Abstract
Background:
We present a review of the results of the current surgical management of acute cervical spine injuries in the Federal Capital Territory, Abuja, Nigeria. This is the first detailed retrospective study on the surgical management of patients with cervical spine injuries from Nigeria.
Methods:
The medical reports of patients with traumatic cervical spine and spinal cord injuries undergoing surgery from 1 August 2009 till 30 August 2010 were reviewed. Management and early results of outcome were ascertained and detailed consecutively in a prospective Microsoft Office Access® database (Microsoft Group of Companies). Frankel grading was used for pre- and immediate post-operative evaluation (within 48 hours). The Barthel index (BI) was used to classify patients as dependent or independent at follow-up.
Results:
Twenty consecutive patients presented with acute cervical spine and spinal cord injuries since August 2009. Twenty anterior cervical spine decompression and fixation with an iliac graft and an anterior cervical plate (ACDF) were performed in 18 patients. All operations were performed with general anaesthesia using standard techniques but without a microscope or a high speed drill. Of the 18 patients who were operated, 4 patients died within a short period following surgical intervention. Seven patients have made a full recovery and seven remain fully dependent. Only two of the dependent quadriplegic patients have become reintegrated back into the society.
Conclusion:
The management of spinal cord injuries in Abuja is evolving. The operations were performed adequately with much limited complement of equipment. Poor intensive care therapy is a major challenge and improvements in this area of care will likely lead to better patient outcomes.
Keywords: Anterior cervical discectomy, cervical spine traumatic instability, Nigeria, outcome, surgical fixation, trauma
INTRODUCTION
Literature from Nigeria on spinal injury is not only scanty, but also the majority of the existing ones have been by non-neurosurgeons.[10,12,24] The reports have also been hospital-based descriptive epidemiological surveys[12] and case reports.[9,24] Patients with cervical spine and spinal cord injuries were mostly managed conservatively.[3,9] The morbidity and mortality for conservatively managed patients reported from different parts of the country are high.[3,4,10,21,24]
Surgical management of spinal injuries has been rare in the reports. Therefore, the advances in spinal injury management practiced in other parts of the World have not been reflected in the published reports from Nigeria.
The management of spinal trauma in Abuja, Nigeria, is now undergoing change with the recent arrival in the city of another neurosurgeon who is particularly interested in the open surgical reduction and fixation of suitable cases. Patients can now be admitted and offered surgical intervention as soon as possible. This allows them to be mobilized and presented to rehabilitation centers early. The new service came into existence in August 2009 and has provided active surgical intervention and management for patients with spinal trauma. The patients in this report were operated via an anterior approach with decompression, iliac graft fusion, and plating (ACDF).
MATERIALS AND METHODS
We have kept a prospective database of all patients admitted with acute cervical spine trauma and cervical spinal cord injury. The demographics includes the age, gender, clinical presentation, type of injury, level of injury, radiological information, disability as measured with the Frankel grading scale, management, and outcome. Pre-operative and post-operative Frankel grades within the first 48 h were recorded. Final outcome, evaluated using the Bathel disability index, was scored by 30 September 2010. Patients and or their carers were contacted and the index applied by telephone questioning, clinic, and home visits.
The patients
The patients in this report were admitted and treated at two hospitals in Abuja. These were the National Hospital, Abuja, which is a public hospital and Cedarcrest Hospital, a private orthopedic/neurosurgery hospital. The patients had suffered a road traffic accident (19 cases) and diving accident (1 case), resulting in cervical spinal column injury and varying degrees of spinal cord injury.
Patients with acute cervical spine injuries have screening x-rays of the cervical spine to review spinal alignment and confirm the level of injury. The majority (19 of 20 patients) were investigated with an MRI scan [Table 1]. One patient who was neurologically intact and had grade 2 spondylolisthesis on x-ray had a CT scan performed. Additional CT and post-operative MRI were only performed if indicated. MRI was necessarily performed for five patients who travelled abroad for rehabilitation and in one patient who re-dislocated after surgery. Otherwise, follow-up radiology was mostly with plain radiography [Table 1].
