Abstract
Laminoplasty for thoracic and lumbar spine surgery enables surgeons to preserve the posterior arch of the spine while preventing invasion of hematoma and scar tissue, postoperative instability, subluxation, and kyphotic deformities. The authors have developed a new surgical technique: namely, transverse placement laminoplasty (TPL) using titanium miniplates. Eight patients and 18 laminae underwent TPL using a titanium mini-plate. The preoperative diagnoses were six intradural tumors, one ossification of a yellow ligament and one spontaneous spinal cord herniation. The mean blood loss was 219 g and the mean duration of surgery was 3 h and 54 min. The mean postoperative follow-up period was 2 years and 1 month. All eight patients started to sit with a soft brace within the second postoperative day, and were able to walk within the fifth postoperative day. There were no cases of spinal deformity, an invasion of hematoma or scar tissue into the spinal canal on magnetic resonance imaging, or back pain. TPL simultaneously enables surgeons to obtain sufficient field of vision and rigid early fixation of the reduced lamina at the time of surgery. Moreover, our novel technique also simplifies the postoperative treatment, while preserving the posterior arch of the spine, and also preventing an invasion of a hematoma and scar tissue, postoperative instability, subluxation, and kyphotic deformities.
Keywords: Laminoplasty, Thoracic and lumbar lesion, Intradural tumor
Introduction
The most common procedure for exposing the spinal canal for surgery on the spinal cord and for treating cauda equina tumors in the thoracic and lumbar spine has been a laminectomy [8], and no reconstruction of the excised laminae has typically been done. Even if a laminectomy provides a sufficient operative exposure for the safe extirpation of a spinal tumor, several difficulties still exist, including an invasion of the hematoma and scar tissue into the spinal canal [4, 6, 10, 13] (Fig. 1), postoperative instability, subluxation or a kyphotic deformity of the spine, especially in pediatric patients [2, 3, 7, 16, 17]. Recently, several investigators have reported the usefulness of laminoplasty to reconstruct the excised laminae for the extirpation of spinal cord and cauda equina tumors [9, 14, 15]. Laminoplasty allows surgeons to compensate for several difficulties encountered during a laminectomy. The authors have developed a new surgical technique: namely transverse placement laminoplasty (TPL) using a titanium mini-plate for surgery on the spinal cord and cauda equina tumors in the thoracic and lumbar spine. In addition, this method has also been applied for other kind of spinal disorders. The purpose of the current study is to introduce this new surgical technique and to evaluate the efficacy for reconstructing of the laminae in thoracic and lumbar lesion.
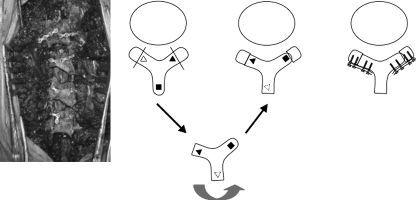
Fig. 1.
A 54-year-old woman. Invasion of hematoma and scar tissue into the spinal canal after laminectomy for expiration of spinal tumour. a Pre-operative MRI showed intradural spinal tumour at the level of the ninth thoracic spine. b Laminectomy from T8 to T10 and tumour extirpation was performed for neurolemoma. Post-operative MRI showed that spinal cord was comprised by hematoma. c Three months after the operation, MRI revealed that hematoma had almost disappeared from the spinal canal
Materials and methods
Five male and three female patients underwent a TPL using titanium miniplates, and the patients ranged from 45 to 78 years old (mean 60 years old). The preoperative diagnoses were six intradural tumors, one ossification of a yellow ligament and one spontaneous spinal cord herniation. The affected spine included the thoracic spine in six and the lumbar spine in two (Table 1).
Table 1.
