Abstract
Introduction
Although tracheal intubation (TI) in the pre-hospital setting is regularly carried out by emergency medical service (EMS) providers throughout the world, its value is widely debated. Heterogeneity in procedures, providers, patients, systems and stated outcomes, and inconsistency in data reporting make scientific reports difficult to interpret and compare, and the majority are of limited quality. To hunt down what is really known about the value of pre-hospital TI, we determined the rate of reported Utstein airway variables (28 core variables and 12 fixed-system variables) found in current scientific publications on pre-hospital TI.
Methods
We performed an all time systematic search according to the PRISMA guidelines of Medline and EMBASE to identify original research pertaining to pre-hospital TI in adult patients.
Results
From 1,076 identified records, 73 original papers were selected. Information was extracted according to an Utstein template for data reporting from in-the-field advanced airway management. Fifty-nine studies were from North American EMS systems. Of these, 46 (78%) described services in which non-physicians conducted TI. In 12 of the 13 non-North American EMS systems, physicians performed the pre-hospital TI. Overall, two were randomised controlled trials (RCTs), and 65 were observational studies. None of the studies presented the complete set of recommended Utstein airway variables. The median number of core variables reported was 10 (max 21, min 2, IQR 8-12), and the median number of fixed system variables was 5 (max 11, min 0, IQR 4-8). Among the most frequently reported variables were "patient category" and "service mission type", reported in 86% and 71% of the studies, respectively. Among the least-reported variables were "co-morbidity" and "type of available ventilator", both reported in 2% and 1% of the studies, respectively.
Conclusions
Core data required for proper interpretation of results were frequently not recorded and reported in studies investigating TI in adults. This makes it difficult to compare scientific reports, assess their validity, and extrapolate to other EMS systems. Pre-hospital TI is a complex intervention, and terminology and study design must be improved to substantiate future evidence based clinical practice.
Introduction
Tracheal intubation (TI) to secure the airway of severely ill or injured patients is a critical intervention regularly conducted by emergency medical service (EMS) providers throughout the world. This activity is based on the assumption that, in keeping with in-hospital practice, a compromised airway should be secured as early as possible to ensure adequate ventilation and oxygenation. However, because pre-hospital environmental and infrastructural factors can be challenging, intubation success rates are variable [1]. When TI is performed incorrectly, it can provoke adverse events and may worsen outcome in some patient groups [2-4]. Even when performed correctly, suboptimal ventilation following TI may increase the risk of fatal outcomes in certain patient subgroups [5-9].
The use of pre-hospital TI is widely debated [see Additional data file 1], but the majority of TI-related studies are thought to be of limited value [10-12]. The core question therefore remains unanswered: does TI in the pre-hospital setting fail or result in adverse events at rates that exceed the benefits of adequately performed TI?
Rapid sequence induction (RSI) and TI are regarded as the standard of care for airway management during in-hospital emergencies. It seems reasonable that this practice should be applied in the pre-hospital phase to prevent delay in good oxygenation and ventilation. However, because of available expertise and pre-hospital external factors, several alternatives to RSI and TI are practised. Environment, equipment, procedures, provider competence, practical skills, and drug protocols vary between emergency rooms and emergency medical service (EMS) systems [13], among EMS systems [14,15], and within EMS systems [16,17]. These variations have been reported to influence the frequency and quality of TI and, in all likelihood, patient outcome [1,18].
However, the heterogeneity of procedures, providers, patients, systems and monitored outcomes makes the published scientific reports difficult to interpret and compare, and inconsistency in the types of data reported exacerbates the problem. To improve reporting, an international expert panel published a consensus-based, Utstein-style template for the uniform reporting of data on pre-hospital advanced airway management [19]. The template defines inclusion criteria along with 28 core variables and 19 optional variables for documenting and reporting data. The 28 core variables are in three groups: "system variables", "patient variables", and "post-intervention variables" (Table 1). In addition, the template recommends that 12 fixed-system variables be reported (Table 2) to accurately describe the particular EMS system from which the data were collected.
Table 1.
The 28 core variables for uniform reporting of data from advanced airway management in the field
| Data variable name | Data variable categories or values | Definition of data variable |
|---|---|---|
| System variables | ||
| Highest level of EMS provider on scene | 1 = EMS non-P 2 = EMS-P 3 = Nurse 4 = Physician 5 = Unknown |
Highest level of EMS provider on scene, excluding any non-EMS personnel (e.g., bystanders, family etc) |
| Airway device available on scene | 1 = BMV 2 = Extraglottic device 3 = ETT 4 = Surgical airway 5 = None 6 = Unknown |
Airway devices available on scene and provider on scene who knows how to use it |
| Drugs for airway management available on scene | 1 = Sedatives 2 = NMBA 3 = Analgetics/opioids 4 = Local/topic anaesthetic 5 = None |
Drugs used for airway management, available on scene and someone competent to administer |
| Main type of transportation | 1 = Ground ambulance 2 = Helicopter ambulance 3 = Fixed-wing ambulance 4 = Private or public vehicle 5 = Walk-in 6 = Police 7 = Other 8 = Not transported 9 = Unknown |
Main type of transportation vehicle (if multiple chose vehicle used for the majority of the transportation phase) |
| Response time | Minutes | Time from Emergency Medical Communication Centre operator initiates transmission of dispatch message to first resource/unit time of arrival on scene of first unit as reported by first unit |
| Patient variables | ||
| Co-morbidity | 1 = No (ASA-PS = 1) 2 = Yes (ASA-PS = 2-6) 3 = Unknown |
ASA-PS definition 1 = A normal healthy patient 2 = A patient with mild systemic disease 3 = A patient with severe systemic disease 4 = A patient with severe systemic disease that is a constant threat to life 5 = A moribund patient who is not expected to survive without the operation 6 = A declared brain-dead patient whose organs are being removed for donor purposes |
| Age | Years or months | Years, if patient <2 years then months |
| Gender | 1 = Female 2 = Male 3 = Unknown |
Patients gender |
| Patient category | 1 = Blunt trauma (incl burns) 2 = Penetrating trauma 3 = Non-trauma (including drowning and asphyxia) 4 = Unknown |
Dominant reason for emergency treatment. |
| Indication for airway intervention | 1 = Decreased level of consciousness 2 = Hypoxemia 3 = Ineffective ventilation 4 = Existing airway obstruction 5 = Impending airway obstruction 6 = Combative or uncooperative 7 = Relief of pain or distress 8 = Cardiopulmonary arrest 9 = Other, specify |
Dominating indication for airway intervention |
| RR initial | Number/ Not recorded |
First value recorded by EMS provider on scene |
| SBP initial | Number/ Not recorded |
First value recorded by EMS provider on scene |
| HR initial | Number/ Not recorded |
First value recorded by EMS provider on scene |
| GCS initial (m/v/e) | Motor 1-6 Verbal 1-5 Eyes 1-4 Not recorded |
