Abstract
A patient diagnosed with early squamous-cell carcinoma (SCC) with microinvasion was treated by surgical excision followed by histopathologic evaluation. During surgery, all the nodes appeared free of tumor other than a single level-3 node which looked suspicious and enlarged. Surprisingly, the node, instead of showing SCC showed features suggestive of “etastatic papillary thyroid carcinoma.” The characteristics of papillary thyroid carcinoma (PTC), their usual histopathologic features and treatment are discussed. The aim of this paper is to present the case of a patient with dual malignancy—oral SCC and PTC in an adult male, which was diagnosed accidently because the protocol of complete surgery and extensive sampling for pathologic examination was followed and thus emphasizes on the necessity for the same.
Keywords: Extensive sampling, papillary thyroid carcinoma, thyroid carcinoma
INTRODUCTION
Usually after the diagnosis, treatment plan is made and the patient is operated according to the surgery planned. But it is important that surgeon should not stick strictly to the planned surgery, rather should believe more on his instincts and surgical/clinical acumen and should alter the surgery if required at all. Similarly the pathologists should never only examine the main lesional specimen; rather a complete extensive sampling and examination of all the tissues bits sent should be done to come to a final diagnosis. Herein we report a case which emphasizes the importance of this. The aim of this paper is to describe the case of a patient with oral SCC in whom one of the involved nodes showed the features of PTC instead of SCC.
Thyroid cancers are quite rare, and they occur more frequently in middle aged women. The thyroid carcinomas are primarily of papillary, follicular, medullary and anaplastic types.[1] During the last few years, the frequency of papillary cancer has increased.[2] The characteristics of papillary thyroid carcinoma (PTC), investigations, histopathologic features and treatment are discussed. The thyroid cancers are typically treated with complete removal of the lobe of the thyroid that harbors the cancer, in addition to the removal of most or all of the other side.[3]
CASE REPORT
A 17-year-old male patient with a 6-year history of tobacco/gutkha chewing and 3-year history of smoking reported to the outpatient department of Banaras Hindu University (BHU), Varanasi, with a nonhealing ulcerated lesion of 8-month duration on the lower left gingiva. Patient took some medication for ulcer during this period, which could not provide him relief for the same. There was a history of slight weight loss during this period. Nothing significant was reported in medical history. Family history was also not relevant.
Clinically, intraoral examination revealed an ulceroproliferative fixed growth of size 1.0 × 1.5 cm on left mandibular gingiva in canine-premolar region. There was presence of abundant deposits on left upper and lower posterior teeth suggestive of unilateral masticatory habit on right side.
Extraoral examination revealed that the mouth opening was normal—about 40 mm and there was foul smell from mouth. There was smooth and coordinated movement of temporomandibular joint (TMJ) with no palpable lymph nodes.
Routine blood investigations were performed which were within normal limits and the enzyme-linked immunosorbent assay (ELISA) test for human immunodeficiency virus (HIV) was negative. The lesion was subjected for histopathological examination by incisional biopsy and was diagnosed as early SCC with microinvasion. The patient underwent wide excision and supraomohyoid neck dissection. The patient was advised chemotherapy which he refused due to monetary reasons. The patient was finally lost for follow-up.
The excised tissue bits were sent for further histopathologic evaluation. The hematoxylin and eosin sections from the lesion revealed ulcerated parakeratinized stratified squamous epithelium with epithelial proliferation noted at the margin of ulcer [Figure 1]. The dysplastic epithelium showed features like increased nuclear-cytoplasmic ratio, nuclear hyperchromatism, pleomorphism, individual cell keratinization, and few atypical mitotic figures. A few dysplastic squamous cells were found infiltrating the underlying connective tissue. The underlying connective tissue showed moderately dense amount of chronic inflammatory cell infiltrate. All these features confirmed the diagnosis of early SCC with microinvasion.
Figure 1.
