Abstract
Supportive housing, defined as subsidized housing in conjunction with site-based social services, may help improve the health and residential stability of highly disadvantaged individuals. This study examined changes in health status, quality of life, substance use, health care utilization, and residential stability among 112 homeless and vulnerably housed individuals who applied to a supportive housing program in Toronto, Canada, from December 2005 to June 2007. Follow-up interviews were conducted every 6 months for 18 months. Comparisons were made between individuals who were accepted into the program (intervention) and those who were wait-listed (usual care) using repeated-measures analyses. Individuals who were accepted into the housing program experienced significantly greater improvements in satisfaction with living situation compared with individuals in the usual care group (time, F3,3,261 = 47.68, p < 0.01; group × time, F3,3,261 = 14.60, p < 0.01). There were no significant differences in other quality of life measures, health status, health care utilization, or substance use between the two groups over time. Significant improvement in residential stability occurred over time, independent of assigned housing group (time, F3,3,261 = 9.96, p < 0.01; group × time, F3,3,261 = 1.74, p = 0.17). The ability to examine the effects of supportive housing on homeless individuals was limited by the small number of participants who were literally homeless at baseline and by the large number of participants who gained stable housing during the study period regardless of their assigned housing status. Nonetheless, this study shows that highly disadvantaged individuals with a high prevalence of poor physical and mental health and substance use can achieve stable housing.
Keywords: Supportive housing, Homelessness, Health status, Health care utilization
Introduction
In comparison to the general population, homeless people are at increased risk for all-cause mortality1–5 and often experience higher rates of acute and chronic health conditions.6 Nearly two thirds of homeless adults suffer from mental illness and/or substance abuse.6 Lack of preventative health care, difficulty in accessing needed care, and exposure to certain environments further contribute to negative health outcomes among this population.7,8
The combination of housing and support, which includes subsidized housing in conjunction with either site-based or community-based social services, has been widely studied as an approach to assist homeless people improve their residential stability. Approaches to how housing and support are delivered are broadly differentiated in the research literature as “supportive housing” or “supported housing.”9–13 Supportive housing provides tenants with onsite or closely linked medical, mental health, and substance abuse services. In a supportive housing approach, support and services are integrated into the housing setting, although staff may be on call and not physically on site in the case of supervised apartments.11 In contrast to supportive housing, supported housing allows individuals to live independently and access regular housing in the community while offering them individualized and flexible support services that are client-centered.12,13
Overall, there is a lack of rigorous research evaluating the effectiveness of supportive housing, which includes a wide range of housing programs, complicating the interpretation of the research that has been conducted. Previous longitudinal research demonstrates that supportive housing can lead to long-term residential stability, improved quality of life, and a reduction in the frequency and length of hospitalizations and length of time in jail.14–18 However, it is less clear whether the provision of supportive housing has a positive impact on physical health status or whether supportive housing can significantly reduce mental health symptoms or substance use among homeless individuals.14–18 Moreover, these studies were conducted in the United States, where over half of homeless people lack health insurance.19 It is uncertain what the effects of providing supportive housing would be for homeless people living within a system of universal health insurance. The changes in health care utilization seen in US studies may not be seen in other countries such as Canada, where there are fewer financial barriers to accessing health care.20
In this prospective study, we examined a supportive housing program for homeless and vulnerably housed people in Toronto, Canada. We examined changes in health status, quality of life, substance use, health care utilization, and residential stability among individuals who were accepted into the program compared with those who were wait-listed for the program. We hypothesized that individuals placed in supportive housing (intervention) would report greater improvements in physical and mental health status, quality of life, residential stability, and decreases in substance use and health care utilization compared with the group who did not receive housing (usual care).
Methods
Program Description
This study enrolled participants who applied to a newly opened supportive housing program for homeless and vulnerably housed individuals in Toronto, Canada. The supportive housing program is operated by the Evangel Hall Mission, a not-for-profit organization that also provides meals and support services to homeless and low-income individuals. The program is located in one building with 84 units, of which 66 were allocated for single adults. The units include bachelor, one-bedroom, and two-bedroom apartments which are fully furnished and have private bathrooms and kitchens. Tenants have access to a shared kitchen facility, a drop-in center offering meals and outreach services, as well as a medical and dental clinic providing free services. Individuals accepted into the program received rental subsidies and paid rent-geared-to-income (not exceeding 30% of income). The program partnered with COTA Health, a mental health and community support services organization that provided onsite support to tenants. Specifically, tenant support workers assisted residents with mental illness to transition into the housing program as well as providing ongoing help with living skills, counseling, and advocacy.
Sample Recruitment and Follow-up
This study sought to enroll applicants to the Evangel Hall supportive housing program who were interviewed for single adult housing units, including individuals with severe and persistent mental illness referred by COTA Health (30 units) and individuals without severe and persistent mental illness (36 units). The remaining units were reserved for families with children and individuals with acquired brain injury referred by COTA Health, nearly all of whom were accepted into housing. Because no comparison group was available for these applicants, they were excluded from this study.
