Abstract
A 56-year-old man presented with a painless cyst on the top of his head which has been increasing in size in the last 6 months. Due to his learning disability, he could not be dissuaded from his belief that the lump was a sign of brain prolapse which led to increasing agitation in the next 2 weeks. A provisional diagnosis of benign lipoma was made and prompt excision was performed in his best interests. The lesion was more cystic and fluctuant than that of a lipoma and hence it was sent for histological diagnosis. The report came back as a trichilemmal cyst with no signs of proliferation. Cosmetic outcome was reasonable at follow-up after 3 months. The patient was scheduled for regular review every 6 months.
Background
Painless soft tissue masses on the scalp are commonly encountered in clinical practice. The most likely diagnoses still remain as epidermoid cysts, sebaceous cysts and benign lipomas. However, clinicians should be cognisant of other possible, though uncommon, pathologies as differential diagnoses. We hereby present a case of soft scalp mass which was mis-diagnosed as benign lipoma until clarified by histological confirmation to be trichilemmal cyst, a relatively common condition known to carry proliferative and malignant potential in rare cases.
Case presentation
A 56-year-old patient with learning disability presented with a lump at top of his head. Due to problems in communication, history was obtained from his mother who had been living together with the patient since his birth. The lump appeared when patient was in his late teens, and had never been painful, infected or bled. It remained the size of a cherry and it had increased in size in the last 6 months. Patient was unaware of the lump until someone commented on it. Despite repeated assurance from his mother, patient became nervous with frequent agitation, thinking that it is a punishment from God and he would soon meet his demise. He had no history of trauma or developmental defect to his head and he takes losartan and hydrochlorothiazide for his hypertension. He had no personal or family history of solid tumours. On examination, there is a solitary 4×4 cm spherical mass arising from the vertex of his skull. The mass is soft and fluctuant and partially trans-illuminable. The surface consisted of normal looking skin of the near-alopecic scalp with no discolouration, cicatration or punctum. The mass was non-pulsatile and non-tender on palpation (figure 1). A provisional diagnosis of lipoma was made and when the benign nature of the lesion was explained to the patient; his mother elected to observe the lesion. Two weeks later, patient returned in an extremely distressed state and pleaded for an operation to prevent ‘his brains from sticking out’. In view of the patient’s inability to comprehend the situation, it was decided that the mass be removed in the best interests of the patient. The patient was offered the choice between a plastic surgery procedure (guaranteed cosmesis), or an office procedure (possible cicatration). Due to the long waiting time (up to 12 months) for plastics referral, patient opted for the latter.
Figure 1.
Soft fluctuant cystis mass measuring 4×4 cm arising from the vertex of the scalp.
Differential diagnosis
Differential diagnosis of trichilemmal cysts includes epidermoid cysts, benign lipomas, spindle cell lipoma, hibernomas and liposcarcoma. Epidermoid cysts broadly refer to cystic lesions that rise from invagination of the epidermis into deeper layers either accidentally or iatrogenically, as a complication of hair transplantation.1 Though considered benign and slow-growing, epidermoid cysts of the scalp are known to be associated with perforation of the skull2 and even the dura and the brain.3 Sebaceous cysts arise from cystic dilatation of the secretory glands of the hair follicles and in fact should be distinct from epidermoid cysts. However, in our medical literature, epidermoid cysts are often used synonymously and interchangeably with sebaceous cysts. Due to the semisolid contents, both epidermoid cysts and sebaceous cysts are often firmer to touch and less spherical in shape then truly fluid filled cysts. Due to the intrinsic anatomy of the scalp and face, benign lipomas are relatively uncommon with a case prevalence of 2%–14%.4 They are usually slow-growing and often ellipsoid rather than round on the scalp. Spindle cell lipoma is a variant of common lipomas which consists of significant fibrous tissue composing of spindle cells among the mature adipocytes.5 Most spindle cell lipomas are under 5 cm in diameter but can exceed 40 cm.6 Hibernomas are rare tumours thought to arise from the developmental remnants of brown adipose tissues. They often present as non-tender slow-growing masses with increased localised temperature.7 Hibernomas can grow to sizes of 5–10 cm in diameters with a preferred site at the thighs, interscapular area, the neck and the scalp.8 9 Although rare, liposarcomas of the scalp have been reported which were mostly the myxoid subtypes.10 11 They can mimic infected benign sebaceous cysts with their rapid growth and possible tissue necrosis. Diagnosis with fine-needle aspiration or local biopsy is known to be difficult as well-differentiated liposarcomas may look similar to benign lipomas.12 13
Treatment
The lesion was infiltrated with 2% lidocaine containing 1:10 000 norepinephrine. Due to ballooning effect of the lesion, an elliptical strip of skin was excised as the cyst was removed en bloc (figures 2 and 3). There was moderate tethering of the base to the underlying fascia which upon separation, led to profuse bleeding initially. Using electrodessication from a hyfrecator and subsequent prompt suturing, adequate haemostasis was eventually achieved. There was moderate tissue and cutaneous swelling when the suture was complete (figure 4). The wound was given a light dressing, and patient was observed in the waiting room for an hour before being sent home.
