Abstract
Diaschisis is the inhibition of function produced by focal disturbances in a portion of the brain at a distance from original site of injury. Many studies using brain SPECT (single-photon emission computed tomography) have demonstrated crossed cerebellar diaschisis (CCD) in patients with cerebral cortical infarct. We report a case of cerebrovascular accident involving the left middle cerebral artery territory. PET/CT performed one month after stroke showed hypometabolism in the left cerebral hemisphere with hypometabolism of the contralateral cerebellum. The finding of diminished glucose metabolism in the contralateral cerebellum represents CCD.
Keywords: Crossed cerebellar diaschisis, PET/CT, stroke
INTRODUCTION
Crossed cerebellar diaschisis (CCD) is a matched depression of blood blow or metabolism in the cerebellar hemisphere contralateral to a focal supratentorial lesion.[1] In acute brain disorders such as infarct, limitation of the excitatory output from an injured brain region reduces physiological activity in connecting brain regions remote from the lesion site. This is manifested as decreased cerebral blood flow or glucose metabolism.[1,2] CCD is characterized by secondary hypoperfusion due to neural deactivation.[3]
CASE REPORT
A 33-year-old female presented with acute onset right sided hemiparesis. CT scan of the brain showed ischemic stroke involving the left middle cerebral artery territory. Rest of the brain was structurally normal. MRI of the brain showed altered signal intensity in the left parietal, temporal cortices and left basal ganglia [Figure 1]. Both cerebellar hemispheres were normal.
Figure 1.
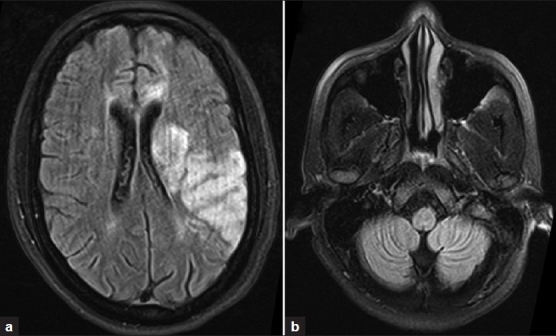
MRI of the brain (a) showing altered signal intensity in the left parietal, temporal cortices and left basal ganglia. Both cerebellar hemispheres (b) are normal
Patient was planned for stem cell transplant for stroke and underwent FDG PET/CT as part of routine evaluation. PET/CT of the brain revealed reduced FDG uptake in the frontal, parietal and temporal cortices and basal ganglia on the left side [Figure 2]. Correlative CT revealed a hypo-dense lesion in the medial part of the left basifrontal lobe, in the left Putamen extending superiorly to the left para-ventricular white matter and around the frontal horn of the left lateral ventricle. Additionally, right cerebellum showed reduced FDG uptake without any morphologic abnormality [Figures 3 and 4].
Figure 2.
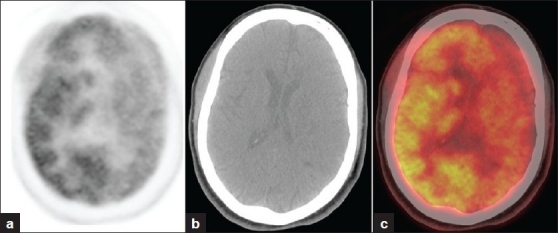
Transaxial sections at basal ganglia level (a) PET (b) CT (c) fused PET/CT showing FDG hypometabolism in the frontal, parietal and temporal cortices and basal ganglia on the left side region corresponding to a well defined hypodense area on CT
Figure 3.
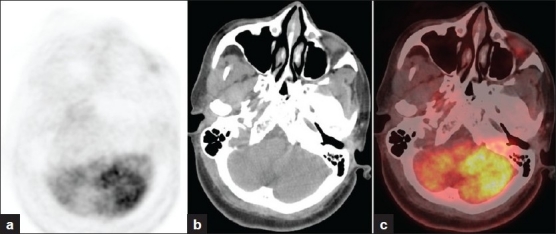
Transaxial sections at the cerebellar level (a) PET (b) CT (c) fused PET/CT showing diffuse FDG hypometabolism in the right cerebellar hemisphere with CT showing no morphological abnormality
Figure 4.