Applications for the housing program were accepted from homeless and vulnerably housed individuals, most of whom were already receiving services from Evangel Hall Mission or other community-based service providers. Eligible applicants must have met at least one of the following criteria: (1) were homeless, defined as living and sleeping outside or on the street or sleeping in an emergency shelter or hostel or doubled up and staying temporarily with others; (2) were financially disadvantaged, defined as currently paying more than 50% of gross income on rent, were in receipt of or eligible for social assistance, and had a gross income not exceeding 3.3 times the market rent of the unit for which the applicant was eligible; or (3) were at-risk of homelessness, defined as currently paying more than 50% of gross income on rent or under an eviction order or renting a hotel or motel room by the month. Applicants were excluded from consideration if they were not eligible for rent-geared-to-income assistance due to lack of legal residence status in Canada or were currently in rental arrears with another subsidized housing provider and an agreement to repay the arrears had not been entered into or honored.
A total of 166 applicants were eligible for this study, 112 (67%) of whom agreed to participate and underwent a baseline interview prior to being informed of the outcome of their housing application (accepted or wait-listed). Participants gave written informed consent and received a $20 honorarium for each completed interview. This study was approved by the St. Michael’s Hospital Research Ethics Board.
The baseline interviews were conducted between December 2005 and June 2007. Participants were re-interviewed approximately every 6 months after their move-in date (for individuals accepted into the housing program) or the date they received a notification letter that they had not been accepted into the housing program (for individuals who were wait-listed). Interviews took place at secure and private locations at community health centers, drop-in centers, homeless shelters, or the individual’s place of residence. Interviews were also conducted at correctional facilities and hospitals, if the individual was incarcerated or admitted to the hospital at the time of follow-up. When a participant moved outside of the city, interviews were conducted by telephone. Data for the 18-month follow-up period were collected between September 2006 and December 2008.
Measures
Physical and mental health status was assessed using the 36-item Short Form health survey (SF-36), which measures health status, physical functioning, role limitations due to physical and emotional problems, bodily pain, general health, vitality, social functioning, and mental health across eight domains.21 These domains were combined into two summary measures: the Physical Component Summary measure and the Mental Component Summary measure.22
Quality of life was assessed using two complementary instruments. The EuroQol (EQ-5D) is a standardized health-related quality of life instrument that generates a composite score reflecting the preference value associated with a given health state based on five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) as well as a global rating of current health using a visual analog scale ranging from 0–100.23–25 The Lehman Brief Quality of Life Interview (QOLI) is a broad-based instrument designed to assess the recent and current life circumstances of individuals in eight domains including living situation, daily activities and functioning, family relations, social relations, finances, work and school, legal and safety issues, and health.25 It also contains a global measure of life satisfaction.26 The subjective scale of the Brief QOLI was used to measure satisfaction across the eight domains.
Alcohol use was assessed using the Alcohol Use Disorders Identification Test (AUDIT), which is used to identify the preliminary signs of hazardous drinking and mild dependence.27,28 Participants reported how often they consumed alcohol and whether they had experienced negative events as a result of their drinking (e.g., memory loss, injuries). AUDIT scores of eight or more were considered indicative of hazardous or harmful alcohol use, as well as possible alcohol dependence.27 Drug abuse and the degree of problems related to drug use was assessed using the 20-item version of the Drug Abuse Screening Test (DAST-20).29 The DAST-20 provides a measure of some of the types of problems caused by drug use in the following areas: family relationships, social relationships, employment, legal, and physical symptoms and conditions.30 DAST-20 scores of 5 or higher were considered indicative of intermediate, substantial, or severe drug use problems.29
Health care utilization was assessed through self-report. Participants reported on hospitalizations, psychiatrist visits, emergency department visits, and visits with other non-psychiatrist health professionals, including general practitioners, nurses, optometrists, dentists, and other specialists, in the past 6 months.
Residential stability was measured using the Residential Timeline Follow-Back Calendar, a validated method that allows for the collection of detailed and accurate information on housing history.31 Participants’ pattern of residences, hospital or prison stays, and periods of homelessness were recorded for each 6-month period. Residential stability was defined as living in one’s own home or living with family or friends. Residential instability was defined as residing in jail, psychiatric hospital, drug treatment facility, or homeless shelters, or living in public places or on the street.
Data Analysis
Baseline characteristics for the 112 study participants were compared using Student’s t tests for continuous variables and chi-square tests or Fisher’s Exact tests (where appropriate) for categorical variables. Tests with p values less than 0.05 were considered statistically significant. All analyses were performed using SAS version 9.2 statistical software (SAS Institute, Cary, NC).
Repeated-measures analyses were restricted to the 89 participants who had data for all three follow-up interviews. Repeated-measures analysis of variance was used to assess between subject effects, within-subject effects, and group-by-time interactions during the 18-month follow-up period. Changes in health status, quality of life, substance use, health care utilization, and residential stability were assessed. Comparison groups were defined based on the group to which participants were initially assigned (intervention or usual care), regardless of whether they maintained their housing status or obtained other housing.
Results
Demographic Characteristics
Of the 112 participants, 46 (41%) received supportive housing and 66 (59%) were wait-listed for the program. Demographic characteristics at baseline are shown in Table 1. The final sample consisted of 81 (72%) men, 30 (27%) women, and one (1%) transgendered individual. The average age was 40.0 years (standard deviation = 11.5 years). Ninety-eight (88%) participants reported that they had previously been homeless, with the total amount of time spent homeless ranging from 1 day to 33 years. Of those who reported being homeless, the first episode of homelessness occurred on average at 28.5 years of age, and the average homeless episode was 4.5 years.
Table 1.