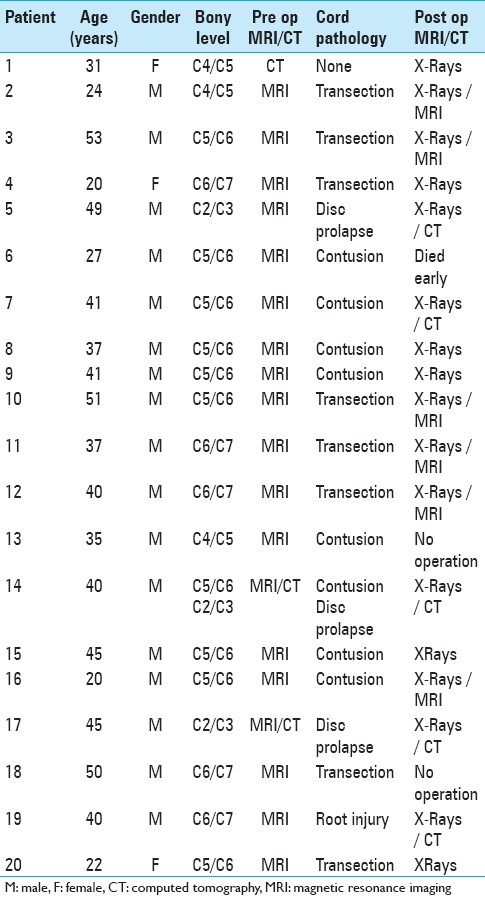
Table 1.
Shows the radiology of the patients admitted with acute spinal cord injury. The level of injury and modality of investigation preoperative and post operatively is shown. The actual significant spinal cord injury is recorded as contusion, transection, root injury or disc prolapse. Two patients were not operated and one died early before post operative imaging
The operation
The operations were usually performed on the day of admission or as soon as possible depending on other issues such as clinical condition, costs, and availability of personnel or equipment. All patients with unstable cervical spine injuries and those with compressive cord lesions (bone compression, hematoma, and disc prolapse) were offered urgent surgical intervention. The exclusion criteria for surgery were medical problems precluding anaesthesia and respiratory distress requiring airway control. Cost may have also been an issue in one case where the relatives refused surgical intervention.
The operation, ACDF, was a single level decompression in all these cases. Operations were performed as per routine approaches as previously documented by others. All patients had ceftriaxone, antibiotic, as prophylaxis at induction of anaesthesia and subsequently for 2 days after the operation. Surgery was performed following general anesthesia with the patient's supine and controlled neck traction using Gardner Wells skull traction. Weights were however only attached after established muscular paralysis or in some cases only after performing the discectomy. This was done in cases where there was a mass of disc behind the vertebrae. An image intensifier was used to localize the level of injury, review the spinal alignment and facetal reduction. The discectomies were performed using curettes and rongeurs. We did not use a microscope or high speed drill. Once the spinal cord was decompressed, an iliac graft was obtained and interposed using a Clowards disc spreader and skull traction. The anterior cervical plate (Implants International, Thornaby, UK) was applied. A wound drain was always utilized in the neck but occasionally in the hip wound.
Post-operative care and rehabilitation
A standard post-operative regimen was developed to care for the patients after surgery. This includes regular turns, close nursing care to prevent the following: aspiration, chest infection, urinary tract infection, and constipation. Early sitting up, a hard cervical collar, and physiotherapy were key elements of the post-operative care. Few of the patients required post-operative intensive care. Five of the patients could afford the cost of travel abroad for rehabilitation after surgery. All the others were managed locally and discharged home as soon as practicable.
RESULTS
Twenty patients have been admitted following an accident, with acute cervical spine and spinal cord injury. There were 17 men and 3 women. All except one had been involved in a road traffic accident (RTA). One young patient sustained neck trauma after he dived into a shallow swimming pool. The age range was 20 to 53 years (mean age 37.4). The patients had sustained injury to different parts of the cervical vertebrae but most of the injuries were at the C5/C6 level [Table 1]. There was injury to C2/C3 level in combination with a C5/C6 lesion in one patient. Another two had an isolated C2/C3 fracture. Injury at the C4/C5 level occurred in three patients and C6/C7 in five patients. All patients had some evidence of cervical spine instability such as vertebra fractures, disc injuries, kyphosis, spondylolisthesis, complete spinal dislocations, and ligamentous injuries. Following MRI scans in 19 patients, it was obvious that our patients had suffered varying degrees of spinal cord injuries as well. Some had complete dislocations and spinal cord transection and others had different degrees of spinal cord contusion. There were some with hematomyelia and compressive disc lesions on MRI [Table 1].