First value recorded by EMS provider on scene See also GCS definitions |
| SpO2 initial, state: with or without supplemental O2 | Number/ Not recorded 1 = Without supplemental O2 2 = With supplemental O2 3 = Unknown if supplemental O2 |
First value recorded by EMS provider on scene |
| Post-intervention variables | ||
| Post-intervention ventilation | 1 = Spontaneous 2 = Controlled 3 = Mixed 4 = Unknown |
How is patient ventilated following airway management? If both spontaneous and controlled choose mixed. |
| Post-intervention SBP | Number/ Not recorded |
First value recorded by EMS provider after finalised airway management |
| Post-intervention SpO2 | Number/ Not recorded |
First value recorded by EMS provider after finalised airway management |
| Post-intervention EtCO2 | Number/ Not recorded |
First value recorded by EMS provider after finalised airway management |
| Post-intervention SBP on arrival | Number/ Not recorded |
First value recorded by EMS provider after patient arrives at hospital |
| Post-intervention SpO2 on arrival | Number/ Not recorded |
First value recorded by EMS provider after patient arrives at hospital |
| Post-intervention EtCO2 on arrival | Number/ Not recorded |
First value recorded by EMS provider after patient arrives at hospital |
| Survival status | 1 = Dead on scene or on arrival 2 = Alive on arival 3 = Unknown |
Patient survival status: EMS treatment and on arrival hospital |
| Attempts at airway intervention | 1 = One attempt 2 = Multiple attempts 3 = Earlier attempts 4 = Unknown |
Number of attempts at securing the airway with extraglottic device or ETI. Earlier attempts describe the situation where another EMS personnel has attempted to secure the airway before the current. |
| Complications | 1 = ETT misplaced in oesophagus 2 = ETT misplaced in right mainstem bronchus 3 = Teeth trauma 4 = Vomiting and/or aspiration 5 = Hypoxia 6 = Bradycardia 7 = Hypotension 8 = Other, define 9 = None recorded |
Problems and mechanical complications recognized on scene and caused by airway management. Physiologic complications (5, 6 and 7) are regarded as such if they were not present before airway intervention and were recorded during or immediately after airway management. The following definitions are to be used: hypoxia: SpO2 <90% bradycardia: pulse rate <60 bpm hypotension: SBP <90 |
| Drugs used to facilitate airway procedure | 1 = Sedatives 2 = NMBA 3 = Analgetics/opioids 4 = Local/topic anaesthetic 5 = None |
Drugs used to facilitate the airway intervention. Select all that apply. |
| Intubation success | 1 = Success on first attempt 2 = Success after more than one attempt and one rescuer 3 = Success after more than one attempt and multiple rescuers 3 = Not successful |
Successful intubation defined as tube verified in the trachea. An intubation attempt is defined as attempted laryngoscopy with the intent to intubate |
| Device used in successful airway management | 1 = Bag Mask Ventilation 2 = SAD 3 = Oral TI 4 = Nasal TI 5 = Surgical airway 6 = None 7 = Unknown |
Device used to manage successful airway or device in place when patient is delivered at hospital/ED |
ASA-PS, American Society of Anesthesiologists physical status; bpm, beats per minute; BMV, bag mask ventilation; ED, emergency department; EMS, emergency medical service; EtCO2, end-tidal carbon dioxide; ETI, endotracheal intubation; ETT, endotracheal tube; GCS, Glasgow coma score; HR, heart rate; NMBA, neuromuscular blocking agent; P, paramedic; RR, respiratory rate; SAD, supraglottic airway device; SBP, systolic blood pressure; SpO2, saturation of peripheral oxygen, TI, tracheal intubation.
As identified by an international expert group [19].
Table 2.
Fixed system variables for uniform reporting of data from advanced airway management in the field, identified by an international expert group
| Data variable name | Data variable categories or values | Definition of data variable |
|---|---|---|
| Population | Number | Population count in the primary response area of the EMS |
| Area | Number | Area in square km or square miles of primary response area of the EMS |
| Rural, urban, split | 1 = Urban 2 = Rural 3 = Split |
Urban area defined as: "De facto population living in areas classified as urban according to the criteria used by each area or country. Data refer to 1 July of the year indicated and are presented in thousands" Rural area defined as: "De facto population living in areas classified as rural. Data refer to 1 July of the year indicated and are presented in thousands" |
| Usual tiered response | Free text | Describe briefly |
| Time intervals collected | Free text | Describe briefly |
| Mission type | Free text | Describe briefly; e.g. Mainly trauma or mixed patient population |
| Times available | Free text | Describe briefly |
| Established airway management protocols | Free text | Describe briefly |
| Airway management techniques available | Free text | Describe briefly |
| Describe type of training in airway management | Describe briefly | |
| Type of tracheal tube confirmation technique | 1 = Auscultation 2 = Colorimetry 3 = Capnometry 4 = Capnography 5 = None |
|
| Type of available ventilator | Free text | Describe briefly |
EMS, emergency medical service.
The aim of this study was to determine the rate of reported Utstein airway variables (28 core variables and 12 fixed-system variables) found in current scientific publications on pre-hospital TI [19].
Materials and methods
Study eligibility criteria
We included original English language articles pertaining to pre-hospital TI in adult patients. Studies that investigated pediatric cohorts and studies that focused on surgical airways were excluded. Studies that compared TI to other airway devices were also excluded.
Identification and selection of studies: data extraction
A systematic search of Medline and EMBASE databases according to the PRISMA guidelines to identify all relevant studies published prior to 1 September, 2009 was conducted (see Table 3 for search strategy) [20]. All records were converted into an EndNote bibliographic database (EndNote X1© Thompson Reuters, UK). Two reviewers (HML and MR) examined the titles and abstracts of the records for eligibility. The full texts of all potentially relevant studies were obtained, and two reviewers (HML and MR) assessed whether each study met the eligibility criteria. The reference lists of the included studies and a recent relevant Cochrane review were inspected to identify additional relevant studies [11].
Table 3.
Search strategy for identification of relevant studies in Medline and EMBASE
| Database | Search terms |
|---|---|
| "keywords" | |
| Medline | "emergency medical services" AND "intubation, intratracheal" |
| EMBASE | "emergency care" AND "intubation/or respiratory tract intubation" |
| "title" | |
| Medline | "prehospital" AND "intubation" |
| Medline | "pre-hospital" AND "intubation" |
| Medline | "out-of-hospital" AND "intubation" |
| Medline | "prehospital" AND "RSI" OR "rapid sequence induction" |
| Medline | "pre-hospital" AND "RSI" OR "rapid sequence induction" |
| Medline | "out-of-hospital" AND "RSI" OR "rapid sequence induction" |
| EMBASE | "prehospital" AND "intubation" |
| EMBASE | "pre-hospital" AND "intubation" |
| EMBASE | "out-of-hospital" AND "intubation" |
| EMBASE | "prehospital" AND "RSI" OR "rapid sequence induction" |
| EMBASE | "pre-hospital" AND "RSI" OR "rapid sequence induction" |
| EMBASE | "out-of-hospital" AND "RSI" OR "rapid sequence induction" |
Study characteristics
One reviewer (HML) used a standardised Excel spreadsheet (© 2007 Microsoft Corporation, USA) and extracted information from the included studies according to the newly published template for uniform reporting of data regarding advanced airway management in the field [19]. Reported variables that matched the Utstein variables were regarded as identical, although definitions sometimes differed or remained unreported.
