Why read this summary?
Maltreatment of children is common, with 538 500 reported referrals to social services departments in England1 and 43 411 in Wales2 in the year ending 31 March 2008, although these probably underestimate the true scale of the problem. Child maltreatment includes neglect; physical, sexual, and emotional abuse; and fabricated or induced illness. It may present in various ways to different healthcare professionals, who have a “duty . . . to be proactive in safeguarding children”3 but often find it difficult to act on what they find.
Child maltreatment has short and long term harmful effects on a child’s health and wellbeing; emotional, interpersonal development; and behaviour; and in extreme circumstances it may lead to death. Children may present with both physical and psychological symptoms and signs that constitute alerting features of one or more types of maltreatment, which may also be observed as part of the interaction between the parent or carer and the child.4 The effects of maltreatment may continue throughout adulthood and include physical disability or disfigurement as well as the profound psychological consequences of anxiety, depression, substance misuse, and self destructive or antisocial behaviours, which may lead to difficulties in forming or sustaining close relationships, sustaining employment, and parenting capacity.3
Child maltreatment is under-recognised and inconsistently reported to children’s social care by healthcare professionals in England and Wales.5 The recent death of Baby Peter is yet another reminder of the consequences of missing the alerting features of child maltreatment.6 The recently published guidance from the National Institute for Health and Clinical Excellence (NICE) aims to raise the awareness of healthcare professionals to the alerting features of child maltreatment.7 It also aims to support healthcare professionals who are not specialists in child protection in identifying children who may be being maltreated and who require further multiagency assessment8 to confirm or exclude child abuse or neglect. The scope of this guidance does not cover family and social risk factors, which may in themselves be alerting features. The guidance should not be used as a definitive diagnostic tool to prove or disprove maltreatment. This article summarises key points in the NICE guidance.
Key points
NICE recommendations are based on systematic reviews of best available evidence. When minimal evidence is available, recommendations are based on the Guideline Development Group’s experience and opinion of what constitutes good practice. For this guidance, the Guideline Development Group used a formal Delphi consensus process when the group did not reach a congruent opinion.
Alerting features
The guideline recommendations refer to “alerting features” in the following categories.
Physical features
Physical features include any serious or unusual injury with an absent or unsuitable explanation, and particularly in the following categories: abrasions, bites, bruises, burns, cold injuries, cuts, lacerations, ligature marks, petechiae, scalds, scars, and strangulation marks. They also include various sites of internal injury including fractures, spinal and intracranial injuries (including subdural haemorrhage), intra-abdominal and intrathoracic injuries, eye injuries (including retinal haemorrhage), and oral injuries. The recommendations describe specific attributes of these injuries and of the child that should lead the healthcare professional to consider or suspect child maltreatment; in so doing, the recommendations draw attention to the age and developmental stage of the child and the suitability of the explanation given by the parents or carers.
Sexual abuse
Several recommendations concern alerting features that may indicate possible sexual abuse, with particular attention to the child’s age and sexual development. These features include anogenital injuries, symptoms, and signs; sexually transmitted infections, pregnancy; and sexualised behaviours.
Clinical presentations
Clinical presentations include (a) unusual patterns of use of medical services and attendance at medical services; (b) discrepant clinical picture (including fabricated or induced illness); (c) poor school attendance attributed to ill health; as well as (d) some particular indicators of ill health (apparent life threatening event; hypernatraemia; ingestion of substances including poisoning; nasal bleeding; and near drowning).
Neglect
Neglect includes abandonment and several aspects of failure of provision and failure of supervision. Many of these features must be persistent for a healthcare professional to consider or suspect neglect. Aspects of neglect through failure of provision may include a child who persistently presents as dirty or smelly, with unsuitable clothing, severe infestations, with untreated tooth decay (when NHS treatment is available); whose home conditions are unhygienic or unsafe; or who receives inadequate provision of food or medication. Other aspects of neglect through failure of provision may include lack of adherence to necessary medical advice and persistent failure to engage with relevant child health promotion programmes, such as immunisation, health and development reviews, and screening. Failure of supervision may be indicated by injuries—for example, a burn, sunburn, an ingestion of a harmful substance, or an animal bite.
The child’s emotional, behavioural, and interpersonal functioning
This section includes a child’s particular behaviours, emotional states, patterns of interpersonal functioning, and other aspects of the child’s functioning. These behaviours comprise a wide range of features including aggression; fearfulness; dissociation; low self esteem; indiscriminate contact or affection seeking; self harm; running away from home; body rocking; aspects of eating and feeding; and soiling and wetting behaviour. Patterns of potential concern include age inappropriate behaviour; marked change in emotional or behavioural state; and repeated, extreme, or sustained emotional responses by a child that are out of proportion to a situation and are not expected for his or her age and developmental stage.