Transverse placement laminoplasty (TPL) using a titanium mini-plate
| Patient no. | Sex (M/F) | Age at surgery (years) | Follow-up (months) | Affected spine | Number of reconstructed laminae | Operation time (min) | Blood loss (g) | Postoperative orthosis | Final diagnosis |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 47 | 40 | T11–12 | 4 | 380 | 600 | Soft brace | Neuroemema |
| 2 | M | 69 | 32 | T12 | 1 | 205 | 45 | Soft brace | Neuroemema |
| 3 | M | 75 | 33 | T7–8 | 2 | 225 | 300 | Soft brace | Hemangiema |
| 4 | M | 64 | 34 | T10–12 | 3 | 220 | 180 | Soft brace | OYLa |
| 5 | M | 55 | 17 | L1–2 | 1 | 170 | 50 | Soft brace | Neuroemema |
| 6 | F | 48 | 12 | T11–12 | 2 | 195 | 210 | Soft brace | Neuroemema |
| 7 | F | 45 | 12 | T3–5 | 3 | 245 | 220 | Bust band | SSCHb |
| 8 | F | 78 | 13 | L1–2 | 2 | 230 | 145 | Soft brace | Neuroemema |
aOssification of yellow ligament
bSpontaneous spinal cord hemiation
TPL using a titanium mini-plate Fig. 2
Fig. 2.
Transverse placement laminoplasty (TPL)
After exposing the affected laminae, two bony gutters at each lamina are drilled for the removal of the laminae by one piece. Both gutters should be positioned at the midpoint where the vertebral arch curve to form the facet joint. When two bony gutters reach the spinal canal, laminae connected with spinous process are removed in one piece. Thus, surgeons can obtain a sufficient field of vision to perform the intra canal procedure. However, bony cutting loss from 3 to 4 mm in width is occurred in both sides of lamina. After finishing the surgical procedures of the intra canal of the spine, the excised laminae connected with spinous process were rotated transversely by 90°, restored on the spinal canal, and then were fixed by a titanium miniplates and screws (Würzburg® Titanium miniplate system. Germany). Early rigid fixation is usually obtained by using six to eight screws length ranging from 5 to 7 mm in length and two miniplates for each lamina.
Postoperative radiographic evaluation
A plain X-ray was performed for in each patient periodically after the surgery, and the surgeon checked the position of the screws and plates. Computed-tomography was performed at 2 months after surgery, and both examinations were continued every month until bony fusion was recognized. When a callus formation of the reconstructed laminae was found and no displacement of the screws and plates was found, the surgeon decided that bony fusion had been achieved. At the latest follow-up, we examined the neurological findings, the presence of back pain, and checked the location of the plates, sublaxation and the instability of the affected spine by the X-rays, and checked for any scar tissue invasion in the spinal canal or a recurrence of the tumor based on the magnetic resonance imaging (MRI) findings and according to the patients’ statements and the follow-up periods. In six of eight cases in the current study whose affected spine demonstrated thoracic and thoracolumbar lesion, postoperative kyphotic deformities were evaluated using the changes of the Cobb angle in lateral plain X-rays at the time of pre-operative and final follow-up periods, and compared with the control group (N = 6), who were diagnosed to have neurilemoma in thoracic and thoracolumbar lesions and therefore underwent a laminectomy in our hospital. MRI examinations were performed at 2 months, 6 months, 1 year after the operation. During the final follow-up periods, the surgeons checked for the presence of invasion of hematoma and scar tissue. Mann–Whitney’s U Test was performed for statistical analyses. Values of P < 0.05 were considered to be statistically significant.
Results
Eight patients and 18 laminae were performed using TPL. Mean blood loss was 219 g (range 45–600 g), and the mean duration of surgery was 3 h 54 min (range 2 h 50 min–6 h 20 min). The postoperative follow-up period ranged from 12 to 40 months (mean 2 years and 1 month). All eight patients started to sit with a soft brace within the second postoperative day, and were able to walk within the fifth postoperative day. Bony fusion of reconstructed laminae was recognized at a mean of 3.2 months. All patients were allowed to remove the soft brace when the bony fusion of the laminae was recognized. No displacement of restored laminae and titanium mini-plates were seen in any patient’s roentgenogram at the final follow-up periods. Moreover, there were no cases of invasion of hematoma or scar tissue on the spinal canal on MRI and instability or sublaxation of affected spine on X-rays. In addition, no instances of back pain were observed. In six cases whose affected laminae were thoracic lesions and therefore they were treated by TPL methods, the preoperative mean Cobb angle was 13.2° ± 4.7°, while the final mean Cobb angle was 14.0° ± 5.1°. Otherwise, in the control group, the preoperative mean Cobb angle was 12.3° ± 2.8° preoperatively and final mean cobb angle increased to 22.0° ± 6.5° (P = 0.0045) (Table 2).