The data were analysed using the Statistical Package for the Social Sciences, v. 18.0 (SPSS, Inc., Chicago, IL, USA), and the distributions were reported as medians and inter-quartile ranges (IQR). Being a systematic literature review, this study did not need approval from The Regional Committee for Research Ethics or the National Social Science Services.
Results
Literature search
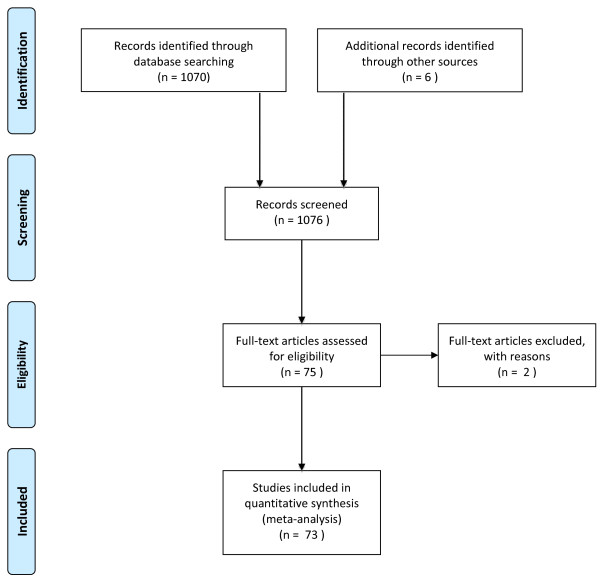
We identified 1,070 records in the initial search. Another six records were identified through other sources. Among these 1,076 records, 75 full-text original papers were assessed. Two of these were excluded from further analysis, one because of qualitative methodology and one being a preliminary report, leaving 73 studies for the final analysis (Figure 1).
Figure 1.
A search diagram according to the PRISMA statement.
Characteristics of the included studies
The majority of the studies (59, 81%) were from North American EMS systems. Of these, 46 (78%) described services in which non-physicians conducted TI. In contrast, 13 (87%) of the 15 non-North American EMS systems, physicians performed the pre-hospital TI. Of the 47 non-physician-manned systems, 25 (53%) performed drug-assisted TI.
Sixty-five studies had applied an observational methodology (89%), of which 29 were conducted prospectively and 36 retrospectively [see Additional data file 1]. We identified two randomised controlled trials (RCT) and six non-RCT interventional studies.
Core variables
None of the included studies presented the complete set of 28 variables recommended in the template [19]. The maximum number of core variables reported in a single study was 21. The minimum number reported was two, whereas the median number of core variables reported from all the studies was 10 (IQR 8 to 12).
The most frequent reported core variable was "patient category", reported in 63 (86%) of the 73 studies (Table 4). The least reported variable was "co-morbidity", reported in only 2 (3%) of 73 studies (Table 4).
Table 4.
Number of times (%) each Utstein variable was collected and documented among the 73 studies included
| Core variables | Number (%) |
|---|---|
| Core system variables | |
| Main type of transportation | 55 (75%) |
| Highest level of EMS provider on scene | 34 (47%) |
| Airway device available on scene | 26 (36%) |
| Drugs for airway management available on scene | 27 (37%) |
| Response time | 10 (14%) |
| Core patient variables | |
| Patient category | 63 (86%) |
| Age | 59 (81%) |
| Gender | 53 (73%) |
| GCS initial (m/v/e) | 40 (55%) |
| Systolic blood pressure, initial | 35 (48%) |
| Indication for airway intervention | 26 (36%) |
| Heart rate, initial | 13 (18%) |
| Respiratory rate, initial | 12 (16%) |
| SpO2 initial, state: with or without supplemental O2 | 11 (15%) |
| Co-morbidity | 2 (3%) |
| Post intervention variables | |
| Intubation success | 44 (60%) |
| Device used in successful airway management | 41 (56%) |
| Survival status | 40 (55%) |
| Complications | 30 (41%) |
| Drugs used to facilitate airway procedure | 28 (38%) |
| Attempts at airway intervention | 25 (34%) |
| Post-intervention SBP on arrival | 11 (15%) |
| Post-intervention SpO2 on arrival | 10 (14%) |
| Post-intervention EtCO2 on arrival | 8 (11%) |
| Post-intervention SBP | 8 (11%) |
| Post-intervention SpO2 | 8 (11%) |
| Post-intervention ventilation | 3 (4%) |
| Post-intervention EtCO2 | 3 (4%) |
| Fixed system variables | |
| Service mission types | 52 (71%) |
| Established airway management protocols | 48 (66%) |
| Area | 40 (55%) |
| Usual tiered response | 33 (45%) |
| Type of tracheal tube confirmation technique | 31 (42%) |
| Rural, urban, split | 31 (42%) |
| Airway management techniques available | 30 (41%) |
| Population | 24 (33%) |
| Describe type of training in airway management | 23 (32%) |
| Time intervals collected | 15 (21%) |
| Times available | 13 (18%) |
| Type of available ventilator | 1 (1%) |
EMS, emergency medical service; EtCO2, end-tidal carbon dioxide; GCS, Glasgow coma score, SBP, systolic blood pressure; SpO2, saturation of peripheral oxygen.
Fixed-system variables
Of the 12 fixed-system variables, the maximum number reported in a single study was 11. The median number reported was five (IQR four to eight), and two studies did not report any of the recommended fixed-system variables. The most frequently reported variable was "service mission type", which was reported in 52 (71%) of the 73 studies (Table 4). The least frequently reported fixed system variable was "type of available ventilator", which was only reported in one paper (1%) (Table 4).
All the studies included in the review are listed, and the number of matching core variables and fixed-system variables from each study are presented in Additional file 1.
Discussion
Our systematic literature review of studies pertaining to TI of adults revealed deficient reporting of the Utstein airway core variables as defined by an international expert group. Recommended core variables, such as "post-interventional end-tidal carbon dioxide (ETCO2)", "number of attempts at airway intervention" and "co-morbidity", which are all recognised as being highly associated with efficiency and outcome, were missing in the majority of the papers. Fixed-system variables were incompletely reported or absent in most of the included studies. The low number of reported core variables makes it difficult to compare different scientific reports, assess their validity, and extrapolate to other EMS systems. One could claim that several of the included studies with a low number of documented and reported core variables in fact only report the occurrence and performance of TI within their system and therefore are not reflective of the effects or efficiency of pre-hospital TI.