Interactions between parent and child
Several aspects of interactions between a child and the parent or carer may be harmful, especially when persistent. They include emotional unavailability and unresponsiveness from the parent or carer; hostility towards and rejection and scapegoating of a child; interactions and expectations that are inappropriate for the age of the child, including inappropriate threats or methods of disciplining; exposure to domestic abuse; using the child to fulfil the parent’s or carer’s needs (for example, involving the child in marital disputes); and failing to promote the child’s socialisation by isolation or lack of stimulation or education, or by involving the child in unlawful activities.
Terminology
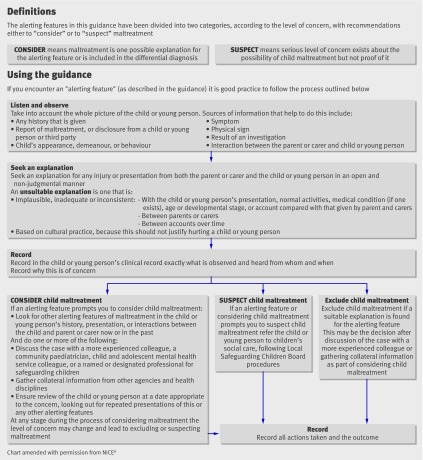
The terms “consider” and “suspect” have been used in the guidance to indicate the level of concern with respect to the various alerting features. These two terms reflect the action(s) to be taken by the healthcare professional when encountering the particular alerting feature (figure). The associated actions are intended to direct healthcare professionals to resources or ways of thinking that will enable them to overcome barriers to recognising maltreatment. “Consider” means that maltreatment is one possible explanation for the alerting feature or is included in the differential diagnosis.
When to suspect maltreatment of a child
The actions recommended in the figure will lead the healthcare professional to exclude maltreatment, to continue to keep the case under consideration, or to move to a stage of heightened concern where they suspect maltreatment.
“Suspect” means a serious level of concern about the possibility of maltreatment but is not proof of it. This may trigger a child protection investigation, which may indicate the need for starting child protection procedures and/or offering supportive services to the family or may lead to alternative explanations for the reported concerns being identified.
The guidance takes account of alternative causes of the alerting features, both in the recommendations and the processes associated with considering and suspecting child maltreatment.
Overcoming barriers
Child maltreatment is a sensitive and emotive subject. Healthcare professionals face many obstacles to recognising and responding to possible maltreatment (box). This guidance aims to empower and help them to overcome these obstacles, to encourage the appropriate course of action to protect the child or young person from further harm, and to reduce both delay in timely action and the high cost of abuse and neglect to individuals and to society.3 Support, supervision, education and training of ‘front line staff’ will be essential if this guidance is to be implemented successfully. Improving the quality of recognition should result in the right child being referred to specialist services for further assessment and protection from further maltreatment.
Obstacles for health professionals in identifying child maltreatment
Concern about missing a disorder which is treatable
Discomfort of disbelieving, thinking ill of, suspecting, or wrongly blaming a parent or carer
Fear of losing a positive relationship with a family already under the care of the health professionals
Divided duties towards adult and child patients and breaching confidentiality
An understanding of the reasons why the maltreatment might have occurred and a belief that the parent or carer did not intend to harm the child
Fear of loss of control over the child protection process and doubts about the benefits
Stress
Personal safety
Fear of complaints
Further information on the guidance
Background
In 2008, 29 200 children in England and 2320 in Wales (including 420 and five unborn children respectively) were the subject of a child protection plan.9 This translates into rates (per 10 000 children younger than 18 years (excluding unborn children) in England) of 26 for any type of abuse, 12 for neglect, three for physical abuse, two for sexual abuse, seven for emotional abuse, and two for multiple types of abuse. There were 538 500 reported referrals about child maltreatment to social services departments in England1 and 43 411 in Wales2 during the year ending 31 March 2008. These figures represent those regarded by children’s social care services as “at risk” of maltreatment and probably underestimate the true scale of the problems, with surveys of the general public suggesting that 15-20% of people have suffered some form of maltreatment as a child.10 This underestimation results partly from a lack of recognition or reporting by professionals, including healthcare professionals, of suspected child maltreatment.