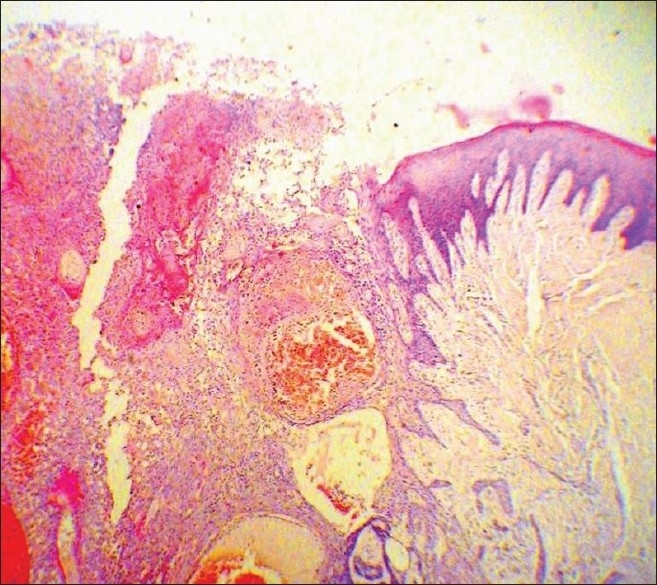
Dysplastic epithelial proliferation at the margin of ulcer (H and E stain, 100×)
The level-1, level-2, and all, except a single level-3 node, were free of tumor. A single level-3 node looked suspicious and enlarged. Grossly, the involved node was large in size and appeared blackish from outside. The longitudinal section (L.S.) of node revealed black papillary growth involving the nodal structure [Figure 2].
Figure 2.

Longitudinal section of node showing black papillary growth involving nodal structure
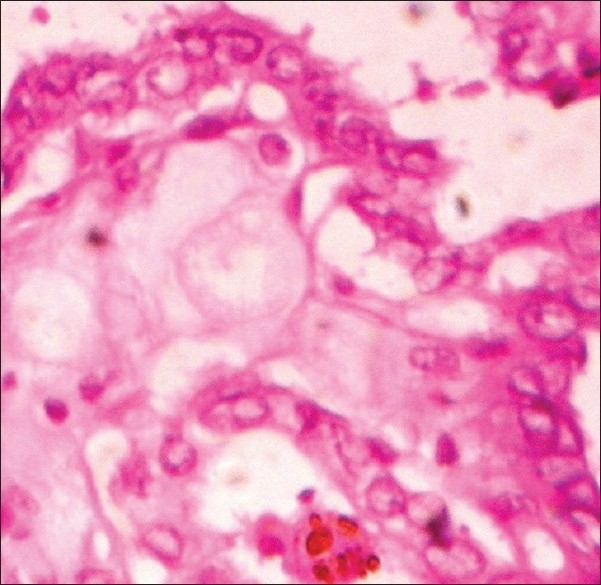
The microscopic examination of the sections from the node showed normal nodal architecture on one side, whereas on the other side, there were numerous randomly oriented papillae with a central fibrovascular core and a single stratified lining of cuboidal cells [Figure 3]. A few tumor cells were arranged in the form of follicles and they showed eosinophilic colloid with scalloped edges [Figure 4]. The stroma between the papillae was edematous and contained lymphocytes and macrophages. The tumor cells appeared optically clear (ground-glass appearance), containing large nucleus with fine chromatin and eccentrically placed nucleoli Figure 5]. Some tumor cells showed nuclear pseudoinclusions [Figure 5]. Some tumor cells had grooves arranged along the long axis of their oval-shaped nuclei giving a “coffee bean appearance” [Figure 5]. Psammoma bodies were also present in the stroma [Figure 6]. The psammoma body is a nonspecific finding, but along with other findings, it confirms PTC and its presence in the node signifies metastasis. Hence, on basis of the above histopathologic features, a final diagnosis of “Metastatic papillary thyroid carcinoma” was made for the node.
Figure 3.

Section of node showing normal nodal structure on one side and papillary growth on other side (H and E stain, 100×)
Figure 4.
Tumor cells arranged in form of follicles containing eosinophillic colloid with scalloped edges (H and E stain, 400×)
Figure 5.
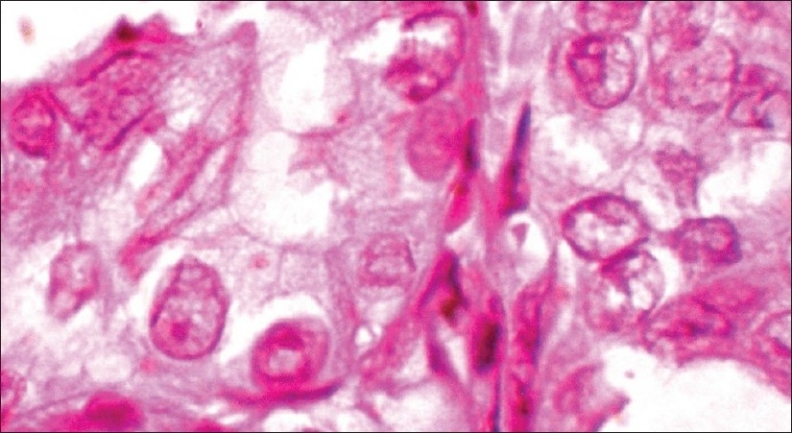
Tumor cells showing nuclear pseudo-inclusions and grooves (H and E stain, 400×)
Figure 6.