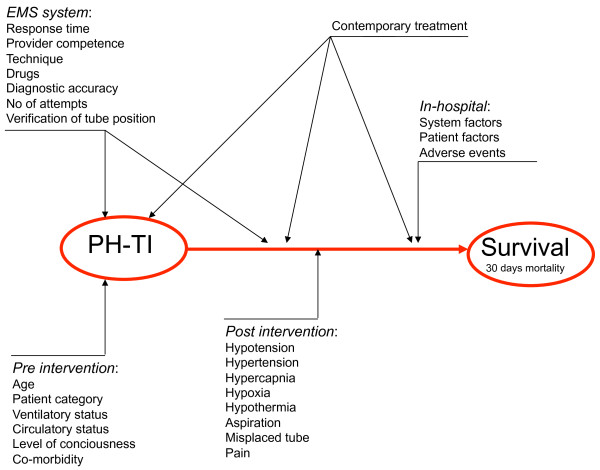
Several studies have focused on the intricacy of implementing TI in the pre-hospital setting [21-23]. TI represents a complex intervention (Figure 2) that contains several separate but highly interacting components. Scientific studies on this subject are difficult to design and interpret because of tremendous variability in (and insufficient description of) operator experience, technique, and patient case-mix, making it difficult to understand or eliminate confounding factors [24]. Furthermore, neither contemporary interventions nor pre-intervention, per-intervention, or post-intervention factors highly likely to influence outcome are usually documented, analysed, or adjusted for. Key in-hospital factors (likely to be concealed from the investigator) further confound the outcome analysis [25]. This finding may explain why apparently similar studies present conflicting results and reach opposite conclusions.
Figure 2.
A cause-effect chart and factors influencing the relation between PH-TI and survival.
RSI with oral intubation is the standard of care for drug-assisted emergency TI because it is widely recommended to be the safest way of performing this high-risk intervention [26-28]. However, only 19 (31%) of the 73 papers in this study reported the variable "drugs for airway management available on scene". Among papers that reported this variable, the definition and extent of drug assistance varied. Some services had protocols based on administering a muscle relaxant only; some combined this with a small dose of a sedative or analgesic, whereas some administered a traditional RSI. The presence or absence of drug assistance and the availability and dose of specific agents are likely to influence the success rate of TI and the rate and severity of adverse events. This information is essential to correctly assess the reported outcomes.
The majority of the included papers were based on observational studies, commonly referred to as low-quality evidence [29]. In a complex intervention, a true association between a single cause (TI) and an effect (survival) is difficult to prove (Figure 2). The presented results are flawed by multiple confounding factors, and external validity is questionable. Even randomization may fail to exclude the major confounders, a phenomenon demonstrated by Gausche et al. in one of the few randomized trials on pre-hospital TI [30]. The investigators reported no additional effect on survival or neurological outcome when paramedics performed pre-hospital TI compared with traditional bag/valve/mask ventilation in critically ill pediatric patients. The study set out to analyze the effect of the intervention itself, but due to an "intention-to-treat protocol", the intervention group was heavily confounded (abstained intubation, repetitive attempts of intubation, or failed intubation). The study instead demonstrates the effects of suboptimal provider competence and TI complications, and it illustrates the challenges of using traditional analytical techniques when assessing a complex intervention.
Several recent reviews have assessed the evidence of a pre-hospital TI effect [10,31], including a Cochrane review [11]. They consistently conclude that the available evidence is limited and weak. It has been suggested that the traditional method of systematic review is of limited use in the evaluation of a complex intervention [32]. The lack of a standard definition of pre-hospital TI poses a significant challenge for systematic reviewers and readers of these reviews. With respect to the Cochrane review on pre-hospital TI [11], the number of studies located in our review illustrates that any strict inclusion criteria for a systematic review will exclude the majority of studies published because pre-hospital TI is often performed differently or described inadequately. It also questions the whole evidence base on which current practice is based.
Limitations
We have assessed the included studies assuming that all the recommended Utstein airway core variables are important to document for each study. Some studies focus on particular aspects of pre-hospital TI intervention and may not need to report all the core variables from the template. Nonetheless, understanding the correlations between the intervention and its outcomes presupposes that all the interacting factors are accounted for.
The Utstein airway template still requires validation. Not all the variables relevant to outcome may have been identified. In a systematic review of studies on out-of-hospital cardiac arrest, a large variability in outcome not entirely explained by variability in documented Utstein variables, was found [33].
We also acknowledge that some relevant studies may not have been located during our database search. In the future, more homogenous reporting of studies pertaining to pre-hospital TI may reduce these limitations.
Conclusions
Our systematic literature review of studies investigating TI in adults demonstrated that core data required for proper interpretation of results were frequently not recorded and reported. The inconsistent and imprecise reporting of data may be the explanation for the fact that, despite numerous published studies on this subject, there is an ongoing debate on if, when, how, and by whom pre-hospital advanced airway management should be performed. Pre-hospital TI is a complex intervention, and terminology and study design must be improved to substantiate future evidence-based clinical practice. To support this, there is a significant need for an international standard for documenting and reporting pre-hospital TI in severely ill and injured patients. The newly published template might be a first and important step in this direction [19].
Key messages
• Studies investigating pre-hospital TI in adults lack the core data required for useful interpretation of results.
• The published studies investigating pre-hospital TI rarely present high-quality scientific evidence.
• Pre-hospital TI is a complex intervention, and terminology and study design must be developed to substantiate future evidence-based clinical practice.
• A recently published template for reporting advanced pre-hospital airway management might be a first and important step in this direction.
Abbreviations
EMS: emergency medical services; ETCO2: end-tidal carbon dioxide; IQR: interquartile range; RCT: randomized controlled trial; RSI: rapid sequence intubation; TI: tracheal intubation.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
HML, SJMS and DJL developed the protocol. MR and HML conducted the systematic review. HML performed the analysis and drafted the manuscript. All authors read and approved the final manuscript.
Supplementary Material
Overview of included studies. Aim of study, study design, TI provider, continent, number of the 28 Utstein core and 12 Utstein fixed system variables (%) reported in the 73 reviewed studies.
Please see related commentary by Davis, http://ccforum.com/content/15/2/133
Contributor Information
Hans Morten Lossius, Email: hans.morten.lossius@snla.no.
Stephen JM Sollid, Email: Stephen.Sollid@snla.no.
Marius Rehn, Email: marius.rehn@snla.no.
David J Lockey, Email: David.Lockey@nbt.nhs.uk.