Social advantage does not necessarily protect a child from maltreatment, which also affects children in higher socioeconomic groups. There is compelling evidence (including that reported by England’s national service framework for children, young people, and maternity services) for the harmful short and long term effects of various forms of child maltreatment, which affect all aspects of the child’s health, development, and wellbeing and which can last into and throughout adulthood.3 The national service framework states: “The high cost of abuse and neglect both to individuals and to society underpins the duty on all agencies to be proactive in safeguarding children.” Some evidence from several randomised control trials suggests that interventions to prevent abuse or recurrence of abuse have some positive effect on the short and long term wellbeing of the child.11
NICE anticipated that this guidance would support and update the implementation of relevant recommendations from both the English and the Welsh national service frameworks for children, young people, and maternity services.3 12
This guidance is predicated on an acceptance that the welfare of children is the paramount consideration as articulated in the United Nations’ Convention on the Rights of the Child, specifically article 19, which deals with child maltreatment.13 The guidance applies to all children and young people up to 18 years of age.
Methods
The remit of the guidance was discussed at length with the Department of Health. After this, workshops were held with key stakeholders and NICE to discuss the purpose of the guidance, its remit, and its main outcomes. Information gathered from these meetings formed the basis of the content of the scope outlined below. It was decided that we would provide guidance integrating published literature with consensus opinion. Formal Delphi consensus methods would be adopted for part of this process.
The guidance uses the definitions of various forms of child maltreatment set out in Working Together to Safeguard Children8, based on the concept of significant harm as the threshold for protective intervention, which was introduced in the Children Act 1989.
For child protection to be effective, all agencies must cooperate and do so at the earliest point possible. This guidance tackles the crucial contribution of healthcare professionals to this endeavour by setting out the indicators that will alert healthcare professionals to the recognition of possible child maltreatment.
The guideline was developed by the National Collaborating Centre for Women’s and Children’s Health (NCC-WCH) in accordance with the NICE guideline development process as outlined in the NICE technical manual.14 A multiprofessional Guideline Development Group was established, and this included one child and adolescent psychiatrist, two general practitioners, one nurse, one health visitor, one child psychologist, one accident and emergency consultant, three consultant community paediatricians, one consultant hospital paediatrician, one social worker, and four patients or consumer members. All committee members were recruited because of their expertise in child protection.
The technical team from the NCC-WCH provided methodological support for the guideline development process; undertook systematic literature searches, retrieval, appraisal, and synthesis of the evidence; did health economics modelling; and together with the chair of the Guideline Development Group wrote successive drafts of the guideline. A clinical adviser with expertise in child protection and the related evidence base was recruited to support the technical team. For each clinical question, recommendations were derived using, and explicitly linked to, the evidence that supported them. The development group used formal (Delphi) and informal consensus methods to agree evidence statements and recommendations, including the areas where important clinical questions were identified but no substantial evidence existed. The group used the Delphi consensus process when there was a lack of relevant literature on a clinical feature’s importance in child maltreatment; when the group’s members were unable to agree; and when the group required external validation from a wider group of experts (the Delphi panel) for their opinion. The Delphi panel comprised child protection experts (clinicians with substantial experience in child protection).
The process by which the evidence statements informed the recommendations was summarised in a section in the relevant evidence review. Registered stakeholder organisations were given an opportunity to comment on the scope of the guideline at the initial stage of development and on the final draft at the concluding stage. Both the documents were revised taking into account the comments received. Future updates of the guidance will be prepared in line with the NICE guideline development process.
Areas for further research
Fractures—How can abusive fractures be differentiated from those resulting from conditions that lead to bone fragility and those resulting from unintentional injury, particularly in relation to metaphyseal fractures?
Anogenital symptoms, signs, and infections—What is the association between anogenital warts and sexual abuse in children of different ages?
Fabricated or induced illness—Are the indicators of fabricated or induced illness as described in the recommendations valid for discriminating fabricated or induced illness from other explanations?
Emotional and behavioural states—Which aspects of behaviours and emotional states, as “alerting” individual signs, discriminate maltreated children from non-maltreated children in the healthcare setting?
Recurrent abdominal pain—What is the association between unexplained recurrent abdominal pain and child maltreatment?
The members of the Guideline Development Group are Jane Appleton, reader in Primary and Community Care (nursing), School of Health and Social Care, Oxford Brookes University; Tricia Brennan, consultant paediatrician (emergency medicine), Children’s Hospital, Sheffield; Geoff Debelle (from 2008), consultant paediatrician, Birmingham Children’s Hospital Foundation NHS Trust and designated doctor, South Birmingham Primary Care Trust; Susan Dunstall, lay member, policy adviser for Health and Family Support, National Society for the Prevention of Cruelty to Children; Danya Glaser, Chair of the Guideline Development Group and consultant child and adolescent psychiatrist; Andrea Goddard, consultant paediatrician (general), St Mary’s Hospital and designated doctor for Child Protection, Westminster Primary Care Trust; Kathryn Gutteridge, lay member, consultant midwife, Sandwell and West Birmingham NHS Trust; Christine Habgood, general practitioner, Brighton and Hove; Chris Hobbs, consultant paediatrician (community), St James’s University Hospital, Leeds; Elizabeth Hughes, consultant nurse in safeguarding children, Sheffield Primary Care Trust; Anne Livesey, consultant paediatrician (community), Children and Young People’s Trust, Brighton and Hove; David Lucey, independent clinical child psychologist, York; Rosemary Neary, lay member, managing director/founder, Eaton Foundation; Annmarie Reeves, senior practitioner (social work), Milton Keynes; Peter Saunders, lay member, chief executive, National Association for People Abused in Childhood; Anubha Sinha, general practitioner, Bidford-on-Avon; David Vickers (resigned in April 2008; replaced by Geoff Debelle), consultant paediatrician (community), South Cambridgeshire Primary Care Trust.