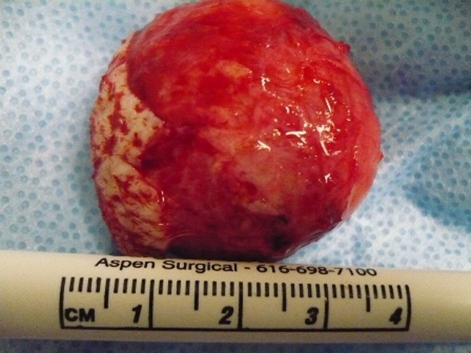
Figure 2.
Elliptical excision of skin marked out to facilitate better wound closure.
Figure 3.
Cystic mass removed en bloc with the ellipse of skin.
Figure 4.
Wound closed with adequate haemostasis albeit moderate degree of cutaneous oedema.
Outcome and follow-up
Sutures were removed after 10 days with satisfactory healing of the wound. When reviewed after 3 months, there was mild degree of cicatration at the site of excision (figure 5). Nevertheless, patient was not concerned by the cosmetic effects and repeatedly expressed gratitude to us for ‘putting his brains back in’! Given the cystic nature of the lesion and the obvious lack of lobulation in appearance, the author queried the diagnosis of lipoma, hence the lesion was sent off for histology. Indeed, histology report confirmed the diagnosis of trichilemmal cyst with no signs of active cell proliferation. In view of the low risks of malignancy for this patient, no further action was considered necessary. Patient was scheduled for routine review every 6-months thereafter.
Figure 5.
Review of patient after 3 months with mild cicatration at site of cyst excision.
Discussion
Trichilemmal (pilar) cysts and the commoner epidermoid (sebaceous) cysts are the two types of cutaneous cysts found in the hair bearing area that arise from different parts of the hair follicle unit, with a prevalence ratio of 1:4.14 In earlier days, all cutaneous cysts were erroneously referred to as sebaceous cysts until Pinkus15 pointed out in 1969 that trichilemmal cysts arise from the outer root sheath of the isthmus of the follicle, whereas sebaceous cysts arise from the follicular infundibulum and hence are distinct entities. Trichilemmal cysts usually occur in the hair bearing areas with a predisposition for the scalp, neck, trunk and gluteal region. They have a female dominance and with an age preponderance of over 60 years16 and occasionally reached extreme sizes of over 8 cm in diameter.17 18 Trichilemmal cysts are usually solitary lesions and can increase in size over time. They may partially rupture leading to low-grade inflammation due to the cystic contents. Though rare, proliferative forms of trichilemmal cysts have been reported which mimic squamous cell carcinomas histologically19 20 and may eventually progress to true local malignancy20–22 and even metastases.23 24 Some studies even suggested that the metastatic potential of proliferative trichilemmal cysts may even exceed that of squamous cell carcinomas.14 25 In our case, whether the preoperative diagnosis was a lipoma or trichilemmal cyst would in fact make no difference in our surgical management of excision. However, it would be necessary to confirm if there is a proliferative or malignant potential if it is turns out to be a trichilemmal cyst, as it would affect the postoperative management and overall prognosis.
Learning points.
-
▶
Soft tissue masses of the head and neck are commonly encountered in general practice.
-
▶
Benign lipomas, epidermoid cysts and sebaceous cysts remain as the most common diagnoses.
-
▶
Excision of lesions from the scalp can lead to profuse bleeding and adequate haemostasis must be ensured.
-
▶
Trichilemmal cyst usually presents as a slow-growing painless lump with cystic fluctuant consistency.
-
▶
Though rare, proliferative forms of trichilemmal cysts have been reported which mimic squamous cell carcinomas.