References
- Hubble MW, Brown L, Wilfong DA, Hertelendy A, Benner RW, Richards ME. A meta-analysis of prehospital airway control techniques part I: orotracheal and nasotracheal intubation success rates. Prehosp Emerg Care. 2010;14:377–401. doi: 10.3109/10903121003790173. [DOI] [PubMed] [Google Scholar]
- Lockey D, Davies G, Coats T. Survival of trauma patients who have prehospital tracheal intubation without anaesthesia or muscle relaxants: observational study. BMJ. 2001;323:141. doi: 10.1136/bmj.323.7305.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang HE, Cook LJ, Chang CC, Yealy DM, Lave JR. Outcomes after out-of-hospital endotracheal intubation errors. Resuscitation. 2009;80:50–55. doi: 10.1016/j.resuscitation.2008.08.016. [DOI] [PubMed] [Google Scholar]
- Bochicchio GV, Scalea TM. Is field intubation useful? Curr Opin Crit Care. 2003;9:524–529. doi: 10.1097/00075198-200312000-00010. [DOI] [PubMed] [Google Scholar]
- Warner KJ, Sharar SR, Copass MK, Bulger EM. Prehospital management of the difficult airway: a prospective cohort study. J Emerg Med. 2009;36:257–265. doi: 10.1016/j.jemermed.2007.10.058. [DOI] [PubMed] [Google Scholar]
- Davis DP. Early ventilation in traumatic brain injury. Resuscitation. 2008;76:333–340. doi: 10.1016/j.resuscitation.2007.08.004. [DOI] [PubMed] [Google Scholar]
- Helm M, Hauke J, Lampl L. A prospective study of the quality of pre-hospital emergency ventilation in patients with severe head injury. Br J Anaesth. 2002;88:345–349. doi: 10.1093/bja/88.3.345. [DOI] [PubMed] [Google Scholar]
- Shafi S, Gentilello L. Pre-hospital endotracheal intubation and positive pressure ventilation is associated with hypotension and decreased survival in hypovolemic trauma patients: an analysis of the National Trauma Data Bank. J Trauma. 2005;59:1140–1145. doi: 10.1097/01.ta.0000196434.88182.77. [DOI] [PubMed] [Google Scholar]
- Di Bartolomeo S, Sanson G, Nardi G, Michelutto V, Scian F. Inadequate ventilation of patients with severe brain injury: a possible drawback to prehospital advanced trauma care? Eur J Emerg Med. 2003;10:268–271. doi: 10.1097/00063110-200312000-00005. [DOI] [PubMed] [Google Scholar]
- von Elm E, Schoettker P, Henzi I, Osterwalder J, Walder B. Pre-hospital tracheal intubation in patients with traumatic brain injury: systematic review of current evidence. Br J Anaesth. 2009;103:371–386. doi: 10.1093/bja/aep202. [DOI] [PubMed] [Google Scholar]
- Lecky F, Bryden D, Little R, Tong N, Moulton C. Emergency intubation for acutely ill and injured patients. Cochrane Database Syst Rev. 2008. p. CD001429. [DOI] [PMC free article] [PubMed]
- Dunham CM, Barraco RD, Clark DE, Daley BJ, Davis FE, Gibbs MA, Knuth T, Letarte PB, Luchette FA, Omert L, Weireter LJ, Wiles CE. EAST Practice Management Guidelines Work Group. Guidelines for emergency tracheal intubation immediately after traumatic injury. J Trauma. 2003;55:162–179. doi: 10.1097/01.ta.0000083335.93868.2c. [DOI] [PubMed] [Google Scholar]
- Garza AG, Gratton MC, McElroy J, Lindholm D, Coontz D. Environmental factors encountered during out-of-hospital intubation attempts. Prehosp Emerg Care. 2008;12:286–289. doi: 10.1080/10903120802100480. [DOI] [PubMed] [Google Scholar]
- Huter L, Schreiber T, Reichel J, Schwarzkopf K. Present-day prehospital airway management in the former Eastern German state of Thuringia: equipment and education of emergency physicians. Eur J Emerg Med. 2009;16:97–99. doi: 10.1097/MEJ.0b013e32830a7577. [DOI] [PubMed] [Google Scholar]
- Ridgway S, Hodzovic I, Woollard M, Latto IP. Prehospital airway management in Ambulance Services in the United Kingdom. Anaesthesia. 2004;59:1091–1094. doi: 10.1111/j.1365-2044.2004.03965.x. [DOI] [PubMed] [Google Scholar]
- Timmermann A, Russo SG, Hollmann MW. Paramedic versus emergency physician emergency medical service: role of the anaesthesiologist and the European versus the Anglo-American concept. Curr Opin Anaesthesiol. 2008;21:222–227. doi: 10.1097/ACO.0b013e3282f5f4f7. [DOI] [PubMed] [Google Scholar]
- Jeremie N, Seltzer S, Lenfant F, Ricard-Hibon A, Facon A, Cabrita B, Messant I, d'Athis P, Freysz M. Rapid sequence induction: a survey of practices in three French prehospital mobile emergency units. Eur J Emerg Med. 2006;13:148–155. doi: 10.1097/01.mej.0000209052.85881.e2. [DOI] [PubMed] [Google Scholar]
- Garza AG, Algren DA, Gratton MC, Ma OJ. Populations at risk for intubation nonattempt and failure in the prehospital setting. Prehosp Emerg Care. 2005;9:163–166. doi: 10.1080/10903120590924654. [DOI] [PubMed] [Google Scholar]
- Sollid SJ, Lockey D, Lossius HM. A consensus-based template for uniform reporting of data from pre-hospital advanced airway management. Scand J Trauma Resusc Emerg Med. 2009;17:58. doi: 10.1186/1757-7241-17-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JB, Abo BN, Wang HE. Paramedic perceptions of challenges in out-of-hospital endotracheal intubation. Prehosp Emerg Care. 2007;11:219–223. doi: 10.1080/10903120701205802. [DOI] [PubMed] [Google Scholar]
- Wang HE, Abo BN, Lave JR, Yealy DM. How would minimum experience standards affect the distribution of out-of-hospital endotracheal intubations? Ann Emerg Med. 2007;50:246–252. doi: 10.1016/j.annemergmed.2007.04.023. [DOI] [PubMed] [Google Scholar]
- Ummenhofer W, Scheidegger D. Role of the physician in prehospital management of trauma: European perspective. Curr Opin Crit Care. 2002;8:559–565. doi: 10.1097/00075198-200212000-00013. [DOI] [PubMed] [Google Scholar]
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langhelle A, Tyvold SS, Lexow K, Hapnes SA, Sunde K, Steen PA. In-hospital factors associated with improved outcome after out-of-hospital cardiac arrest. A comparison between four regions in Norway. Resuscitation. 2003;56:247–263. doi: 10.1016/S0300-9572(02)00409-4. [DOI] [PubMed] [Google Scholar]
- Dunham CM, Barraco RD, Clark DE, Daley BJ, Davis FE, Gibbs MA, Knuth T, Letarte PB, Luchette FA, Omert L, Weireter LJ, Wiles CE. EAST Practice Management Guidelines Work Group. Guidelines for emergency tracheal intubation immediately after traumatic injury. J Trauma. 2003;55:162–179. doi: 10.1097/01.ta.0000083335.93868.2c. [DOI] [PubMed] [Google Scholar]
