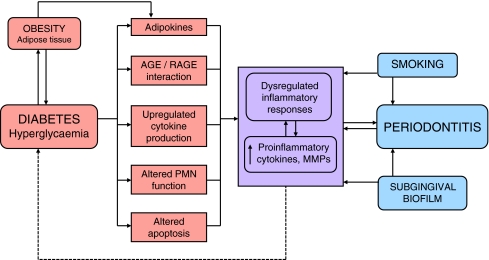
Fig. 4.
Schematic representation of the proposed two-way relationship between diabetes and periodontitis. Exacerbated and dysregulated inflammatory responses are at the heart of the proposed two-way interaction between diabetes and periodontitis (purple box), and the hyperglycaemic state results in various proinflammatory effects that impact on multiple body systems, including the periodontal tissues. Adipokines produced by adipose tissue include proinflammatory mediators such as TNF-α, IL-6 and leptin. The hyperglycaemic state results in deposition of AGEs in the periodontal tissues (as well as elsewhere in the body), and binding of the receptor for AGE (RAGE) results in local cytokine release and altered inflammatory responses. Neutrophil function is also altered in the diabetic state, resulting in enhancement of the respiratory burst and delayed apoptosis (leading to increased periodontal tissue destruction). Local production of cytokines in the periodontal tissues may, in turn, affect glycaemic control through systemic exposure and an impact on insulin signalling (dotted arrow). All of these factors combine to contribute to dysregulated inflammatory responses that develop in the periodontal tissues in response to the chronic challenge by bacteria in the subgingival biofilm, and which are further exacerbated by smoking