Demographic characteristics of Evangel Hall supportive housing study participants (n = 112) at baseline
| Variable | Intervention (n = 46) | Usual care (n = 66) | p Value |
|---|---|---|---|
| Sex, n (%) | 0.19 | ||
| Male | 30 (65) | 51 (77) | |
| Female | 15 (33) | 15 (23) | |
| Transgendered | 1 (2) | 0 (0) | |
| Age group, n (%) | 0.96 | ||
| 17–30 years | 9 (20) | 13 (20) | |
| 31–40 years | 15 (33) | 23 (35) | |
| 41–50 years | 11 (24) | 18 (27) | |
| 51–60 years | 10 (22) | 11 (17) | |
| ≥61 years | 1 (2) | 1 (2) | |
| Race/ethnicity, n (%) | 0.04 | ||
| White | 22 (48) | 29 (44) | |
| Black | 12 (26) | 6 (9) | |
| First Nations | 5 (11) | 16 (24) | |
| Mixed/other | 7 (15) | 15 (23) | |
| Marital status, n (%) | 0.76 | ||
| Single/never married | 30 (65) | 39 (59) | |
| Divorced/separated | 12 (26) | 19 (29) | |
| Widowed | 2 (4) | 2 (3) | |
| Married/partnered | 2 (4) | 6 (9) | |
| Canadian-born, n (%) | 31 (67) | 55 (83) | 0.05 |
| Education, n (%) | 0.51 | ||
| Some high school or less | 19 (41) | 34 (52) | |
| High school or equivalent | 10 (22) | 10 (15) | |
| Vocational training/college | 17 (37) | 22 (33) | |
| Currently enrolled in school, n (%) | 9 (20) | 6 (9) | 0.11 |
| Currently employed, n (%) | 11 (24) | 10 (15) | 0.24 |
| Previously homeless, n (%) | 40 (89) | 58 (89) | 0.95 |
| Lifetime duration of homelessness (years), mean (SD)a | 4.4 (7.3) | 4.6 (6.6) | 0.87 |
| Has a usual source of health care,bn (%) | 44 (98) | 57 (86) | 0.04 |
aAmong participants with a lifetime history of homelessness (n = 98)
bAmong participants with valid responses (n = 111); one participant reported “don’t know”
Follow-up Rates
The follow-up rates for the intervention and usual care groups respectively for each time period were 93% and 89% at 6 months, 93% and 83% at 12 months, and 85% and 76% at 18 months. There was no significant difference in the proportion of participants lost to follow-up between the intervention and usual care groups at 18 months (15% vs. 24%, χ2 = 1.35, df = 1, p = 0.24). Participants who were lost to follow-up did not significantly differ from participants who had data for all three follow-up interviews with respect to demographic characteristics, housing status, health status, quality of life, substance use, or health care utilization at baseline (data not shown).
Baseline Comparisons
There were significant differences between groups for baseline demographics, including race and country of birth (Table 1). Participants in the intervention group were more likely to report having a usual source of health care. The usual care group had significantly lower baseline scores for the EQ-5D Quality of Life health index as well as significantly higher baseline drug and alcohol use scores as measured by the AUDIT and DAST-20 (Table 2).
Table 2.
Health status, quality of life, substance use, and health care utilization for Evangel Hall supportive housing study participants (n = 112) at baseline
| Variable | Intervention (n = 46) | Usual care (n = 66) | p Value |
|---|---|---|---|
| Health status (SF-36), mean (SD) | |||
| Physical composite score | 46.9 (12.1) | 43.5 (12.9) | 0.16 |
| Mental composite score | 39.2 (11.4) | 41.1 (13.5) | 0.54 |
| Quality of Life (EQ-5D), mean (SD) | |||
| Health index | 0.8 (0.1) | 0.7 (0.2) | 0.01 |
| Quality of Life (Lehman), mean (SD) | |||
| General life satisfaction | 3.9 (1.4) | 4.1 (1.5) | 0.54 |
| Satisfaction with living situation | 2.7 (1.2) | 3.0 (1.5) | 0.32 |
| Satisfaction with daily activities | 4.1 (1.1) | 4.4 (1.3) | 0.35 |
| Satisfaction with family contacta | 4.7 (1.8) | 4.7 (1.6) | 0.96 |
| Satisfaction with social relations | 4.5 (1.3) | 4.7 (1.1) | 0.37 |
| Satisfaction with finances | 3.0 (1.5) | 2.6 (1.3) | 0.17 |
| Job satisfactionb | 3.9 (2.0) | 4.8 (1.4) | 0.23 |
| Satisfaction with safety | 4.2 (1.4) | 4.0 (1.8) | 0.58 |
| Satisfaction with health | 4.3 (1.3) | 4.1 (1.6) | 0.36 |
| Hazardous or harmful drinking in past 6 months, n (%) (AUDIT) | 13 (28) | 26 (39) | 0.22 |
| Alcohol use in past 6 months composite score (AUDIT), mean (SD) | 3.9 (5.7) | 9.0 (11.9) | <0.01 |
| Intermediate, substantial or severe drug use problems in past 6 months, n (%) (DAST-20) | 7 (15) | 13 (20) | 0.54 |