- The Association of Anaesthetists of Great Britain and Ireland. AAGBI safety guideline: Pre-hospital Anaesthesia. London: AAGBI; 2009. [Google Scholar]
- Berlac P, Hyldmo PK, Kongstad P, Kurola J, Nakstad AR, Sandberg M. Pre-hospital airway management: guidelines from a task force from the Scandinavian Society for Anaesthesiology and Intensive Care Medicine. Acta Anaesthesiol Scand. 2008;7:897–907. doi: 10.1111/j.1399-6576.2008.01673.x. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gausche M, Lewis RJ, Stratton SJ, Haynes BE, Gunter CS, Goodrich SM, Poore PD, McCollough MD, Henderson DP, Pratt FD, Seidel JS. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. JAMA. 2000;283:783–790. doi: 10.1001/jama.283.6.783. [DOI] [PubMed] [Google Scholar]
- Davis DP. Prehospital intubation of brain-injured patients. Curr Opin Crit Care. 2008;14:142–148. doi: 10.1097/MCC.0b013e3282f63c40. [DOI] [PubMed] [Google Scholar]
- Shepperd S, Lewin S, Straus S, Haynes BE, Gunter CS, Goodrich SM, Poore PD, McCollough MD, Henderson DP, Pratt FD, Seidel JS. Can we systematically review studies that evaluate complex interventions? PLoS Med. 2009;6:e1000086. doi: 10.1371/journal.pmed.1000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksson M, Herlitz J, Nichol G. Variation in outcome in studies of out-of-hospital cardiac arrest: a review of studies conforming to the Utstein guidelines. Am J Emerg Med. 2003;21:276–281. doi: 10.1016/S0735-6757(03)00082-2. [DOI] [PubMed] [Google Scholar]
- Adams BD, Cuniowski PA, Muck A, De Lorenzo RA. Registry of emergency airways arriving at combat hospitals. J Trauma. 2008;64:1548–1554. doi: 10.1097/TA.0b013e3181728c41. [DOI] [PubMed] [Google Scholar]
- Adnet F, Jouriles NJ, Le Toumelin P, Hennequin B, Taillandier C, Rayeh F, Couvreur J, Nougiere B, Nadiras P, Ladka A, Fleury M. Survey of out-of-hospital emergency intubations in the French prehospital medical system: a multicenter study. Ann Emerg Med. 1998;32:454–460. doi: 10.1016/S0196-0644(98)70175-1. [DOI] [PubMed] [Google Scholar]
- Arbabi S, Jurkovich GJ, Wahl WL, Franklin GA, Hemmila MR, Taheri PA, Maier RV. A comparison of prehospital and hospital data in trauma patients. J Trauma. 2004;56:1029–1032. doi: 10.1097/01.TA.0000123036.20919.4B. [DOI] [PubMed] [Google Scholar]
- Bair AE, Smith D, Lichty L. Intubation confirmation techniques associated with unrecognized non-tracheal intubations by pre-hospital providers. J Emerg Med. 2005;28:403–407. doi: 10.1016/j.jemermed.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Bochicchio GV, Ilahi O, Joshi M, Bochicchio K, Scalea TM. Endotracheal intubation in the field does not improve outcome in trauma patients who present without an acutely lethal traumatic brain injury. J Trauma. 2003;54:307–311. doi: 10.1097/01.TA.0000046252.97590.BE. [DOI] [PubMed] [Google Scholar]
- Bozeman WP, Kleiner DM, Huggett V. A comparison of rapid-sequence intubation and etomidate-only intubation in the prehospital air medical setting. Prehosp Emerg Care. 2006;10:8–13. doi: 10.1080/10903120500366854. [DOI] [PubMed] [Google Scholar]
- Bradley JS, Billows GL, Olinger ML, Boha SP, Cordell WH, Nelson DR. Prehospital oral endotracheal intubation by rural basic emergency medical technicians. Ann Emerg Med. 1998;32:26–32. doi: 10.1016/S0196-0644(98)70095-2. [DOI] [PubMed] [Google Scholar]
- Bulger EM, Copass MK, Sabath DR, Maier RV, Jurkovich GJ. The use of neuromuscular blocking agents to facilitate prehospital intubation does not impair outcome after traumatic brain injury. J Trauma. 2005;58:718–723. doi: 10.1097/01.TA.0000159239.14181.BC. [DOI] [PubMed] [Google Scholar]
- Bushby N, Fitzgerald M, Cameron P, Marasco S, Bystrzycki A, Rosenfeld JV, Bailey M. Prehospital intubation and chest decompression is associated with unexpected survival in major thoracic blunt trauma. Emerg Med Australas. 2005;17:443–449. doi: 10.1111/j.1742-6723.2005.00775.x. [DOI] [PubMed] [Google Scholar]
- Cantineau JP, Tazarourte K, Merckx P, Martin L, Reynaud P, Berson C, Bertrand C, Aussavy F, Lepresle E, Pentier C, Duvaldestin P. Tracheal intubation in prehospital resuscitation: importance of rapid-sequence induction anesthesia. Ann Fr Anesth Reanim. 1997;16:878–884. doi: 10.1016/S0750-7658(97)89837-1. [DOI] [PubMed] [Google Scholar]
- Christensen EF, Hoyer CC. Prehospital tracheal intubation in severely injured patients: a Danish observational study. BMJ. 2003;327:533–534. doi: 10.1136/bmj.327.7414.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobas MA, De la Pena MA, Manning R, Candiotti K, Varon AJ. Prehospital intubations and mortality: a level 1 trauma center perspective. Anesthesia & Analgesia. 2009;109:489–493. doi: 10.1213/ane.0b013e3181aa3063. [DOI] [PubMed] [Google Scholar]
- Colwell CB, McVaney KE, Haukoos JS, Wiebe DP, Gravitz CS, Dunn WW, Bryan T. An evaluation of out-of-hospital advanced airway management in an urban setting. Acad Emerg Med. 2005;12:417–422. doi: 10.1111/j.1553-2712.2005.tb01542.x. [DOI] [PubMed] [Google Scholar]
- Cudnik MT, Newgard CD, Wang H, Bangs C, Herrington RT. Distance impacts mortality in trauma patients with an intubation attempt. Prehosp Emerg Care. 2008;12:459–466. doi: 10.1080/10903120802290745. [DOI] [PubMed] [Google Scholar]
- Cudnik MT, Newgard CD, Wang H, Bangs C, Herrington RT. Endotracheal intubation increases out-of-hospital time in trauma patients. Prehosp Emerg Care. 2007;11:224–229. doi: 10.1080/10903120701205208. [DOI] [PubMed] [Google Scholar]
- Davis DP, Ochs M, Hoyt DB, Bailey D, Marshall LK, Rosen P. Paramedic-administered neuromuscular blockade improves prehospital intubation success in severely head-injured patients. J Trauma. 2003;55:713–719. doi: 10.1097/01.TA.0000037428.65987.12. [DOI] [PubMed] [Google Scholar]
- Davis DP, Hoyt DB, Ochs M, Fortlage D, Holbrook T, Marshall LK, Rosen P. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J Trauma. 2003;54:444–453. doi: 10.1097/01.TA.0000053396.02126.CD. [DOI] [PubMed] [Google Scholar]