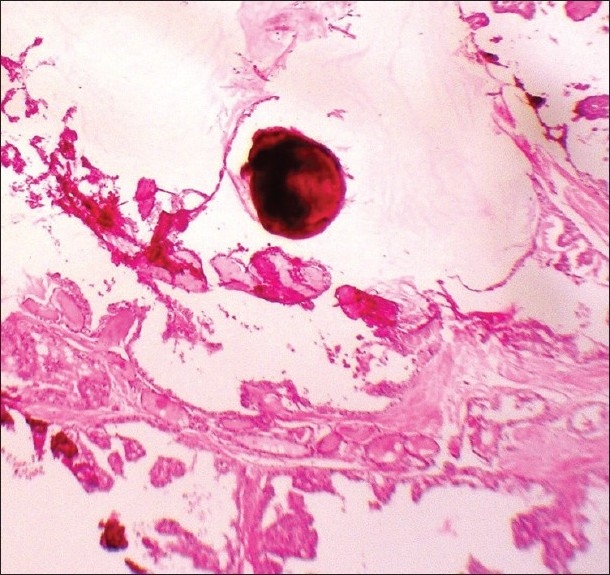
Section showing psammoma body in stroma (H and E stain, 100×)
DISCUSSION
Thyroid cancers are quite rare,[1] accounting for only 1.5% of all cancers in adults and 3% of all cancers in children, but the rate of new cases is increasing in the last decades. Thyroid cancers occur more frequently in women (with female-to-male ratio is near 3: 1) and can occur in any age group. Although it is most common in the 30 to 40 years age group, its aggressiveness increases significantly in older patients. The highest incidence of thyroid carcinomas in the world is found among female Chinese residents of Hawaii. During the last few years, the frequency of papillary cancer has increased, but this increase in frequency is related to an improvement in diagnostic techniques and the information campaign about this carcinoma.[2] In majority of patients, thyroid cancer presents with a nodule on their thyroid that typically does not cause symptoms. But, over 99% of thyroid nodules are not malignant. The major subtypes of thyroid carcinomas[1] and their relative frequencies include the following:
Papillary - 75-85% of cases
Follicular - 10-20% of cases
Medullary - 5% of cases
Anaplastic - <5% of cases
PTC is the most common type of thyroid cancer. It is also the predominant cancer type in children with thyroid cancer, and in patients with thyroid cancer who have had previous radiation to the head and neck.[3]
The thyroid is particularly sensitive to the effects of ionizing radiation. Exposure to ionizing radiation results in a 30% risk for thyroid cancer. A history of exposure of the head and neck to x-ray beams, especially during childhood, has been recognized as an important contributing factor for the development of thyroid cancer. PTC accounts for 85% of thyroid cancers due to radiation exposure. Several reports have shown a relationship between iodine deficiency and the incidence of thyroid carcinomas. Many other conditions have been considered as predisposing to papillary thyroid cancer (oral contraceptive use, benign thyroid nodules, late menarche, late age at first birth). Port et al. reported the “signature” of seven genes (ie, SFRP1, MMP1, ESM1, KRTAP2-1, COL13A1, BAALC, PAGE1) in papillary thyroid cancers after the Chernobyl accident, demonstrating by polymerase chain reaction (PCR) techniques their role in distinguishing such cases from sporadic forms.[2]
Papillary carcinoma is a relatively common well-differentiated thyroid cancer. Papillary/follicular carcinoma (mixed form) must be considered a variant of PTC. Despite its well-differentiated characteristics, papillary carcinoma may be overtly or minimally invasive. In fact, these tumors may spread easily to other organs. Papillary tumors have a propensity to invade lymphatics but are less likely to invade blood vessels.[2] Cervical metastasis (spread to lymph nodes in the neck) is present in 50% of small tumors and in over 75% of the larger thyroid cancers. The presence of lymph node metastasis in these cervical areas causes a higher recurrence rate but not a higher mortality rate. Distant metastasis (spread) is uncommon, but lung and bone are the most common sites. Tumors that invade or extend beyond the thyroid capsule have a worsened prognosis because of a high local recurrence rate.