| Drug use in past 6 months composite score (DAST-20), mean (SD) | 1.4 (2.8) | 2.9 (4.4) | 0.03 |
| Health care utilization in past 6 months, n (%) | |||
| Any hospitalizations, overnight | 9 (20) | 12 (18) | 0.85 |
| Any emergency room visits | 18 (39) | 20 (30) | 0.33 |
| Any psychiatrist visits | 14 (30) | 14 (21) | 0.27 |
| Other health professional visitsc | 38 (83) | 56 (85) | 0.75 |
| Number of visits to health care sources in past 6 months, mean (SD) | |||
| Hospitalizations, overnight | 0.2 (0.5) | 0.2 (0.6) | 0.81 |
| Emergency room visits | 0.5 (0.6) | 0.5 (1.0) | 0.71 |
| Psychiatrist visits | 3.0 (8.1) | 1.0 (2.9) | 0.13 |
| Other health professional visitsc | 9.3 (13.4) | 10.8 (16.4) | 0.60 |
| Days spent in various residences in past 6 months, mean (SD) | |||
| Own place | 122.9 (76.6) | 89.5 (81.9) | 0.03 |
| Friends/family | 19.7 (48.6) | 23.4 (47.1) | 0.69 |
| Shelter | 27.1 (54.5) | 38.2 (64.9) | 0.34 |
| Drug treatment | 3.9 (26.5) | 7.2 (31.0) | 0.56 |
| Jail | 0.7 (4.3) | 1.8 (10.5) | 0.42 |
| Institution | 2.3 (9.8) | 0.8 (4.1) | 0.34 |
| Street | 3.4 (20.8) | 19.0 (44.8) | 0.02 |
| Days spent stably housed in past 6 months, mean (SD) | 142.6 (63.6) | 112.9 (78.2) | 0.04 |
aData only available for n = 48 participants who were in contact with their families (n = 19 in the intervention group and n = 29 in the usual care group)
bData only available for n = 21 participants who have jobs (n = 11 in the intervention group and n = 10 in the usual care group)
cIncludes general practitioners, neurologists, psychologists, dentists, audiologists, physical therapists, nurses, chiropractors, podiatrists, chiropodists, optometrists, and dieticians
Many participants were stably housed (either staying at their own place or with friends and family) prior to enrollment in the study, independent of their assignment to the intervention or usual care groups. At baseline, 36 (78%) participants in the intervention group and 45 (68%) in the usual care group were in stable housing (χ2 = 1.38, df = 1, p = 0.24).
Repeated-Measures Analysis
Repeated-measures analyses were restricted to the 89 (79%) participants who had data available for all three follow-up interviews. Repeated-measures analysis showed a significant improvement in the Lehman Brief Quality of Life satisfaction with living situation score in the intervention group compared with the usual care group (time, F3,3,261 = 47.68, p < 0.01; group × time, F3,3,261 = 14.60, p < 0.01; Table 3). Significant improvements over time were also observed for the Lehman Brief general life satisfaction score (F3,3,261 = 3.61, p = 0.02), satisfaction with finances score (F3,3,261 = 6.98, p < 0.01), and satisfaction with safety score (F13,3,261 = 14.03, p < 0.01); however, these improvements occurred independently of assigned housing group (Table 3). Repeated-measures analyses showed no significant within-subject effects for time or the group × time interaction with respect to SF-36 physical and mental health summary scores, EQ-5D Quality of Life scores, AUDIT alcohol use scores, DAST-20 drug use scores, or health care utilization (Table 3).
Table 3.
Repeated-measures analysis of variance (ANOVA) between and within-subject effects for group, time, and group × time interaction by assigned housing group for Evangel Hall supportive housing study participants with complete follow-up data (n = 89)
| Variablea | Mean score | ANOVA results | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6-Month follow-up | 12-Month follow-up | 18-Month follow-up | Group | Time | Group × time | ||||||||
| I | UC | I | UC | I | UC | I | UC | F | p Value | F | p Valueb | F | p Valueb | |
| Health status (SF-36) | ||||||||||||||
| Physical composite score | 46.1 | 42.7 | 46.2 | 43.6 | 46.1 | 42.4 | 46.0 | 42.6 | 2.14 | 0.15 | 0.17 | 0.90 | 0.11 | 0.94 |
| Mental composite score | 38.8 | 42.6 | 36.2 | 40.7 | 37.9 | 40.7 | 36.5 | 42.1 | 3.53 | 0.06 | 0.99 | 0.40 | 0.40 | 0.74 |
| Quality of Life (EQ-5D) | ||||||||||||||
| Health index | 0.8 | 0.8 | 0.8 | 0.8 | 0.8 | 0.7 | 0.8 | 0.8 | 1.69 | 0.20 | 0.71 | 0.54 | 0.04 | 0.99 |
| Quality of Life (Lehman) | ||||||||||||||
| General life satisfaction | 3.8 | 4.2 | 4.1 | 4.3 | 4.3 | 4.2 | 4.4 | 4.3 | 0.11 | 0.74 | 3.61 | 0.02 | 1.99 | 0.12 |
