Dec, 1929. to Dec, 1932. Mar 16, 1931. Long Ashton, Shepton Mallet, Keynsham, June 16, 1931, Clutton, Wells, Langport, Frome, September 27, 1932 Dulverton, Taunton, Yeovil, Wells and Wincanton; tramping routes: SARS C/WS/1/5. Public Assistance Reports. Jun 14, 1932. and passim; after 1936 only final quarter totals were given, from which the 1937 figure is extrapolated.
SARS C/WS/1/5. Public Assistance Reports. Sep 27, 1932.
Cope Zachary, Gill W. J., Griffiths Arthur, Kelly G. C. Ministry of Health: Hospital Survey, the Hospital Services of the South-Western Area. London: HMSO; 1945. p. 34.
Bristol MOH. pp. 1932–1942. passim (n. 47)
Cope, et al. Hospital Survey. p. 34. n. 68. Bristol MOH. 1934. pp. 127–130. 1935, 150.
SARS C/WS/2/57, Savage W. G. Somerset County Council Health Department: A Preliminary Report upon the Accommodation for the Sick and Other Inmates in Poor Law Institutions in Somerset. Feb 12, 1930. pp. 2–3.pp. 10–11.
GA CW/M1/2. Institutional Accommodation. pp. 73–74. n. 65.
SARS C/WS/1/5. Public Assistance Reports. Jun 17, 1947.
SARS C/WS/2/57. Preliminary Report. p. 2. n. 71.
Oliver Michael. The Politics of Disablement. London: Macmillan; 1990. pp. 46–54.
Thane Pat. Old Age in English History: Past Experiences, Present Issues. Oxford: Oxford University Press; 2000. pp. 436–438.
Bristol: City Accounts. 1931. 1932. pp. 6–7. n. 61. the new weighting incorporated unemployment levels and numbers of under5s and rateable values and was phased in to cushion impacts on losers: 25 percent for the first seven years, rising to 50 percent thereafter, and 75 percent after twelve years; the block grant also compensated for the derating of industrial properties.
Bristol: City Accounts. 1933. 1934. pp. 4–6. n. 61.
Since the SMS was funded from the education budget and (from 1918) without a specific grant, the percentages shown in Table 1 represent the subsidies of the overall education budgets.
The domiciliary assistance accounts, excluded here, recorded Ministry of Health grants under the Unemployment Assistance (Temporary Provisions) Acts 1935-36, and there were trivial sums for staff of children's homes under the Widow, Orphans and Old Age Contributory Pensions Act.
Levene, Powell, Stewart Patterns of Municipal Health Expenditure. p. 655. n. 15.
Levene, Powell, Stewart Patterns of Municipal Health Expenditure. pp. 656–668. n. 15. quotation on 656.
Lee Uneven Zenith. p. 270. n. 35. Levene, Powell, Stewart Investment Choices? p. 438. n. 14. e.g., Bath CB 1919-20 to 1939-40: SMS £158,523, TB £65,069, MCW £121,123; Bristol CB 1919-20 to 1939-40: SMS £856,901, TB £959,799, MCW £509,041.
Lee Uneven Zenith. p. 268. n. 35. Levene, Powell, Stewart Patterns of Municipal Health Expenditure. pp. 646–648. n. 15. quotation on 648.
Halsbury's Statutes. pp. 888–889. 19 Geo.5 Local Government Act 1929, section 5.
Liverpool Record Office. The Accounts of the Treasurer of the City of Liverpool. 1935. 1936.
Levene, Powell, Stewart Patterns of Development of Municipal General Hospitals. pp. 21–22. n. 14.
Levene, Powell, Stewart Patterns of Municipal Health Expenditure. p. 650. n. 15. Levene, Powell, Stewart Investment Choices? pp. 441–446. n. 14.
Levene, Powell, Stewart Municipal Health Expenditure. p. 647. n. 15. see also Levene, Powell, Stewart Investment Choices? pp. 445–446. n. 14.
Bartlett Peter. The Asylum and the Poor Law: The Productive Alliance in Insanity, Institutions and Society, 1800-1914: A Social History of Madness in Comparative Perspective ed. Melling Joseph, Forsythe Bill. London: Routledge; 1999. 48–67. Barham Peter. Closing the Asylum: The Mental Patient in Modern Society. London: Penguin; 1992. pp. 68–75.
Jones Kathleen. Mental Health and Social Policy 1845-1959. London: Routledge Kegan Paul; 1960. pp. 106–121.
Webster Health Services. pp. 326–340. n. 10.
Barham Closing the Asylum. pp. 104–109. n. 90.
Levene, Powell, Stewart Patterns of Municipal Health Expenditure. p. 655. n. 15. n40. Levene, Powell, Stewart Investment Choices? p. 655. n. 14. n18.
Bradbury Jonathan P. The 1929 Local Government Act: The Formulation and Implementation of the Poor Law (Health Care) and Exchequer Grant Reforms for England and Wales (Outside London) University of Bristol; 1990. pp. 235–238.pp. 246–249. Ph.D. thesis.
Bradbury Jonathan P. The 1929 Local Government Act: The Formulation and Implementation of the Poor Law (Health Care) and Exchequer Grant Reforms for England and Wales (Outside London) University of Bristol; 1990. pp. 253–254.pp. 258–265.pp. 357–358. Ph.D. thesis.
Levene, Powell, Stewart Patterns of Municipal Health Expenditure. p. 650. n. 15. Powell Did Politics Matter? pp. 376–377. n. 36.
Mills Anne. Decentralization Concepts and Issues: A Review in Mills, et al. Health System Decentralization n. 1 9–42.
Peacock Allan T., Wiseman Jack. The Growth of Public Expenditure in the United Kingdom 1961. repr., London: Allen & Unwin; 1967. 99–105.
Levene, Powell, and Stewart assume only the possibility of collaboration between boroughs, citing Gloucester as an example of an isolated authority that would find such joint working difficult: Patterns of Municipal Health Expenditure. p. 656. n. 15.
Levene A. Between Less Eligibility and the NHS: The Changing Place of Poor Law Hospitals in England and Wales, 1929-39. Twent. Cent. Brit. Hist. 2009;20:322–345. doi: 10.1093/tcbh/hwp018.
Cope, et al. Hospital Survey. p. 57. n. 68.
Thane Old Age. p. 438. n. 76.
Bevan A. 422 H.C.Deb. Apr 30, 1946. 5 s. col. 49.
Klein Rudolf. The Eternal Triangle: Sixty Years of the Centre-Periphery Relationship in the National Health Service. Soc. Policy Admin. 2010;44:285–304. Invitation to Join the Government of Britain: The Conservative Manifesto 2010. London: Conservative Party; 2010. pp. 45–48.