Of the 20 patients, 18 were operated and most within 48 h. The operation was performed on the day of the accident and as soon as possible following admission in 11 patients and at varying periods in the remainder. In one patient, it was performed as late as 3 weeks due to late referral and subsequent pre-operative complications (urinary tract infection and epistaxis). In a few cases, the operation was delayed because the surgeon was not available and due to early respiratory problems in one patient. We were unable to operate on two patients. One was not operated because the family refused treatment. We do not have any follow-up information. One other patient had respiratory distress and underwent an early tracheostomy. He was nursed in the intensive care unit for weeks before discharge to a rehabilitation center.
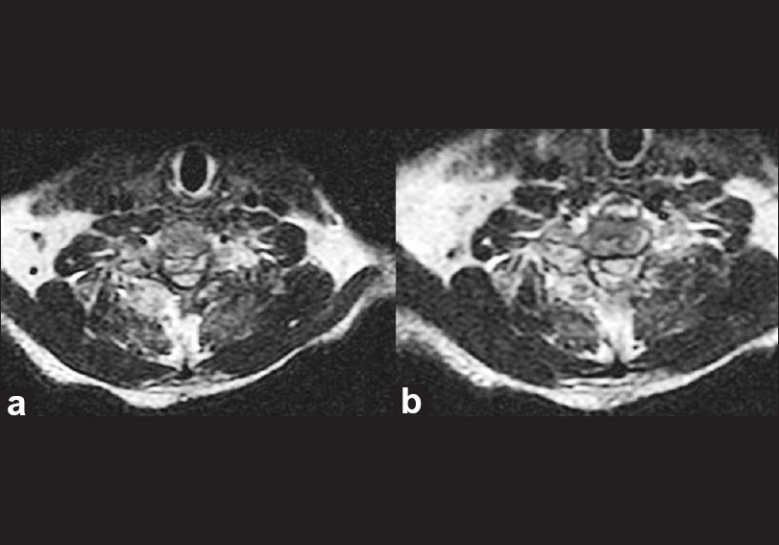
Eighteen patients underwent 20 operations. One patient re-dislocated 5 days after surgery and had a repeat operation performed. He was involved in a road traffic accident which led to a C6/C7 subluxation and complete spinal cord injury[Figures 1 and 2]. He developed respiratory failure and subsequently died from this complication. Another case had two operations. The patient had a complex fracture of C2 as well as significant spinal cord injury at C5/C6 associated with minor subluxation. We initially decompressed and fixed the C5/C6 level. A week later, he also underwent an ACDF and fixation at C2/C3. The case is illustrated in Figures 3 and 4.
Figure 1.
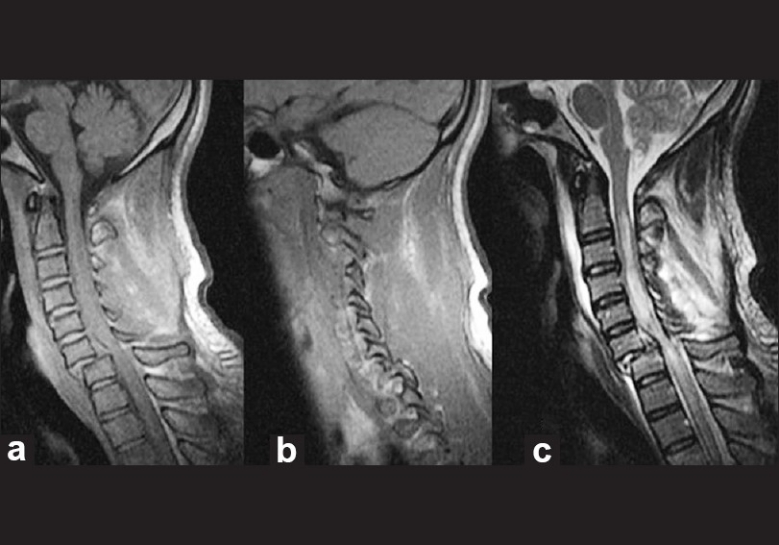
T1- and T2-weighted sagittal MRI scans showing the traumatic spondylolisthesis at C6/C7 (a-c). The image b demonstrates the facetal dislocation. The image on the right (c) shows the related spinal cord injury and a posterior disc fragment. This precludes spinal traction before reduction as the disc may be pushed back into the spinal cord causing more injury
Figure 2 (a, b).