-
▶
Practising clinicians should be aware of trichilemmal cysts as a possible differential diagnosis when approaching soft tissue masses of the head and neck, and to exclude malignant potential which will affect prognosis and management.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Whiting DA, Stough DB. Posttransplant epidermoid cysts secondary to small graft hair transplantation. Dermatol Surg 1995;21:863–6 [DOI] [PubMed] [Google Scholar]
- 2.Ambo M, Kumakiri M, Chohno Y. Epidermoid cyst with perforation of the skull. J Am Acad Dermatol 2003;49:934–6 [DOI] [PubMed] [Google Scholar]
- 3.Cho JH, Jung TY, Kim IY, et al. A giant intradiploic epidermoid cyst with perforation of the dura and brain parenchymal involvement. Clin Neurol Neurosurg 2007;109:368–73 [DOI] [PubMed] [Google Scholar]
- 4.Truhan AP, Garden JM, Caro WA, et al. Facial and scalp lipomas: case reports and study of prevalence. J Dermatol Surg Oncol 1985;11:981–4 [DOI] [PubMed] [Google Scholar]
- 5.Haas AF, Fromer ES, Bricca GM. Spindle cell lipoma of the scalp: a case report and review. Dermatol Surg 1999;25:68–71 [DOI] [PubMed] [Google Scholar]
- 6.Eryilmaz M, Yigit T, Ozturk G, et al. Giant spindle cell lipoma of the posterior neck. Dermatol Surg 2007;33:1258–61 [DOI] [PubMed] [Google Scholar]
- 7.Lawson W, Biller HF. Cervical hibernoma. Laryngoscope 1976;86:1258–67 [DOI] [PubMed] [Google Scholar]
- 8.Furlong MA, Fanburg-Smith JC, Miettinen M. The morphologic spectrum of hibernoma: a clinicopathologic study of 170 cases. Am J Surg Pathol 2001;25:809–14 [DOI] [PubMed] [Google Scholar]
- 9.Naik R, Pai MR. Hibernoma of scalp: case report and review of literature. Indian J Cancer 1996;33:116–8 [PubMed] [Google Scholar]
- 10.Newlands SD, Divi V, Stewart CM. Mixed myxoid/round cell liposarcoma of the scalp. Am J Otolaryngol 2003;24:121–7 [DOI] [PubMed] [Google Scholar]
- 11.Herman O, Ariely D. Myxoid liposarcoma of the scalp: case report and literature review. Plast Reconstr Surg 1997;100:84–5 [DOI] [PubMed] [Google Scholar]
- 12.Collins BT, Gossner G, Martin DS, et al. Fine needle aspiration biopsy of well-differentiated liposarcoma of the neck in a young female. A case report. Acta Cytol 1999;43:452–6 [DOI] [PubMed] [Google Scholar]
- 13.Dey P. Fine needle aspiration cytology of well-differentiated liposarcoma. A report of two cases. Acta Cytol 2000;44:459–62 [DOI] [PubMed] [Google Scholar]
- 14.Sau P, Graham JH, Helwig EB. Proliferating epithelial cysts. Clinicopathological analysis of 96 cases. J Cutan Pathol 1995;22:394–406 [DOI] [PubMed] [Google Scholar]
- 15.Pinkus H. “Sebaceous cysts” are trichilemmal cysts. Arch Dermatol 1969;99:544–55 [PubMed] [Google Scholar]
- 16.Leppard BJ, Sanderson KV. The natural history of trichilemmal cysts. Br J Dermatol 1976;94:379–90 [DOI] [PubMed] [Google Scholar]
- 17.Karaman E, Duman C, Yagiz C. Giant trichilemmal cyst at the neck region. J Craniofac Surg 2009;20:961–2 [DOI] [PubMed] [Google Scholar]
- 18.Karaca S, Kulac M, Dilek FH, et al. Giant proliferating trichilemmal tumor of the gluteal region. Dermatol Surg 2005;31:1734–6 [DOI] [PubMed] [Google Scholar]
- 19.Brownstein MH, Arluk DJ. Proliferating trichilemmal cyst: a simulant of squamous cell carcinoma. Cancer 1981;48:1207–14 [DOI] [PubMed] [Google Scholar]
- 20.Satyaprakash AK, Sheehan DJ, Sangüeza OP. Proliferating trichilemmal tumors: a review of the literature. Dermatol Surg 2007;33:1102–8 [DOI] [PubMed] [Google Scholar]
- 21.Sethi S, Singh UR. Proliferating trichilemmal cyst: report of two cases, one benign and the other malignant. J Dermatol 2002;29:214–20 [DOI] [PubMed] [Google Scholar]
- 22.Garg PK, Dangi A, Khurana N, et al. Malignant proliferating trichilemmal cyst: a case report with review of literature. Malays J Pathol 2009;31:71–6 [PubMed] [Google Scholar]
- 23.Amaral AL, Nascimento AG, Goellner JR. Proliferating pilar (trichilemmal) cyst. Report of two cases, one with carcinomatous transformation and one with distant metastases. Arch Pathol Lab Med 1984;108:808–10 [PubMed] [Google Scholar]
- 24.Eskander A, Ghazarian D, Bray P, et al. Squamous cell carcinoma arising in a proliferating pilar (trichilemmal) cyst with nodal and distant metastases. J Otolaryngol Head Neck Surg 2010;39:E63–7 [PubMed] [Google Scholar]
- 25.Ye J, Nappi O, Swanson PE, et al. Proliferating pilar tumors: a clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J Clin Pathol 2004;122:566–74 [DOI] [PubMed] [Google Scholar]