| Satisfaction with living situation | 2.6 | 3.1 | 5.4 | 3.6 | 5.2 | 4.0 | 5.0 | 4.1 | 15.24 | <0.01 | 47.68 | <0.01 | 14.60 | <0.01 |
| Satisfaction with daily activities | 4.0 | 4.5 | 4.3 | 4.2 | 4.5 | 4.2 | 4.4 | 4.4 | 0.00 | 1.00 | 0.35 | 0.78 | 2.90 | 0.04 |
| Satisfaction with family contactc | 4.6 | 4.9 | 4.7 | 5.6 | 5.2 | 5.4 | 5.1 | 5.3 | 1.59 | 0.22 | 1.32 | 0.27 | 0.76 | 0.49 |
| Satisfaction with social relations | 4.4 | 4.8 | 4.5 | 4.7 | 4.9 | 4.6 | 4.5 | 4.6 | 0.50 | 0.48 | 0.83 | 0.48 | 3.09 | 0.03 |
| Satisfaction with finances | 2.8 | 2.8 | 3.1 | 3.2 | 3.5 | 3.1 | 3.6 | 3.3 | 0.79 | 0.38 | 6.98 | <0.01 | 1.38 | 0.25 |
| Job satisfactiond | 3.6 | 5.0 | 3.7 | 6.0 | 3.1 | 5.7 | 2.9 | 4.7 | 1.26 | 0.38 | 3.89 | 0.17 | 1.34 | 0.37 |
| Satisfaction with safety | 4.1 | 4.1 | 5.0 | 4.5 | 5.2 | 4.6 | 5.0 | 4.6 | 2.23 | 0.14 | 14.03 | <0.01 | 1.72 | 0.17 |
| Satisfaction with health | 4.1 | 4.2 | 3.9 | 4.3 | 4.1 | 4.1 | 4.3 | 4.1 | 0.14 | 0.71 | 0.17 | 0.90 | 1.38 | 0.25 |
| Alcohol use in past 6 months composite score (AUDIT) | 4.2 | 9.5 | 7.1 | 8.5 | 5.7 | 8.8 | 5.9 | 9.4 | 2.58 | 0.11 | 0.63 | 0.58 | 2.07 | 0.11 |
| Drug use in past 6 months composite score (DAST-20) | 1.4 | 3.3 | 1.0 | 3.0 | 1.7 | 3.2 | 1.6 | 2.9 | 6.04 | 0.02 | 0.70 | 0.53 | 0.57 | 0.61 |
| Number of visits to health care sources in past 6 months | ||||||||||||||
| Hospitalizations, overnight | 0.2 | 0.2 | 0.2 | 0.4 | 0.2 | 0.4 | 0.2 | 0.3 | 1.03 | 0.31 | 0.40 | 0.74 | 0.71 | 0.54 |
| Emergency room visits | 0.4 | 0.5 | 0.4 | 0.7 | 0.6 | 0.6 | 0.6 | 0.4 | 0.07 | 0.79 | 0.61 | 0.58 | 1.09 | 0.35 |
| Psychiatrist visits | 2.9 | 1.0 | 2.1 | 1.1 | 1.4 | 0.6 | 1.8 | 1.4 | 2.09 | 0.15 | 1.27 | 0.29 | 0.73 | 0.51 |
| Other health professional visits | 10.7 | 11.5 | 6.7 | 6.9 | 11.1 | 7.0 | 6.6 | 8.9 | 0.01 | 0.92 | 1.15 | 0.32 | 0.63 | 0.56 |
| Days spent in various residences in past 6 months | ||||||||||||||
| Own place | 128.8 | 93.5 | 179.5 | 124.3 | 175.7 | 130.8 | 173.1 | 143.9 | 16.64 | <0.01 | 20.05 | <0.01 | 1.35 | 0.26 |
| Friends/family | 19.7 | 22.4 | 0.0 | 2.1 | 0.1 | 3.5 | 4.8 | 6.9 | 0.73 | 0.39 | 11.74 | <0.01 | 0.01 | 0.96 |
| Shelter | 19.7 | 37.6 | 0.1 | 15.0 | 0.8 | 23.7 | 0.0 | 14.6 | 5.67 | 0.02 | 10.86 | <0.01 | 0.40 | 0.68 |
| Drug treatment | 4.6 | 3.2 | 0.3 | 0.3 | 1.1 | 0.0 | 1.2 | 1.3 | 0.12 | 0.73 | 1.55 | 0.22 | 0.08 | 0.79 |
| Jail | 0.8 | 1.6 | 0.0 | 3.4 | 0.0 | 4.7 | 0.4 | 2.2 | 2.30 | 0.13 | 0.23 | 0.77 | 0.63 | 0.52 |
| Institution | 5.0 | 5.0 | 0.0 | 1.9 | 0.8 | 4.1 | 0.4 | 2.3 | 0.90 | 0.34 | 7.29 | <0.01 | 1.01 | 0.33 |
| Street | 4.0 | 21.2 | 0.0 | 32.9 | 1.5 | 13.3 | 0.0 | 8.8 | 7.71 | <0.01 | 3.80 | 0.02 | 3.79 | 0.02 |
| Days spent stably housed in past 6 months | 148.5 | 115.9 | 179.6 | 126.4 | 175.8 | 134.3 | 178.0 | 150.8 | 15.65 | <0.01 | 9.96 | <0.01 | 1.74 | 0.17 |
I intervention, UC usual care
aExcludes participants with missing data for at least one follow-up interview (n = 23)
bGreenhouse–Geisser correction applied to adjust p value in instances where sphericity assumption was violated
cData only available for n = 30 participants who were in contact with their families
dData only available for n = 4 participants who had a job
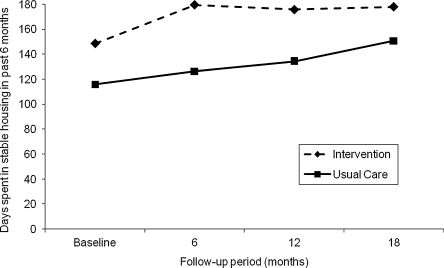
In terms of residential stability, significant within-subject effects for time were observed for the number of days spent in the participant’s own place (F3,3,261 = 20.05, p < 0.01), staying with friends or family (F3,3,261 = 11.74, p < 0.01), in a shelter (F3,3,261 = 10.86, p < 0.01), in an institution (F3,3,261 = 7.29, p < 0.01), and on the street (F3,3,261 = 3.80, p = 0.02) in the past six months (Table 3). There was also a significant within-subject group × time interaction effect for the number of days spent on the street in the past six months (F3,3,261 = 3.79, p = 0.02). During the study period, the number of days spent in stable housing significantly increased (F3,3,261 = 9.96, p < 0.01), and participants in the intervention group spent significantly more days in stable housing in the past six months (F1,87 = 15.65, p < 0.01; Figure 1). However, the improvement in residential stability over time did not differ between groups, as the test for the within-subject group × time interaction effect was not significant (F3,3,261 = 1.74, p = 0.17; Table 3).