T2 axial images of the patient described in case 1. The images show the related spinal cord injury and compression due partly to the posterior disc fragment and the bone
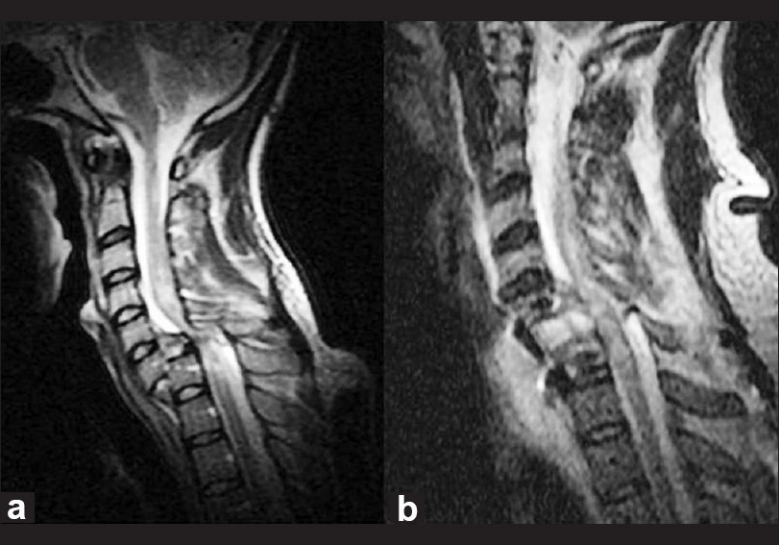
Figure 3 (a, b).
MRI scan of the patient (T1 and T2 sagittal images) showing the level of injury mostly at the C5/C6 level with spinal cord contusion. The disc at C2/C3 is also disrupted with no significant hematoma or soft tissue injury
Figure 4.
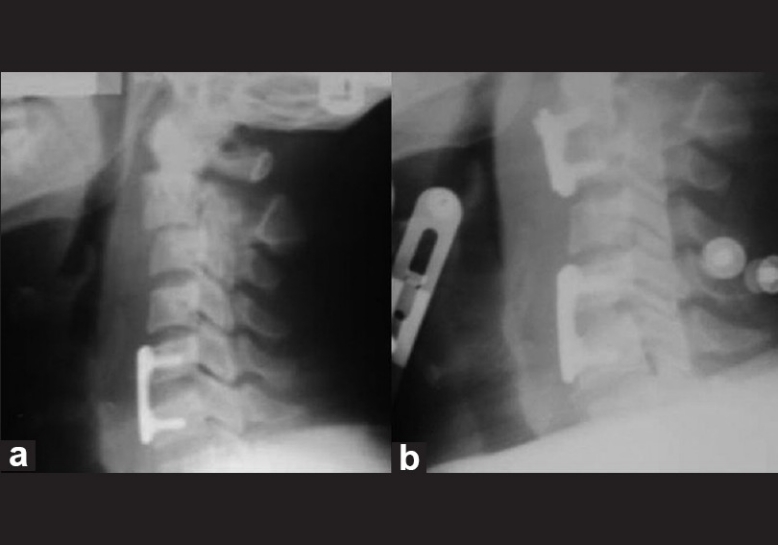
Lateral cervical x-rays of the patient after the first (a: C5/C6 fixation) and second operation (b: following the C2/C3 fixation)
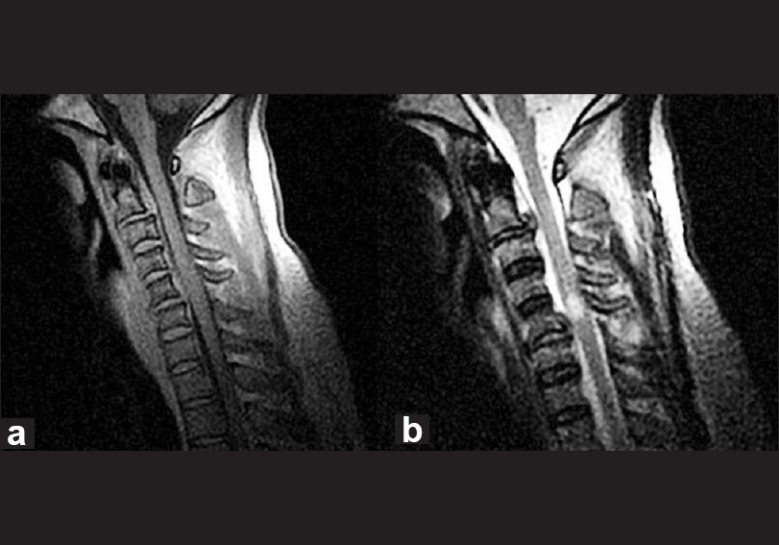
Seven patients had severe dislocations (grade 4) of the vertebrae and bifacetal dislocations posteriorly. We were unable to achieve posterior fracture/dislocation reduction in two patients. None underwent posterior fixation due to non-availability of instrumentation. One was described above. The other patient also had a C6/C7 grade 4 spondylolisthesis and fractures of the posterior elements [Figure 5]. He tolerated the procedure and remained well 9 months since surgery without need for posterior reduction and fixation.