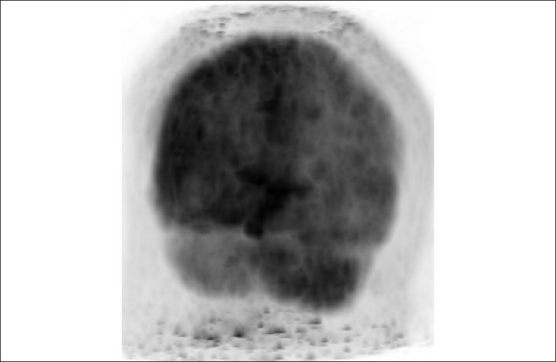
Maximum intensity projection image showing right cerebellar hypometabolism
DISCUSSION
The term “diaschisis” defined as a reversible, functional phenomenon without any structural change was introduced by von Monakow in 1914.[4] The underlying mechanism of CCD is the interruption of the corticopontocerebellar tract by the infarct causing deafferentation and transneural metabolic depression of the contra-lateral cerebellar hemisphere.[1] Baron in 1980 using PET imaging demonstrated matched reduction in cerebral blood flow and oxygen extraction fraction in the contralateral cerebellum in patients with supratentorial ischemic stroke.[2] The finding has been subsequently seen with SPECT perfusion imaging in many settings including: Internal capsule/basal ganglion infract, brain tumor, spinocerebellar degeneration, Alzheimer's disease, Wada test in epilepsy, and progressive supranuclear palsy.[5] Cerebral gliomas cause a reduction of glucose metabolism in the cerebellum contralateral to the tumor side CCD. Frontal lobe tumors have been reported to be associated with the highest CCD values. CCD was reportedly higher in malignant than in low-grade gliomas and increasing tumor size increased CCD values.[5]
Although acute-stage CCD has no prognostic value independent of acute-stage hypoperfusion volume, it might indicate the proportion of nutritional to non-nutritional perfusion at the infarct site, and hence, be useful in the evaluation of reperfusion therapies in the acute stage. CCD is a known complication of stroke both in acute and chronic phases. CCD appears to be prominent in patients with severe hemiparesis in various stages.[2] SPECT has been used to evaluate CCD in acute (5–30 hours),[6] early sub-acute (5-15 days),[7] and chronic (13–56 days) stages.[6] Several series of stroke have reported frequency of CCD after infarct greater than 60%.[8–10] CCD has been demonstrated on F18-FDG-PET up to 20 years after a cerebro-vascular accident[11] indicating the irreversibility of the lesion once the acute phase is over. It is of particular significance to the nuclear medicine physician as it is most often clinically and anatomically occult yet may frequently seen with cerebral perfusion studies. In summary, we present a unique case of CCD on F-18 FDG PET/CT scan whose abnormal findings reflect decreased glucose metabolism with CT showing normal morphology.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Baron JC, Bousser MG, Comar D, Castaigne P. Crossed cerebellar diaschisis in human supratentorial brain infarction. Trans Am Neurol Assoc. 1981;105:459–61. [PubMed] [Google Scholar]
- 2.Pantano P, Baron JC, Samson Y, Bousser MG, Derouesne C, Comar D. Crossed cerebellar diaschisis: Further studies. Brain. 1986;109:677–94. doi: 10.1093/brain/109.4.677. [DOI] [PubMed] [Google Scholar]
- 3.Ito H, Kanno I, Shimosegawa E, Tamura H, Okane K, Hatazawa J. Hemodynamic changes during neural deactivation in human brain: A positron emission tomography study of crossed cerebellar diaschisis. Ann Nucl Med. 2002;16:249–54. doi: 10.1007/BF03000103. [DOI] [PubMed] [Google Scholar]
- 4.Wiesendanger M. Constantin von Monakow (1853–1930): A pioneer in interdisciplinary brain research and a humanist. Comptes Rendus Biologies. 2006;329:406–18. doi: 10.1016/j.crvi.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 5.Otte A, Roelcke U, von Ammon K, Hausmann O, Maguire RP, Missimer J, et al. Crossed cerebellar diaschisis and brain tumor biochemistry studied with positron emission tomography, [F18] fluorodeoxyglucose and [11 C] methionine. J Neurol Sci. 1998;156:73–7. doi: 10.1016/s0022-510x(98)00019-7. [DOI] [PubMed] [Google Scholar]
- 6.Serrati C, Marchal G, Rioux P, Viader F, Petit-Taboué MC, Lochon P, et al. Contralateral cerebellar hypometabolism: A predictor for stroke outcome. J Neurol Neurosurg Psychiatry. 1994;57:174–9. doi: 10.1136/jnnp.57.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takasawa M, Watanabe M, Yamamoto S, Hoshi T, Sasaki T, Hashikawa K, et al. Prognostic value of subacute crossed CT study in patient with middle cerebral artery territory infarct. AJNR Am J Neuroradiol. 2002;23:189–93. [PMC free article] [PubMed] [Google Scholar]
- 8.Yamada H, Koshimoto Y, Sadato N, Kawashima Y, Tanaka M, Tsuchida C, et al. Crossed cerebellar diaschisis: Assessment with dynamic susceptibility contrast MR imaging. Radiology. 1999;210:558–62. doi: 10.1148/radiology.210.2.r99fe02558. [DOI] [PubMed] [Google Scholar]
- 9.Miura H, Nagata K, Hirata Y, Satoh Y, Watahiki Y, Hatazawa J. Evolution of crossed cerebellar diaschisis in middle cerebral artery infarction. J Neuroimaging. 1994;4:91–6. doi: 10.1111/jon19944291. [DOI] [PubMed] [Google Scholar]
- 10.Yamauchi H, Fukuyama H, Kimura J. Hemodynamic and metabolic changes in crossed cerebellar hypoperfusion. Stroke. 1992;23:855–60. doi: 10.1161/01.str.23.6.855. [DOI] [PubMed] [Google Scholar]
- 11.Shih WJ, Huang WS, Milan PP. F18-FDG PET demonstrates crossed cerebellar diaschisis 20 years after stroke. Clin Nucl Med. 2006;31:259–61. doi: 10.1097/01.rlu.0000210526.50300.f7. [DOI] [PubMed] [Google Scholar]