Figure 1.
Change in days spent in stable housing in the past 6 months from baseline to 18-month follow-up among Evangel Hall supportive housing study participants with complete follow-up data (n = 89; excludes participants with missing data for at least one follow-up interview).
Discussion
Our results show that individuals accepted into a supportive housing program had significant improvements over time in only one dimension of quality of life, their satisfaction with living situation, in comparison to participants who were wait-listed for the program. We did not observe any significant improvements in other aspects of quality of life or health status, nor did we observe any decreases in substance use or health care utilization that could be attributed to the supportive housing program. Participants in the intervention group spent consistently more days in stable housing in the past 6 months compared with the usual care group, and significant improvements in residential stability were observed in both groups over the follow-up period. However, the change in residential stability over time was not significantly different between the two groups, and the majority of participants, regardless of their study assignment, acquired stable housing at some point during the 18-month follow-up. Only five participants remained homeless throughout the study period.
Our study made use of a natural experiment at a community-based agency that was providing housing to homeless and marginally housed individuals. Consequently, we had no control over how the intervention was implemented. Our baseline data suggests that individuals who were accepted into the program had lower composite scores for drug and alcohol use and had spent fewer nights living on the streets in the past 6 months. As indicated by these differences between groups at baseline, the assignment of participants to the intervention or usual care groups was not random and may suggest a tendency for the program to accept individuals who were less active substance users and who may have been considered more likely to be successful residents in the program. A central value espoused by supported housing programs such as Pathways to Housing is to target these “hardest to house” individuals.32 However, as our findings show, supportive housing programs may not always admit those individuals who are considered the “hardest to house,” such as those who are chronically homeless and/or dually diagnosed with substance abuse and psychiatric problems. Furthermore, supportive housing programs may preferentially select applicants who are considered to have higher social functioning, as these applicants may be perceived as being better able to adapt to and function within a cooperative housing community.
Prior research involving homeless and vulnerably housed adults have shown improvements in residential stability and decreases in health care utilization resulting from implementation of supportive housing programs. Culhane et al. (2002), in their study of homeless persons with severe mental disabilities in New York, found significant reductions in shelter use and health care utilization following the introduction of a supportive housing program.14 Martinez and Burt (2006) observed significant improvements in residential stability and significant reductions in emergency department visits and inpatient services following the introduction of permanent supportive housing for homeless individuals in San Francisco with psychiatric illness, substance use disorders, and other disabilities.15 Similarly, Clark and Rich (2003), Drake et al. (1997), and Lipton et al. (1988) all observed improvements in housing outcomes among homeless individuals with mental illnesses and/or substance use disorders who were provided with subsidized housing and intensive case management in comparison to those receiving intensive case management alone or usual care, especially among individuals with high psychiatric symptom severity and high substance use.16–18
The effects of supportive housing on substance use are less clear. Drake et al. (1997) observed modest, yet significant, decreases in alcohol and drug use after 18 months of follow-up among participants who were placed in housing.18 In their study of homeless veterans with substance use and/or psychiatric disorders, Clark and Rich (2003) found decreased substance use over a 12-month period, but no differences in level of improvement were found when comparing a comprehensive supportive housing program that included case management to case management alone.16
In contrast to the previous literature, we observed no significant differences in health status, substance use, health care utilization, or residential stability between the two groups over time resulting from our supportive housing program. A number of factors may explain our findings. First, an unexpectedly large proportion of participants who applied to the supportive housing program were already living in stable housing prior to enrollment. As a result, this study had a reduced ability to assess the effects of a transition from homelessness to stable housing on the outcomes of interest.
Second, the power of this study to detect differences between the two groups was limited by a relatively small sample size. Supportive housing programs are often constrained by funding and resource availability, as the costs of housing subsidies and support services are often prohibitively high. The program studied here provided 66 newly built units for single adults; our sample of eligible applicants was limited to 166 individuals, of whom only 112 consented to participate. Studies of larger-scale interventions are preferable because they provide greater power, but such research opportunities are relatively rare.