- Davis DP, Vadeboncoeur TF, Ochs M, Poste JC, Vilke GM, Hoyt DB. The association between field Glasgow Coma Scale score and outcome in patients undergoing paramedic rapid sequence intubation. J Emerg Med. 2005;29:391–397. doi: 10.1016/j.jemermed.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Davis DP, Peay J, Sise MJ, Vilke GM, Kennedy F, Eastman AB, Velky T, Hoyt DB. The impact of prehospital endotracheal intubation on outcome in moderate to severe traumatic brain injury. J Trauma. 2005;58:933–939. doi: 10.1097/01.TA.0000162731.53812.58. [DOI] [PubMed] [Google Scholar]
- Davis DP, Fisher R, Buono C, Brainard C, Smith S, Ochs G, Poste JC, Dunford JV. Predictors of intubation success and therapeutic value of paramedic airway management in a large, urban EMS system. Prehosp Emerg Care. 2006;10:356–362. doi: 10.1080/10903120600725751. [DOI] [PubMed] [Google Scholar]
- Davis DP, Hwang JQ, Dunford JV. Rate of decline in oxygen saturation at various pulse oximetry values with prehospital rapid sequence intubation. Prehosp Emerg Care. 2008;12:46–51. doi: 10.1080/10903120701710470. [DOI] [PubMed] [Google Scholar]
- Denver MASG. A prospective multicenter evaluation of prehospital airway management performance in a large metropolitan region. Prehosp Emerg Care. 2009;13:304–310. doi: 10.1080/10903120902935280. [DOI] [PubMed] [Google Scholar]
- Eckstein M, Chan L, Schneir A, Palmer R. Effect of prehospital advanced life support on outcomes of major trauma patients. J Trauma. 2000;48:643–648. doi: 10.1097/00005373-200004000-00010. [DOI] [PubMed] [Google Scholar]
- Ellis DY, Davies GE, Pearn J, Lockey D. Prehospital rapid-sequence intubation of patients with trauma with a Glasgow Coma Score of 13 or 14 and the subsequent incidence of intracranial pathology. Emerg Med J. 2007;24:139–141. doi: 10.1136/emj.2006.040428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fakhry SM, Scanlon JM, Robinson L, Askari R, Watenpaugh RL, Fata P, Hauda WE, Trask A. Prehospital rapid sequence intubation for head trauma: conditions for a successful program. J Trauma. 2006;60:997–1001. doi: 10.1097/01.ta.0000217285.94057.5e. [DOI] [PubMed] [Google Scholar]
- Frankel H, Rozycki G, Champion H, Harviel JD, Bass R. The use of TRISS methodology to validate prehospital intubation by urban EMS providers. Am J Emerg Med. 1997;15:630–632. doi: 10.1016/S0735-6757(97)90174-1. [DOI] [PubMed] [Google Scholar]
- Gunning M, O'Loughlin E, Fletcher M, Crilly J, Hooper M, Ellis DY. Emergency intubation: a prospective multicentre descriptive audit in an Australian helicopter emergency medical service. Emerg Med J. 2009;26:65–69. doi: 10.1136/emj.2008.059345. [DOI] [PubMed] [Google Scholar]
- Jacoby J, Heller M, Nicholas J, Patel N, Cesta M, Smith G, Jacob S, Reed J. Etomidate versus midazolam for out-of-hospital intubation: a prospective, randomized trial. Ann Emerg Med. 2006;47:525–530. doi: 10.1016/j.annemergmed.2005.12.009. [DOI] [PubMed] [Google Scholar]
- Jemmett ME, Kendal KM, Fourre MW, Burton JH. Unrecognized misplacement of endotracheal tubes in a mixed urban to rural emergency medical services setting. Acad Emerg Med. 2003;10:961–965. doi: 10.1111/j.1553-2712.2003.tb00652.x. [DOI] [PubMed] [Google Scholar]
- Jones JH, Murphy MP, Dickson RL, Somerville GG, Brizendine EJ. Emergency physician-verified out-of-hospital intubation: miss rates by paramedics. Acad Emerg Med. 2004;11:707–709. doi: 10.1197/j.aem.2003.12.026. [DOI] [PubMed] [Google Scholar]
- Karch SB, Lewis T, Young S, Hales D, Ho CH. Field intubation of trauma patients: complications, indications, and outcomes. Am J Emerg Med. 1996;14:617–619. doi: 10.1016/S0735-6757(96)90073-X. [DOI] [PubMed] [Google Scholar]
- Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37:32–37. doi: 10.1067/mem.2001.112098. [DOI] [PubMed] [Google Scholar]
- Klemen P, Grmec S. Effect of pre-hospital advanced life support with rapid sequence intubation on outcome of severe traumatic brain injury. Acta Anaesthesiol Scand. 2006;50:1250–1254. doi: 10.1111/j.1399-6576.2006.01039.x. [DOI] [PubMed] [Google Scholar]
- Mackay CA, Terris J, Coats TJ. Prehospital rapid sequence induction by emergency physicians: is it safe? Emerg Med J. 2001;18:20–24. doi: 10.1136/emj.18.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntosh SE, Swanson ER, McKeone A, Barton ED. Location of airway management in air medical transport. Prehosp Emerg Care. 2008;12:438–442. doi: 10.1080/10903120802301518. [DOI] [PubMed] [Google Scholar]
- Murray JA, Demetriades D, Berne TV, Stratton SJ, Cryer HG, Bongard F, Fleming A, Gaspard D. Prehospital intubation in patients with severe head injury. J Trauma. 2000;49:1065–1070. doi: 10.1097/00005373-200012000-00015. [DOI] [PubMed] [Google Scholar]
- Newton A, Ratchford A, Khan I. Incidence of adverse events during prehospital rapid sequence intubation: a review of one year on the London Helicopter Emergency Medical Service. J Trauma. 2008;64:487–492. doi: 10.1097/TA.0b013e31802e7476. [DOI] [PubMed] [Google Scholar]
- Ochs M, Davis D, Hoyt D, Bailey D, Marshall L, Rosen P. Paramedic-performed rapid sequence intubation of patients with severe head injuries. Ann Emerg Med. 2002;40:159–167. doi: 10.1067/mem.2002.126397. [DOI] [PubMed] [Google Scholar]
- Oswalt JL, Hedges JR, Soifer BE, Lowe DK. Analysis of trauma intubations. Am J Emerg Med. 1992;10:511–514. doi: 10.1016/0735-6757(92)90173-U. [DOI] [PubMed] [Google Scholar]
- Poste JC, Davis DP, Ochs M, Vilke GM, Castillo EM, Stern J, Hoyt DB. Air medical transport of severely head-injured patients undergoing paramedic rapid sequence intubation. Air Med J. 2004;23:36–40. doi: 10.1016/j.amj.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Rhee KJ, O'Malley RJ. Neuromuscular blockade-assisted oral intubation versus nasotracheal intubation in the prehospital care of injured patients. Ann Emerg Med. 1994;23:37–42. doi: 10.1016/S0196-0644(94)70005-2. [DOI] [PubMed] [Google Scholar]
- Ruchholtz S, Waydhas C, Ose C, Lewan U, Nast-Kolb D. Prehospital intubation in severe thoracic trauma without respiratory insufficiency: a matched-pair analysis based on the Trauma Registry of the German Trauma Society. J Trauma. 2002;52:879–886. doi: 10.1097/00005373-200205000-00010. [DOI] [PubMed] [Google Scholar]