Figure 5.
MRI scan of the patient (T2 sagittal images) showing the level of injury and dislocation, C6/C7 with spinal cord transection. Pre-operative image (a). The disc prolapse behind the vertebral body is significant. The post-operative image (b) is also shown following anterior approach, discectomy, and fixation with a hip graft and plate
We performed an urgent tracheostomy in four patients for respiratory distress and to aid airway toileting. Two of these patients died subsequently from respiratory failure.
Complications during surgery included a case in which there was leakage of cerebrospinal fluid seen at the time of the operation. This was related to the injury and not a surgical mishap. It was managed with a lumboperitoneal shunt. Otherwise all the operations were uneventful.
Morbidity and mortality in our patients are detailed in Table 2. Four patients died (20%). One death was from aspiration a day after surgery. The patient had recovered well from surgery and died next day while eating. The other deaths resulted from respiratory failure and hypoxia as previously alluded to. They were managed in the intensive care unit. Fourteen survived with good recovery in 7 patients and residual disability in the remainder (no follow-up information on 2 patients). Of the seven patients who have made a full recovery, two came in quadriplegic. The improvements were noticed immediately following surgery and continued to full functionality before discharge home. The post-operative Frankel grades improved within 48 h of surgery in seven patients (Patients numbered 3,6,7,8,11,14,15 in Table 2). It would appear that surgery was immediately beneficial in these patients [Table 2]. The seven patients who remained quadriplegic had complete spinal cord injury at the time of admission and remained so subsequently. Five of these patients went to other countries for rehabilitation after surgery. Three have returned and are being cared for at home. Of the three, two have returned to social activities using a motorized wheel chair. The follow-up period is detailed in Table 2. The total number of weeks of follow up was 389 (range: 0 – 53, mean: 21.61).
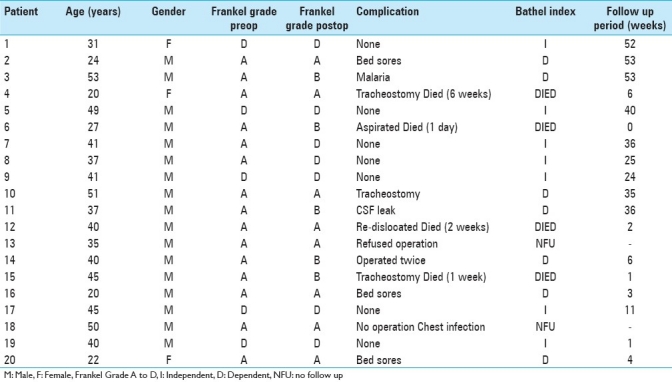
Table 2.
Shows the outcome of the patients admitted with acute spinal cord injury. The frankel grade was applied at admission preoperatively and postoperatively within 48 hours. Bathel Index was used for outcome and dichotomised into dependent and independent of activities of daily living. The follow up period in weeks after surgery is shown. Two patients were not operated and one died a day after surgery.
DISCUSSION
Following a Medline search, no articles were found reporting exclusively on cervical spine trauma in Nigeria. There are also no previous reports on the management of such problems in Abuja. However, there are many reports about spinal trauma and spinal cord injury in Nigeria, notably from Maiduguri and Enugu.[3,4,9–11,14–16,21,24] Previously reported experience also detailed the most common cause of spinal cord injury as a fall from trees.[15,21] Most patients with cervical spine injuries were managed conservatively.[9] Reports from other parts of the World on the current management of cervical spine and spinal cord injuries indicate that early surgical intervention with either anterior and posterior approaches lead to better outcomes.
Spinal cord injury is often associated with lifetime morbidity so early active management is crucial.[24] Surgical management of acute cervical spine and spinal cord injury has not been previously reported from Nigeria. This report therefore presents a significant shift in the management paradigm for patients in Abuja. In this review, important factors related to the surgical care of patients with acute cervical spine and spinal cord injury managed by a neurosurgeon in Abuja are discussed. Injuries resulting from cervical spine trauma due mostly to road traffic accidents are common problems seen in emergency departments in Abuja. There are currently no firm statistics on the scale of the problem.