Third, many individuals in the usual care group obtained stable housing during the follow-up period through means other than the supportive housing program under study. Of note, our findings are similar to that of a study conducted in San Francisco that did not demonstrate a difference in utilization patterns between intervention and control groups among applicants to a supportive housing program.31 Kessell et al. (2006) compared health care utilization between applicants who were placed in supportive housing and those who were wait-listed for the program and found high rates of acute and ambulatory health services utilization in both groups.31 In both the present study and the Kessell study, a substantial proportion of individuals in the usual care group obtained housing during the follow-up period. Similarly, in a recent study comparing homeless and unstably housed persons living with HIV/AIDS who were randomized to either rental assistance or customary care, the limited ability to detect meaningful between-group changes over time using intent-to-treat analyses was attributed to the attainment of stable housing among participants.33 For their study, Wolitski et al. (2010) observed that 51% of participants in the comparison condition obtained stable housing during the 18-month follow-up period.33
Finally, we used self-report to assess hospitalizations, emergency room visits, psychiatric visits, and non-psychiatric medical professional visits. In contrast, other studies have used administrative databases to obtain health care utilization data for their participants. Self-reported health care use can be inaccurate among homeless populations, which may have contributed to the lack of observable differences between groups, especially if accuracy in reporting differed by group.34,35 Additionally, these studies were all conducted in the United States, where lack of health insurance is a major financial barrier to care.19 Because our study was conducted in a country with a system of universal health insurance, health care utilization rates may be less impacted by the provision of supportive housing.1
Despite the lack of observable difference in residential stability between groups, it is encouraging that study participants achieved extremely high rates of retention in stable housing and demonstrated significant increases in the number of days spent in stable housing over time. Over 95% of participants in the intervention group maintained their housing during the study period. Only two participants in the intervention group became homeless again at some point during the study period. Additionally, almost 90% of participants in the wait-listed group were in stable housing at the end of the study period.
Follow-up rates for our study were relatively high, especially considering the often transient and hard-to-reach nature of this population. Over 90% of participants completed at least one follow-up interview and 80% completed all three. Attrition was minimized by a number of strategies. At the time of each interview, participants were asked to provide contact information of friends, relatives, service providers, and case workers who were most likely to know their whereabouts and who could be contacted in order to locate them. Regular in-person or telephone contacts and letters were used throughout the study period to determine the participant’s whereabouts, update their contact information, and remind them of their next follow-up interview. Participants receiving social assistance also gave consent for the research team to contact social services to obtain information on their current mailing address and phone number over the study period.
Conclusions
Our results show that residential stability can be maintained at high rates among individuals who are homeless or vulnerably housed, even if poor physical and mental health status and substance use issues are present. Further research is needed to determine the impact of supportive housing programs on health care utilization and substance use among these highly disadvantaged populations within a system of universal health insurance coverage. The ability to detect any such effects will be substantially reduced if the housing program under study accepts a large proportion of vulnerably housed rather than homeless individuals or if a large proportion of individuals in the usual care group are able to obtain housing independent of the housing program.
Acknowledgements
Dr. Hwang is the recipient of a New Investigator Award from the Canadian Institutes of Health Research. The Centre for Research on Inner City Health is supported in part by a grant from the Ontario Ministry of Health and Long-Term Care. We wish to thank Joseph Taylor, Marcela Fresolone, and all the staff at Evangel Hall Mission for collaborating on this project and for their assistance in participant recruitment and follow-up. We also wish to thank the shelter, drop-in, and municipal and provincial staff who also assisted in participant follow-up. This project was supported by an Advanced Grant from the Wellesley Institute and by an Interdisciplinary Capacity Enhancement Grant on Homelessness, Housing, and Health from the Canadian Institutes of Health Research. The authors wish to thank Marko Katic (Department of Research Design and Biostatistics, Sunnybrook Health Sciences Centre) for his help with programming and data analyses.
References
- 1.Barrow SM, Herman DB, Cordova P, Struening EL. Mortality among homeless shelter residents in New York City. Am J Public Health. 1999;89:529–534. doi: 10.2105/AJPH.89.4.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheung AM, Hwang SW. Risk of death among homeless women: a cohort study and review of the literature. CMAJ. 2004;170:1243–1247. doi: 10.1503/cmaj.1031167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hwang SW. Mortality among men using homeless shelters in Toronto, Ontario. JAMA. 2000;283:2152–2157. doi: 10.1001/jama.283.16.2152. [DOI] [PubMed] [Google Scholar]