- Sing RF, Rotondo MF, Zonies DH, Schwab CW, Kauder DR, Ross SE, Brathwaite CC. Rapid sequence induction for intubation by an aeromedical transport team: a critical analysis. Am J Emerg Med. 1998;16:598–602. doi: 10.1016/S0735-6757(98)90227-3. [DOI] [PubMed] [Google Scholar]
- Slagt C, Zondervan A, Patka P, de Lange JJ. A retrospective analysis of the intubations performed during 5 years of helicopter emergency medical service in Amsterdam. Air Med J. 2004;23:36–37. doi: 10.1016/j.amj.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Sloane C, Vilke GM, Chan TC, Hayden SR, Hoyt DB, Rosen P. Rapid sequence intubation in the field versus hospital in trauma patients. J Emerg Med. 2000;19:259–264. doi: 10.1016/S0736-4679(00)00235-3. [DOI] [PubMed] [Google Scholar]
- Stiell IG, Nesbitt LP, Pickett W, Munkley D, Spaite DW, Banek J, Field B, Luinstra-Toohey L, Maloney J, Dreyer J, Lyver M, Campeau T, Wells GA, Group OS. The OPALS Major Trauma Study: impact of advanced life-support on survival and morbidity. CMAJ. 2008;178:1141–1152. doi: 10.1503/cmaj.071154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonday CJ, Axelband J, Jacoby J, Higgins R, Crider D. Thiopental vs. etomidate for rapid sequence intubation in aeromedicine. Prehosp Disaster Med. 2005;20:324–326. doi: 10.1017/s1049023x00002788. [DOI] [PubMed] [Google Scholar]
- Stockinger ZT, McSwain NE Jr. Prehospital endotracheal intubation for trauma does not improve survival over bag-valve-mask ventilation. J Trauma. 2004;56:531–536. doi: 10.1097/01.TA.0000111755.94642.29. [DOI] [PubMed] [Google Scholar]
- Swanson ER, Fosnocht DE, Neff RJ. The use of etomidate for rapid-sequence intubation in the air medical setting. Prehosp Emerg Care. 2001;5:142–146. doi: 10.1080/10903120190940001. [DOI] [PubMed] [Google Scholar]
- Swanson ER, Fosnocht DE. Effect of an airway education program on prehospital intubation. Air Med J. 2002;21:28–31. doi: 10.1016/S1067-991X(02)70054-0. [DOI] [PubMed] [Google Scholar]
- Swanson ER, Fosnocht DE, Jensen SC. Comparison of etomidate and midazolam for prehospital rapid-sequence intubation. Prehosp Emerg Care. 2004;8:273–279. doi: 10.1016/j.prehos.2003.12.026. [DOI] [PubMed] [Google Scholar]
- Tam RK, Maloney J, Gaboury I, Verdon JM, Trickett J, Leduc SD, Poirier P. Review of endotracheal intubations by Ottawa advanced care paramedics in Canada. Prehosp Emerg Care. 2009;13:311–315. doi: 10.1080/10903120902935231. [DOI] [PubMed] [Google Scholar]
- Timmermann A, Russo SG, Eich C, Roessler M, Braun U, Rosenblatt WH, Quintel M. The out-of-hospital esophageal and endobronchial intubations performed by emergency physicians. Anesth Analg. 2007;104:619–623. doi: 10.1213/01.ane.0000253523.80050.e9. [DOI] [PubMed] [Google Scholar]
- Tracy S, Schinco MA, Griffen MM, Kerwin AJ, Devin T, Tepas JJ. Urgent airway intervention: does outcome change with personnel performing the procedure? J Trauma. 2006;61:1162–1165. doi: 10.1097/01.ta.0000243887.90697.06. [DOI] [PubMed] [Google Scholar]
- Ufberg JW, Bushra JS, Karras DJ, Satz WA, Kueppers F. Aspiration of gastric contents: association with prehospital intubation. Am J Emerg Med. 2005;23:379–382. doi: 10.1016/j.ajem.2005.02.005. [DOI] [PubMed] [Google Scholar]
- Vadeboncoeur TF, Davis DP, Ochs M, Poste JC, Hoyt DB, Vilke GM. The ability of paramedics to predict aspiration in patients undergoing prehospital rapid sequence intubation. J Emerg Med. 2006;30:131–136. doi: 10.1016/j.jemermed.2005.04.019. [DOI] [PubMed] [Google Scholar]
- Wang HE, O'Connor RE, Schnyder ME, Barnes TA, Megargel RE. Patient status and time to intubation in the assessment of prehospital intubation performance. Prehosp Emerg Care. 2001;5:10–18. doi: 10.1080/10903120190940254. [DOI] [PubMed] [Google Scholar]
- Wang HE, Sweeney TA, O'Connor RE, Rubinstein H. Failed prehospital intubations: an analysis of emergency department courses and outcomes. Prehosp Emerg Care. 2001;5:134–141. doi: 10.1080/10903120190939995. [DOI] [PubMed] [Google Scholar]
- Wang HE, Kupas DF, Paris PM, Bates RR, Costantino JP, Yealy DM. Multivariate predictors of failed prehospital endotracheal intubation. Acad Emerg Med. 2003;10:717–724. doi: 10.1111/j.1553-2712.2003.tb00065.x. [DOI] [PubMed] [Google Scholar]
- Wang HE, Kupas DF, Paris PM, Yealy DM. Factors associated with the use of pharmacologic agents to facilitate out-of-hospital endotracheal intubation. Prehosp Emerg Care. 2004;8:1–9. doi: 10.1080/312703002740. [DOI] [PubMed] [Google Scholar]
- Wang HE, Peitzman AB, Cassidy LD, Adelson PD, Yealy DM. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004;44:439–450. doi: 10.1016/j.annemergmed.2004.04.008. [DOI] [PubMed] [Google Scholar]
- Wang HE, Yealy DM. How many attempts are required to accomplish out-of-hospital endotracheal intubation? Acad Emerg Med. 2006;13:372–377. doi: 10.1111/j.1553-2712.2006.tb00311.x. [DOI] [PubMed] [Google Scholar]
- Wang HE, Lave JR, Sirio CA, Yealy DM. Paramedic intubation errors: isolated events or symptoms of larger problems? Health Affairs. 2006;25:501–509. doi: 10.1377/hlthaff.25.2.501. [DOI] [PubMed] [Google Scholar]
- Warner KJ, Cuschieri J, Copass MK, Jurkovich GJ, Bulger EM. The impact of prehospital ventilation on outcome after severe traumatic brain injury. J Trauma. 2007;62:1330–1336. doi: 10.1097/TA.0b013e31804a8032. discussion 1336-1338. [DOI] [PubMed] [Google Scholar]
- Wayne MA, Friedland E. Prehospital use of succinylcholine: a 20-year review. Prehosp Emerg Care. 1999;3:107–109. doi: 10.1080/10903129908958916. [DOI] [PubMed] [Google Scholar]
- Winchell RJ, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury. Trauma Research and Education Foundation of San Diego. Arch Surg. 1997;132:592–597. doi: 10.1001/archsurg.1997.01430300034007. [DOI] [PubMed] [Google Scholar]
- Wirtz DD, Ortiz C, Newman DH, Zhitomirsky I. Unrecognized misplacement of endotracheal tubes by ground prehospital providers. Prehosp Emerg Care. 2007;11:213–218. doi: 10.1080/10903120701205935. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Overview of included studies. Aim of study, study design, TI provider, continent, number of the 28 Utstein core and 12 Utstein fixed system variables (%) reported in the 73 reviewed studies.