Table 2.
Kyphotic deformities in lateral plain X-rays
| Patient no. | Age at surgery (years) | Follow-up (months) | Affected spine | Cobb angle (°) | |
|---|---|---|---|---|---|
| Prop. | Most recent follow-up | ||||
| TPL group | |||||
| 1 | 47 | 40 | T11–12 | 18 | 20 |
| 2 | 69 | 32 | T12 | 6 | 7 |
| 3 | 75 | 33 | T7–8 | 12 | 12 |
| 4 | 64 | 34 | T10–12 | 16 | 17 |
| 6 | 48 | 12 | T11–12 | 10 | 10 |
| 7 | 45 | 12 | T3–5 | 17 | 18 |
| Control group | |||||
| 1 | 8 | 84 | T3–5 | 10 | 21 |
| 2 | 54 | 24 | T9–10 | 15 | 28 |
| 3 | 67 | 60 | T12 | 11 | 19 |
| 4 | 63 | 22 | T12–L1 | 9 | 11 |
| 6 | 30 | 12 | T3–5 | 13 | 26 |
| 7 | 63 | 36 | T12 | 16 | 27 |
Case reports
Case 1. A 47-year-old man had a 6 months history of lower back pain and a 2 months history of progressive numbness and spasticity in both legs. MRI of his thoraco-lumbar lesion revealed a huge intradural spinal tumor ranging widely from the ninth thoracic spine to the second lumbar spine (Fig. 3a). The laminae from the ninth thoracic spine to the second lumbar spine were cut using a surgical drill. After removing the spinal tumor, the excised four laminae were rotated transversely, restored on the spinal canal, and then were fixed by titanium miniplates (Fig. 3b). Due to the initial rigid fixation of the reconstructed laminae, he was allowed to walk, wearing a soft brace, on the fifth postoperative day. The post-operative diagnosis was neurilemoma. Post-operative MRI of his thoracic lumbar lesion showed no canal compromise caused by either a hematoma or any other suspicious findings, and bony fusion of the excised laminae was recognized at 3 months after surgery (Fig. 4a–d).
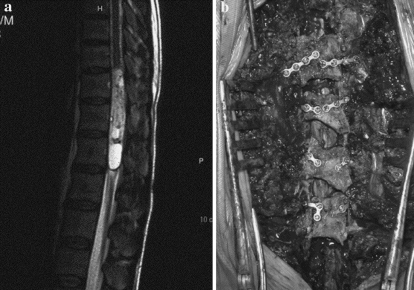
Fig. 3.
Case 1. A 47-year-old man. a magnetic resonance imaging (MRI) of his thoraco-lumbar lesion revealed huge intradural spinal tumour ranging widely from the ninth thoracic spine to the second lumbar spine. b After removing the spinal tumour, the excised four laminae were rotated transversely, restored on the spinal canal, and then were fixed by titanium manipulates
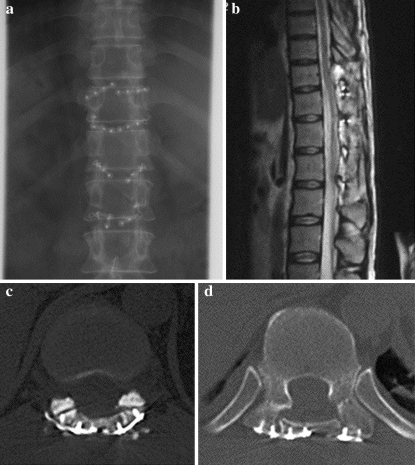
Fig. 4.