Initial care of the spinal injured
The initial care of patients with acute traumatic lesions of the cervical spine is of paramount importance. Neurologic function at both the nerve root and cord levels can be adversely affected by excessive motion of the unstable spine.[18] Many of the patients in Nigeria have been moved from different hospitals before treatment. Most patients in a report from Enugu, Nigeria, 69 (66.4%), were received from private hospitals after a mean duration of 7 days.[10] This increases the related morbidity and mortality. Ideally, treatment starts at the site of trauma. Safe transportation and immobilization in braces are crucial.[7] It is known that following neck trauma, in-line stabilization using a hard cervical collar reduces movement of the cervical spine.[20] Airway management and maintenance of spinal immobilization are important factors in limiting the risk of secondary neurological injury.[20]
Diagnosis
Early diagnostic and clinical evaluations are important in determining the severity of the injury and making plans for subsequent management. Timely and appropriate imaging studies using x-rays, CT and MRI scans are essential to the cervical spine evaluation.[19] We have been able to offer early evaluation, investigation, and surgical management to the majority of our patients. With access to CT and MRI scans, most of our patients had an MRI scan to evaluate the severity and type of spinal cord injury.
Skull traction for facetal dislocation
Operations were performed routinely after attaching a Gardner Wells tong to the head. We did the traction in theatre under image guidance and not on the wards. No pre-operative closed reduction was performed because we had no means of checking the reduction on the wards. As in the cases illustrated in Figures 1, 2, and 5, we performed the approach and discectomy first before applying weights to aid reduction of the facet joints posteriorly. This was done in many cases to remove the mass of disc behind the vertebra body and avoid further injury to the cord. It is vital to evaluate the MRI scan carefully and identify posteriorly placed disc prolapses that could damage the cord following traction. The incidence of acute herniated nucleus pulposus was determined in a previous study involving 55 patients following cervical spine trauma.[17] The incidence of herniated nucleus pulposus was correlated with the patients’ present neurologic status and mechanism of injury. The incidence of herniated nucleus pulposus was highest in patients with bilateral facet dislocations (80%) and anterior cord syndromes (100%).[17] We therefore remove the disc prolapse first, before applying traction to aid facetal reduction [Figure 5]. Subsequently, the graft was interposed and the construct stabilized with an anterior cervical plate (Implants International, Thornaby, UK).
Anterior/and or posterior fixation
We performed only an anterior approach and discectomy with fracture fixation using an anterior cervical plate in all our patients. This proved adequate in 16 patients. However, posterior facetal reduction and fixation and subsequent anterior decompression and fixation would have been of benefit in at least three of our patients. We did not perform posterior cervical operations primarily due to non-availability of equipment for posterior fixation and other issues. Some of these issues are cost, length of operations, and subsequent need for intensive care.
We accept that surgical stabilization should be individualized for each patient. The procedure used should provide both immediate and prolonged stability at the site of instability.[23] Dvorak et al.[2] presented an algorithm to guide the choice of surgical approach in cervical subaxial burst fractures, distraction injuries, and translation or rotation injuries. The authors argued that burst or compression injuries and distraction injuries are more likely to be treated with a single anterior approach, whereas the more severe translation or rotation injuries may more commonly be approached posteriorly or with combined anterior and posterior surgery.[2] A previous study compared the results of combined anterior and posterior fixation/fusion with those of anterior fixation/fusion alone through a retrospective review of 50 patients.[22] In those with a bilateral dislocation, the clinical results, such as neurologic recovery and complications, were similar.[22] Overall, anterior fixation/fusion alone in a bilateral dislocation has been recommended as an alternative management method.[6,22] It has been argued that anterior instrumented fusion is at least as efficient as the posterior procedure in the management of cervical spine injuries and injuries including dislocations.[6] Further, these can be managed with anterior instrumented fusion alone.[6]
Conservative management of cervical spinal instability
Patients and their families have to pay for all operative interventions and acute care: the cost of a CT scan examination (CT spine) is uniformly about N40, 000 ($250 approximately) and MR is double that (average monthly salary in Nigeria is about N20, 000 or $120 approximately). The operation costs about N1,000,000 (one million Naira or equivalent of $6250 on average). The cost is therefore challenging for the average Nigerian. In this regards, conservative management remains a viable alternative and is often practiced. Management such as hard cervical collar, skull traction, Minerva jackets and plaster casts are sometimes used. The halo fixator has a well-defined place in the management of fractures of the cervical spine. Available evidence suggest that management of upper cervical spine fracture with halo fixator is safe and effective.[1,8] It is also however unavailable and unaffordable for most Nigerians.