The members of the National Collaborating Centre for Women and Children’s Health technical team are Jiri Chard, senior research fellow; Rupert Franklin, work programme coordinator; Eva Gautam-Aitken, project manager; Paul Jacklin, senior health economist; Alison Kemp, clinical adviser, consultant paediatrician and professor in child health; Angela Kraut, research fellow, Monica Lakhanpaul, clinical co-director, consultant paediatrician/senior lecturer in child health; Carolina Ortega, work programme coordinator; Julia Saperia, lead research fellow; Samantha Vahidi, senior work programme coordinator; Danielle Worster, information scientist..
Contributors: ML wrote the initial draft of the article using material developed collectively by the Guideline Development Group. JS, AK, and DG contributed to the revision and the final draft of this article. They have all approved this version.
Funding: The National Collaborating Centre for Women’s and Children’s Health was commissioned and funded by the National Institute for Health and Clinical Excellence to write this summary.
Competing interests: All authors were members of the Guideline Development Group: JS was the lead research fellow, ML the clinical codirector, and AK the adviser; DG chaired the group. DG has acted as an expert witness (as part of her NHS contract) in the subject of this paper.
Provenance and peer review: Commissioned; not externally peer reviewed.
Cite this as: BMJ 2009;339:b2689
This is one of a series of BMJ summaries of new guidelines, which are based on the best available evidence; they highlight important recommendations for clinical practice, especially where uncertainty or controversy exists.
References
- 1.Department for Children, Schools and Families. DCSF: referrals, assessments and children and young people who are the subject of a Child Protection Plan, England—year ending 31 Mar 2008 (additional tables including England summary tables and local authority tables). 2008. www.dcsf.gov.uk/rsgateway/DB/SFR/s000811/additional_tables.xls.
- 2.Data Unit Wales. Dataunitwales Dissemination Tool. 2009. http://dissemination.dataunitwales.gov.uk/webview/index.jsp.
- 3.Department of Health. National Service Framework for children, young people, and maternity services—core standards. London: DH, 2004. [DOI] [PubMed]
- 4.Glaser D. Emotional abuse and neglect (psychological maltreatment): a conceptual framework. Child Abuse and Neglect 2002;26:697-714. [DOI] [PubMed] [Google Scholar]
- 5.Gilbert R, Kemp A, Thoburn J, Sidebotham P, Radford L, Glaser D, et al. Recognising and responding to child maltreatment. Lancet 2009;373:167-80. [DOI] [PubMed] [Google Scholar]
- 6.Wise J. Systemic failings in NHS contributed to death of Baby P. BMJ 2009;338:b1967. [Google Scholar]
- 7.National Institute for Health and Clinical Excellence. When to suspect child maltreatment. 2009. (Clinical guideline 89.) www.nice.org.uk/CG89.
- 8.HM Government. Working together to safeguard children. London: Stationery Office, 2006.
- 9.National Society for the Prevention of Cruelty to Children. Child protection register statistics. 2009. www.nspcc.org.uk/Inform/resourcesforprofessionals/Statistics/ChildProtectionRegisterStatistics/england_wdf49858.pdf.
- 10.Gilbert R, Spatz Widom C, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet 2009;373:68-81. [DOI] [PubMed] [Google Scholar]
- 11.MacMillan HL, Wathen CN, Barlow J, Fergusson DM, Leventhal JM, Taussig HN. Interventions to prevent child maltreatment and associated impairment. Lancet 2009;373:250-66. [DOI] [PubMed] [Google Scholar]
- 12.Welsh Assembly Government. National Service Framework for Children, Young People and Maternity Services in Wales. 2005. www.wales.nhs.uk/sites3/home.cfm?OrgID=441
- 13.Office of the United Nations High Commissioner for Human Rights. Convention on the Rights of the Child. 1990. www.unhchr.ch/html/menu3/b/k2crc.htm
- 14.National Institute for Health and Clinical Excellence. The guidelines manual. London: NICE, 2007.