Case 1. A 47-year-old man. a Postoperative roentgenogram of the transverse placement method using titanium miniplates. b Postoperative MRI at 2 months after the operation. c, d Postoperative computed tomography showing bony fusion of excised laminae was recognized at 3 months after surgery
Case 7. A 45-year-old woman had a 6-month history of progressive pain and numbness in her right leg. Myelography and computed tomography after myelography showed a huge tumor at the anterior of the conus medullaris and the cauda equina at the level of the 11th and 12th thoracic spine. The eleventh and twelfth laminae were cut using a surgical drill. After removing the spinal tumor, the excised two laminae were rotated transversely, restored on the spinal canal, and then were fixed by a titanium mini-plate. The post-operative diagnosis was neurilemoma. She was allowed to walk on the fourth postoperative day. Bony fusion of the excised laminae was recognized at 3 months after surgery (Fig. 5a–c).
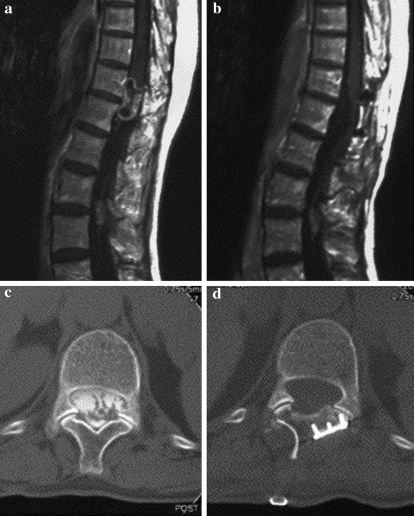
Fig. 5.
Case 7. A 45-year-old woman. a magnetic resonance imaging (MRI) revealed a huge intradural spinal tumour. b Preoperative computed tomography. c Postoperative MRI at 12 months after the operation. c, d Postoperative computed tomography showing wide spinal canal and rigid early fixation of reduced lamina
Discussion
Various kinds of laminoplasty have been reported for thoracic and lumbar spine spinal cord and cauda equina tumors. Laminoplasty using a thread wire saw [5] enables the restoration of the excised laminae precisely because the gap at the cut end of the laminae is very thin. On the other hand, this procedure presents several problems: for example, nerve injury may occur if the thread wire saw passes beneath the laminae; operative exposure may not be sufficient because the cut end of the opened spinal canal becomes conical; and/or rigid fixation is not initially obtained. In our hospital, the patients who underwent recapping T saw laminoplasty had to have a solid brace applied until bony fusion was recognized because rigid fixation was not initially obtained. Laminoplasty using a surgical drill or chisel enables operative exposure sufficient to extirpate the spinal tumor safely. On the other hand, it is difficult to restore the excised laminae precisely because the gap at the cut end of the laminae is wide. 90° rotation laminoplasty reported by Murakami et al. [11] and Asazuma et al. [1] enabled a sufficient operative exposure to extirpate the spinal tumor safely and maintain the expanded spinal canal, though the initial fixation of the restored laminae was not so rigid. On the other hand, since 1996, several authors have reported the application of a titanium mini-plate for spinal surgery [12, 18]. We developed a new surgical technique for the thoracic and lumbar spine in the spinal cord and cauda equina tumors which utilize a combination of 90° rotation laminoplasty and a titanium mini-plate TPL. In the current study, there were no cases of neurological deterioration postoperatively. Furthermore, regarding the rigid early fixation of the reduced lamina, all patients were able to obtain rigid bony fixation with a simple soft brace. Postoperative kyphotic deformities of the affected spine in the TPL group were significantly lower than in the control group who underwent a laminectomy in our hospital.
Our novel technique simultaneously enables surgeons to obtain a sufficient field of vision and rigid early fixation of reduced lamina at the time of surgery, moreover TPL also helps to simplify the postoperative treatment, preserve posterior arch of the spine, and prevents the invasion of hematoma and scar tissue, postoperative instability, subluxation, and kyphotic deformities.
Conclusions
Transverse placement laminoplasty simultaneously enables surgeons to obtain a sufficient field of vision and rigid early fixation of the reduced lamina at the time of surgery. Furthermore, TPL also helps to simplify the postoperative treatment, preserve the posterior arch of the spine, and prevents the invasion of hematoma and scar tissue, postoperative instability, subluxation, and kyphotic deformities.