Morbidity and mortality
The report details the management and outcome of patients with significant spinal column and spinal cord injury in Abuja. Morbidity in this series included significant bed sores, malaria, respiratory, and urinary tract infections. Considering the significant morbidity of these patients who were previously managed conservatively, our reported rate of clinically significant complications could be considered acceptable. It could be further minimized by good pre-operative planning, careful surgical technique, expert nursing care, and improved intensive care facilities.[5] In the report from Enugu, Nigeria, 36 (34.4%) of their patients with spinal cord injury died.[10] This was mainly from respiratory failure. In the report from Maiduguri, Nigeria, all the deaths, 3 (8.3%), occurred in patients with complete cervical spine lesion.[24] Four patients died in the present series. The deaths occurred early and within 6 weeks of surgical intervention. Three were due to poor respiratory support and subsequent hypoxic brain injury during admission in the intensive care unit. Seven patients remained fully dependent for all activities of daily living. This is balanced with the good results obtained in the remaining seven patients. Of particular interest are the two patients who were admitted quadriplegic and subsequently recovered with mild neurologic deficits.
Rehabilitation
Prolonged survival has resulted from better understanding of the pathophysiology of cord damage, as well as from the advances in antibiotic and ventilatory therapy.[18] Regional spinal injury centers have done much to increase the survival of and quality of life of cord injured patients. There is need to congregate these patients in spinal units where dedicated experts and facilities exist for better outcome of treatment and rehabilitation.[10] The high morbidity associated with spinal cord injury could be reduced through public enlightenment on road safety measures and establishment of spinal centers equipped to function.[24] The importance of the role of post-injury rehabilitation has been previously identified.[13] The establishment of rehabilitation centers would go a long way in improving the social rehabilitation and survival of the patients.
CONCLUSION
We have presented early and evolving experience of the management of patients with significant cervical spinal column and spinal cord injury in Abuja. We are advocates for early surgical management via an anterior approach, even with the limited complement of equipment. Posterior stabilization may however be required in a few patients, especially those with complete dislocation of the spine where 360° fusion may be more appropriate. Improved outcomes can be achieved with a careful approach and multidisciplinary integrated care including improvements in intensive care and effective rehabilitation centers.
This report could be a template for stimulating early surgical treatment for this group of patients in the country as a whole.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/156/89854
REFERENCES
- 1.Bransford RJ, Stevens DW, Uyeji S, Bellabarba C, Chapman JR. Halo vest treatment of cervical spine injuries: A success and survivorship analysis. Spine (Phila Pa 1976) 2009;34:1561–6. doi: 10.1097/BRS.0b013e3181a9702d. [DOI] [PubMed] [Google Scholar]
- 2.Dvorak MF, Fisher CG, Fehlings MG, Rampersaud YR, Oner FC, Aarabi B, et al. The surgical approach to subaxial cervical spine injuries: An evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976. 2007;32:2620–9. doi: 10.1097/BRS.0b013e318158ce16. [DOI] [PubMed] [Google Scholar]
- 3.Emejulu JK, Ekweogwu OC. Outcome of spinal cord injuries managed in a centre without modern imaging facilities. West Afr J Med. 2009;28:376–9. doi: 10.4314/wajm.v28i6.55028. [DOI] [PubMed] [Google Scholar]
- 4.Igun GO, Obekpa OP, Ugwu BT, Nwadiaro HC. Spinal injuries in the Plateau State, Nigeria. East Afr Med J. 1999;76:75–9. [PubMed] [Google Scholar]