Many cases of papillary thyroid cancer are subclinical. It typically arises as an irregular, solid or cystic mass that can be felt in the neck and arises from otherwise normal thyroid tissue.[4] Occasionally, symptoms such as hoarseness, neck pain, and enlarged lymph nodes do occur in people with thyroid cancer.[5] The lexicon of differential diagnoses includes De Quervain thyroiditis, Goiter—nontoxic and toxic nodular, Graves disease, Hurthle cell carcinoma, Thyroid lymphoma, Anaplastic thyroid carcinoma, Medullary thyroid carcinoma, Follicular thyroid carcinoma, Metastatic cancer, and Leukemias. The following laboratory workup[2] should be considered for patients with PTC:
Fine needle aspiration biopsy (FNAB) is considered the best first-line diagnostic procedure for a thyroid nodule; it is a safe and minimally invasive procedure.
Thyroid function
Thyriod stimulating harmone (TSH) suppression test
Imaging studies: Including chest radiography, computed tomography (CT scan), and magnetic resonance imaging (MRI).
Echography
Scintigraphy
Papillary thyroid cancer is strongly associated with some specific rearrangements of the RET proto-oncogene. If possible, the assessment of the RET proto-oncogene expression should be performed in any people having a relative with a history of papillary thyroid cancer.
Histopathologically, the PTC usually appears as a grossly firm mass that is irregular and not encapsulated. Microscopically, it is multifocal and has a propensity to invade lymphatics; it is less likely to invade blood vessels. They have a high tendency to metastasize locally to lymph nodes, which may produce cystic structures near the thyroid that are difficult to diagnose because of the paucity of malignant tissue. Furthermore, papillary tumors may metastasize to the lungs and produce a few nodules or the lung fields may exhibit a snowflake appearance throughout.
The tumor shows complete or partial papillary architecture with some follicles. The tumor shows numerous randomly oriented papillae with a central fibrovascular core and a single stratified lining of cuboidal cells. The tumor cells are arranged in the form of follicles and they show eosinophilic colloid with scalloped edges. The thyrocytes are large and show an abnormal nucleus and cytoplasm with several mitoses. They may have the so-called characteristic “orphan Annie eye” nuclear inclusions. The tumor cells appear optically clear (ground-glass appearance), containing large nucleus with fine chromatin and eccentrically placed nucleoli. There are also present nuclear pseudoinclusions which are formed due to finger-like invaginations of cytoplasm into the nucleus and are seen as large optically clear areas within the nucleus. They are membrane-bound structures surrounded by a thin rim of condensed basophilic chromatin. Some tumor cells have oval-shaped nuclei with grooves arranged along the long axis of nucleus giving a “coffee bean appearance.” The nuclear grooves are formed due to infolding of the nuclear membrane. Although the nuclear grooves are nonspecific and can be seen in several neoplastic and nonneoplastic cells, they are very common in thyroid carcinomas. The nuclear pseudoinclusion on the other hand is highly suggestive of “Papillary thyroid carcinoma,” particularly in combination with other characteristic nuclear features. Laminated basophilic psammoma bodies are also present in the stroma of papillary thyroid cancer tumors and they probably represent the remnants of dead papillae, in light microscopy. The psammoma body is also a nonspecific finding but along with other findings, it confirms PTC and its presence in the node signifies metastasis.[6] In the present case, all the above histopathologic features were clearly evident.
Other characteristics of the papillary carcinoma are that electron microscopy (E.M.) shows increased mitochondria, increased rough endoplasmic reticulum (RER), as well as increased apical microvilli. Immunohistochemistry findings usually have a carcino embryonic antigen (CEA)-negative, calcitonin-negative, thyroglobulin-positive, and keratin-positive pattern.[2] HBME-1 staining may be useful for differentiating papillary carcinomas from follicular carcinomas; in papillary lesions, it tends to be positive. Thyroglobulin can be used as a tumor marker for well-differentiated papillary thyroid cancer.[3]
The thyroid cancers are typically treated with complete removal of the lobe of the thyroid that harbors the cancer, in addition to the removal of most or all of the other side. The surgical treatment protocol[3] followed is: For minimal disease (diameter up to 1.0 cm)—hemithyroidectomy (or unilateral lobectomy) and isthmectomy may be sufficient. However, for gross disease (diameter over 1.0 cm)—total thyroidectomy and central compartment lymph node removal is the therapy of choice. Additional lateral neck nodes can be removed at the same time if an ultrasound-guided fine needle aspiration (FNA) and thyroglobulin (TG) cancer washing was positive on the preoperative neck node ultrasound evaluation. Papillary tumors tend to be more aggressive in patients over the age of 45 years. In such cases, it might be required to perform a more extensive resection, including portions of the trachea. Also, the sternocleidomastoid muscle, jugular vein, and accessory nerve are to be removed if such procedure allows apparently complete tumor resection.