- 4.Hwang SW, Wilkins R, Tjepkema M, O'Campo PJ, Dunn JR. Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. BMJ. 2009;339:b4036. doi: 10.1136/bmj.b4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kasprow WJ, Rosenheck R. Mortality among homeless and nonhomeless mentally ill veterans. J Nerv Ment Dis. 2000;188:141–147. doi: 10.1097/00005053-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Goering P, Tolomiczenko G, Sheldon T, Boydell K, Wasylenki D. Characteristics of persons who are homeless for the first time. Psychiatr Serv. 2002;53:1472–1474. doi: 10.1176/appi.ps.53.11.1472. [DOI] [PubMed] [Google Scholar]
- 7.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273. [PMC free article] [PubMed] [Google Scholar]
- 8.Stark LR. Barriers to health care for homeless people. In: Jahiel RI, editor. Homelessness: A Prevention-Oriented Approach. Baltimore, MD: Johns Hopkins University Press; 1992. pp. 151–164. [Google Scholar]
- 9.Dorvil H, Morin P, Beaulieu A, Robert D. Housing as a social integration factor for people classified as mentally ill. House Studies. 2005;20:497–519. doi: 10.1080/02673030500062525. [DOI] [Google Scholar]
- 10.Goering P, Boydell K, Butterill D, Cochrane J, Durbin J, Rogers J, et al. Review of best practices in mental health reform. Ottawa, ON: Health Canada; 1997. [Google Scholar]
- 11.Parkinson S, Nelson G, Horgan S. From housing to homes: a review of the literature on housing approaches for psychiatric consumer/survivors. Can J Community Ment Health. 1999;18:145–164. doi: 10.7870/cjcmh-1999-0008. [DOI] [PubMed] [Google Scholar]
- 12.Ridgway P, Zipple AM. The paradigm shift in residential services: from the linear continuum to supported housing approaches. Psychosoc Rehabil J. 1990;13:11–31. [Google Scholar]
- 13.Sylvestre J, Nelson G, Sabloff A, Peddle S. Housing for people with serious mental illness: a comparison of values and research. Am J Community Psychol. 2007;40:125–137. doi: 10.1007/s10464-007-9129-9. [DOI] [PubMed] [Google Scholar]
- 14.Culhane DP, Metraux S, Hadley T. Public service reductions associated with placement of homeless persons with severe mental illness in supportive housing. Hous Policy Debate. 2002;13:107–164. doi: 10.1080/10511482.2002.9521437. [DOI] [Google Scholar]
- 15.Martinez TE, Burt MR. Impact of permanent supportive housing on the use of acute care health services by homeless adults. Psychiatr Serv. 2006;57:992–999. doi: 10.1176/appi.ps.57.7.992. [DOI] [PubMed] [Google Scholar]
- 16.Clark C, Rich AR. Outcomes of homeless adults with mental illness in a housing program and in case management only. Psychiatr Serv. 2003;54:78–83. doi: 10.1176/appi.ps.54.1.78. [DOI] [PubMed] [Google Scholar]
- 17.Lipton FR, Nutt S, Sabatini A. Housing the homeless mentally ill: a longitudinal study of a treatment approach. Hosp Community Psychiatry. 1988;39:40–45. doi: 10.1176/ps.39.1.40. [DOI] [PubMed] [Google Scholar]
- 18.Drake RE, Yovetich NA, Bebout RR, Harris M, McHugo GJ. Integrated treatment for dually diagnosed homeless adults. J Nerv Ment Dis. 1997;185:305. doi: 10.1097/00005053-199705000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285:200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 20.Frankish CJ, Hwang SW, Quantz D. Homelessness and health in Canada. Can J Public Health. 2005;96:23–29. doi: 10.1007/BF03403700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Ware JE, Kosinski M, Keller D. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2. Boston, MA: The Health Institute, New England Medical Center; 1995. [Google Scholar]
- 23.Krabbe P, Weijnen T. Guidelines for analyzing and reporting EQ-5D outcomes. In: Brooks R, Rabin R, Charro F, editors. The Measurement and Valuation of Health Status Using EQ-5D: A European Perspective. Boston, MA: Kluwer Academic Press; 2003. [Google Scholar]
- 24.Rabin R, Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 25.Lehman AF. A quality of life interview for the chronically mentally ill. Eval Program Plann. 1988;11:51–62. doi: 10.1016/0149-7189(88)90033-X. [DOI] [Google Scholar]
- 26.Lehman AF, Dixon L, Hoch JS, Deforge B, Kernan E, Frank R. Cost-effectiveness of assertive community treatment for homeless persons with severe mental illness. Br J Psychiatry. 1999;174:346–352. doi: 10.1192/bjp.174.4.346. [DOI] [PubMed] [Google Scholar]
- 27.Babor TF, Higgins-Biddle JC, Saunders JB. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines For Use in Primary Care. Geneva: World Health Organization, Department of Mental Health and Substance Dependence; 2001. [Google Scholar]
- 28.Piccinelli M, Tessari E, Bortolomasi M, et al. Efficacy of the alcohol use disorders identification test as a screening tool for hazardous alcohol intake and related disorders in primary care: a validity study. BMJ. 1997;314:420–424. doi: 10.1136/bmj.314.7078.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gavin DR, Ross HE, Skinner HA. Diagnostic validity of the drug abuse screening test in the assessment of DSM-III drug disorders. Br J Addict. 1989;84:301–307. doi: 10.1111/j.1360-0443.1989.tb03463.x. [DOI] [PubMed] [Google Scholar]
- 30.Detailed review of the drug abuse screening test (DAST). In: Directory of Client Outcome Measures for Addiction Treatment Programs. Ontario, Canada: Addiction Research Foundation; 1993.
- 31.Kessell ER, Bhatia R, Bamberger JD, Kushel MB. Public health care utilization in a cohort of homeless adult applicants to a supportive housing program. J Urban Health. 2006;83:860–873. doi: 10.1007/s11524-006-9083-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94:651–656. doi: 10.2105/AJPH.94.4.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wolitski RJ, Kidder DP, Pals SL, et al. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14:493–503. doi: 10.1007/s10461-009-9643-x. [DOI] [PubMed] [Google Scholar]
- 34.Calsyn RJ, Morse GA, Klinkenberg WD, Trusty ML. Reliability and validity of self-report data of homeless mentally ill individuals. Eval Program Plann. 1997;20:47–54. doi: 10.1016/S0149-7189(96)00035-3. [DOI] [Google Scholar]
- 35.Kee R, Sadowski L, Buchanan D, Garcia D. Validity of self-reported health service utilization data in the homeless. 135th APHA Annual Meeting & Exposition; 2007 November 3–7; Washington, DC. Washington, DC: American Public Health Association; 2007. [Google Scholar]