- 5.Kasimatis GB, Panagiotopoulos E, Gliatis J, Tyllianakis M, Zouboulis P, Lambiris E. Complications of anterior surgery in cervical spine trauma: an overview. Clin Neurol Neurosurg. 2009;111:18–27. doi: 10.1016/j.clineuro.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Lambiris E, Kasimatis GB, Tyllianakis M, Zouboulis P, Panagiotopoulos E. Treatment of unstable lower cervical spine injuries by anterior instrumented fusion alone. J Spinal Disord Tech. 2008;21:500–7. doi: 10.1097/BSD.0b013e3181583b56. [DOI] [PubMed] [Google Scholar]
- 7.Lauweryns P. Role of conservative treatment of cervical spine injuries. Eur Spine J. 2010;19(Suppl 1):S23–6. doi: 10.1007/s00586-009-1116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Longo UG, Denaro L, Campi S, Maffulli N, Denaro V. Upper cervical spine injuries: Indications and limits of the conservative management in Halo vest. A systematic review of efficacy and safety. Injury. 2010;41:1127–35. doi: 10.1016/j.injury.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 9.Malomo AO, Emejulu JC, Odukogbe AA, Shokunnbi WA, Shokunbi MT. Conservative management of third trimester cervical spinal cord injury using Gardner-Wells tongs traction. Niger J Clin Pract. 2005;8:46–50. [PubMed] [Google Scholar]
- 10.Nwadinigwe CU, Iloabuchi TC, Nwabude IA. Traumatic spinal cord injuries (SCI): A study of 104 cases. Niger J Med. 2004;13:161–5. [PubMed] [Google Scholar]
- 11.Nwadinigwe CU, Ugezu AI. Management of penetrating spinal cord injuries in a non spinal centre: Experience at Enugu, Nigeria. Niger J Med. 2008;17:205–9. doi: 10.4314/njm.v17i2.37385. [DOI] [PubMed] [Google Scholar]
- 12.Nwankwo OE, Katchy AU. Outcome of a 12-week programme for management of the spinal cord injured with participation of patient's relations at Hilltop Orthopaedic Hospital, Enugu, Nigeria. Spinal Cord. 2003;41:129–33. doi: 10.1038/sj.sc.3101410. [DOI] [PubMed] [Google Scholar]
- 13.O’Dowd JK. Basic principles of management for cervical spine trauma. Eur Spine J. 2010;19(Suppl 1):S18–22. doi: 10.1007/s00586-009-1118-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Obalum DC, Giwa SO, Adekoya-Cole TO, Enweluzo GO. Profile of spinal injuries in Lagos, Nigeria. Spinal Cord. 2009;47:134–7. doi: 10.1038/sc.2008.93. [DOI] [PubMed] [Google Scholar]
- 15.Okonkwo CA. Spinal cord injuries in Enugu, Nigeria--preventable accidents. Paraplegia. 1988;26:12–8. doi: 10.1038/sc.1988.5. [DOI] [PubMed] [Google Scholar]
- 16.Olasode BJ, Komolafe IE, Komolafe M, Olasode OA. Traumatic spinal cord injuries in Ile-Ife, Nigeria, and its environs. Trop Doct. 2006;36:181–2. doi: 10.1258/004947506777978136. [DOI] [PubMed] [Google Scholar]
- 17.Rizzolo SJ, Piazza MR, Cotler JM, Balderston RA, Schaefer D, Flanders A. Intervertebral disc injury complicating cervical spine trauma. Spine (Phila Pa 1976) 1991;16(6 Suppl):S187–9. doi: 10.1097/00007632-199106001-00002. [DOI] [PubMed] [Google Scholar]
- 18.Rubin BD, Fielding JW. Neurological sequelae of cervical spine trauma. Bull Los Angeles Neurol Soc. 1981;46:36–40. [PubMed] [Google Scholar]
- 19.Sciubba DM, Petteys RJ. Evaluation of blunt cervical spine injury. South Med J. 2009;102:823–8. doi: 10.1097/SMJ.0b013e3181abe14e. [DOI] [PubMed] [Google Scholar]
- 20.Siddiqui AK. Airway management for cervical spine injury. Saudi Med J. 2009;30:1133–7. [PubMed] [Google Scholar]
- 21.Solagberu BA. Spinal cord injuries in Ilorin, Nigeria. West Afr J Med. 2002;21:230–2. doi: 10.4314/wajm.v21i3.28037. [DOI] [PubMed] [Google Scholar]
- 22.Song KJ, Lee KB. Anterior versus combined anterior and posterior fixation/fusion in the treatment of distraction-flexion injury in the lower cervical spine. J Clin Neurosci. 2008;15:36–42. doi: 10.1016/j.jocn.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 23.Stauffer ES, Rhoades ME. Surgical stabilization of the cervical spine after trauma. Arch Surg. 1976;111:652–7. doi: 10.1001/archsurg.1976.01360240032005. [DOI] [PubMed] [Google Scholar]
- 24.Umaru H, Ahidjo A. Pattern of spinal cord injury in Maiduguri, North Eastern Nigeria. Niger J Med. 2005;14:276–8. [PubMed] [Google Scholar]