External irradiation may be used when the cancer is unresectable, when it recurs after resection, or to relieve pain from bone metastasis. After around 4 to 6 weeks of surgical thyroid removal, the patient is given radioiodine therapy. This therapy is intended to both detect and destroy any metastasis and residual tissue in the thyroid. The treatment may be repeated 6-12 months after initial treatment of metastatic disease where disease recurs or has not fully responded.[3]
Patients are administered hormone replacement levothyroxine for life after surgery, especially after total thyroidectomy. Chemotherapy with cisplatin or doxorubicin has proven limited efficacy; however, it could be helpful for patients with bone metastases to improve their quality of life.[3]
Recently, the “high frequency thyroid ultrasound” (HFUS)[7] are being used to treat metastatic thyroid cancer neck lymph nodes that occur in patients who either refuse surgery, or are no longer a candidate for surgery. Small amounts of ethanol are injected under ultrasound-guided needle placement. A blood flow study is done prior to the injection, by power Doppler. The blood flow can be destroyed and the node becomes inactive, although it may still be there. Another interventional use for HFUS is to mark a cancer node one hour prior to surgery, to help locate the node cluster at the surgery. A minute amount of methylene dye is injected, under careful ultrasound-guided placement of the needle on the anterior surface, but not in the node. The dye will be evident to the thyroid surgeon when he opens the neck.
The main medical and legal problems related to papillary thyroid cancer treatment are vocal cord paralysis due to damage of the recurrent laryngeal nerve, damage of the parathyroid glands leading to temporary or permanent hypoparathyroidism, and toxic adverse effects of radioiodine administration. Always obtain informed consent for diagnostic procedures and treatments, explaining the procedures and their possible complications. Because radioiodine treatment may cause either teratogenesis or spontaneous abortions, patients should delay pregnancy for at least 1 year after radioiodine treatment.[2]
There are several scoring systems for assessing prognosis. Among them, the more often used systems[3] are as follows: AGES (Age, Grade, Extent of disease, Size); AMES (Age, Metastasis, Extent of disease, Size); MACIS (Metastasis, Age at presentation, Completeness of surgical resection, Invasion [extrathyroidal], Size), and TNM grading (Tumor, node, metastasis). In general, PTC has a high cure rate with 10-year survival rates for almost all patients with appropriate treatments.[4] If cancer is not extending beyond the capsule of the gland, life expectancy is minimally affected. Prognosis is directly related to tumor size (less than 1.5 cm [1/2 inch] good prognosis). The life expectancy of patients with this cancer is also related to their age, sex, and stage. The prognosis is better in female patients and better for younger patients than for those who are older than 45 years.[2]
CONCLUSION
This article presents a case of dual malignancy in a young boy of 17 years of age with a history of tobacco abuse for 6 years. In this, the entire lesional specimen revealed early SCC with microinvasion and all the level-1, -2, and -3 nodes were free of tumor, but only a single level-3 node was enlarged and it showed features suggestive of “Metastatic papillary thyroid carcinoma.” Hence, by this case report, we intend to highlight the importance of complete removal of any suspicious-looking mass—over and beyond the surgery planned, depending on surgeon's acumen. This case also emphasizes the duty of pathologists that each and every bit of tissue sent by surgeon should be extensively sampled and examined as even a single tissue bit can entirely change the diagnosis and treatment plan, as in this case.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Kumar, Abbas, Fausto . Robbins and Cotran pathologic basis of disease. 7th ed. Philadelphia: WB Saunders; 2008. pp. 1177–80. [Google Scholar]
- 2.Thyroid, Papillary Carcinoma; Luigi Santacroce, Silvia Gagliardi. [Last accessed on 2011 Mar 19]. Available from: http://www.emedicine.medscape.com/article/282276.overview .
- 3.Papillary thyroid cancer. [Last accessed on 2011 Mar 19]. Available from: http://www.en.wikipedia.org/wiki/Papillary_thyroid_cancer .
- 4.Papillary Cancer: The Most Common Thyroid Cancer; James Norman. [Last accessed on 2011 Mar 19]. Available from: http://www.endocrineweb.com/capap.html .
- 5.Thyroid Cancer; James Norman. [Last accessed on 2011 Mar 19]. Available from: http://www.endocrineweb.com/thyroidca.html .
- 6.Douglas P, Clark WC, Faquin . Thyroid cytopathology. 1st ed. Verlag: Springer; 2005. Papillary thyroid carcinoma; pp. 124–31. [Google Scholar]
- 7.Interventional thyroid ultrasound. [Last accessed on 2011 Mar 19]. Available from: http://www.en.wikipedia.org/wiki/Interventional_thyroid_ultrasound .