References
- 1.Asazuma T, Yamagishi M, Sato M, Ichimura S, Fujikawa K. Vertebral arch reconstruction on 90-degree rotational laminoplasty after removal of spinal cord and cauda equina tumors. Acta Neurochir (Wien) 2003;145:495–500. doi: 10.1007/s00701-003-0028-z. [DOI] [PubMed] [Google Scholar]
- 2.Epstein F, Epstein N. Surgical treatment of spinal cord astrocytoma of childhood: a series of 19 patients. J Neurosurg. 1982;57:685–689. doi: 10.3171/jns.1982.57.5.0685. [DOI] [PubMed] [Google Scholar]
- 3.Iida Y, Kataoka O, Sho T, et al. Postoperative lumbar spinal instability occurring or progressing secondary to laminectomy. Spine. 1990;15:1186–1189. doi: 10.1097/00007632-199011010-00018. [DOI] [PubMed] [Google Scholar]
- 4.Jacobs RR, McClain O, Neff J. Control of postlaminectomy scar formation. Spine. 1980;5:223–229. doi: 10.1097/00007632-198005000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Kawahara N, Tomita K, Shinya Y, et al. Recapping T-saw laminoplasty for spinal cord tumors. Spine. 1977;24:1363–1370. doi: 10.1097/00007632-199907010-00015. [DOI] [PubMed] [Google Scholar]
- 6.LaRocca H, Macnab The laminectomy membrane. J Bone Joint Surg [Br] 1974;56:545–550. [PubMed] [Google Scholar]
- 7.Lonstein JE. Postoperative kyphosis. Clin Orthop. 1977;128:93–100. [PubMed] [Google Scholar]
- 8.Love JG. Neurosurgical techniques: laminectomy for removal of spinal cord tumors. J Neurosurg. 1966;25:116–121. doi: 10.3171/jns.1966.25.1.0116. [DOI] [PubMed] [Google Scholar]
- 9.Matsui H, Kanamori M, Miaki K. Expansive laminoplasty for lumbar intra dural lipoma. Int Orthop. 1997;21(3):185–187. doi: 10.1007/s002640050147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayfield FH. Complications of laminectomy. Clin Neurosurg. 1976;23:435–436. doi: 10.1093/neurosurgery/23.cn_suppl_1.435. [DOI] [PubMed] [Google Scholar]
- 11.Murakami H, Mamune N, Isaki H, et al. A case report of giant cauda equina tumor with minor symptoms [(in Japanese)] Spine Spinal Cord. 1998;11:53–56. [Google Scholar]
- 12.O’Brien M, Peterson D, Casey TH, et al. A novel technique for laminoplasty augmentation of spinal canal area using titanium mini-plate stabilization. Spine. 1996;4:474–484. doi: 10.1097/00007632-199602150-00012. [DOI] [PubMed] [Google Scholar]
- 13.Pear BL. Spinal epidural hematoma. Am J Roentgenol. 1972;115:155–164. doi: 10.2214/ajr.115.1.155. [DOI] [PubMed] [Google Scholar]
- 14.Raimondi AJ, Gutierrez FA, Di Rocco C. Laminotomy and total reconstruction of the posterior arch for spinal canal surgery in childhood. J Neurosurg. 1976;45:550–560. doi: 10.3171/jns.1976.45.5.0555. [DOI] [PubMed] [Google Scholar]
- 15.Shikata J, Yamamuro T, Shimizu K, Saito T. Combined laminoplasty and posterolateral fusion for spinal canal surgery in children and adolescents. Clin Orthop Relate Res. 1990;259s:92–99. [PubMed] [Google Scholar]
- 16.Winter RB, Hall JE. Kyphosis in childhood and adolescence. Spine. 1978;3:285–308. doi: 10.1097/00007632-197812000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Yasuoka S, et al. Incidence of spinal column deformity after multilevel laminectomy in children and adults. J Neurosurg. 1982;57:441–445. doi: 10.3171/jns.1982.57.4.0441. [DOI] [PubMed] [Google Scholar]
- 18.Yücesoy K, Crawford NR. Increase in spinal canal area after inverse laminoplasty an anatomical study. Spine. 2000;25:2771–2776. doi: 10.1097/00007632-200011010-00009. [DOI] [PubMed] [Google Scholar]