Abstract
The growing elderly population in the United States presents medical, engineering, and legislative challenges in trauma management and prevention. Thoracic injury incidence, morbidity, and mortality increase with age. This study utilized receiver-operator characteristic analysis to identify the quantitative age thresholds associated with increased mortality in common isolated types of thoracic injuries from motor vehicle crashes (MVCs).
The subject pool consisted of patients with a single AIS 3+ thorax injury and no injury greater than AIS 2 in any other body region. A logistic regression algorithm was performed for each injury to estimate an age threshold that maximally discriminates between survivors and fatalities. The c-index describing discrimination of the model and odds ratio describing the increased mortality risk associated with being older than the age threshold were computed.
Twelve leading thoracic injuries were included in the study: unilateral and bilateral pulmonary contusion (AIS 3/4), hemo/pneumothorax, rib fractures with and without hemo/pneumothorax (AIS 3/4), bilateral flail chest, and thoracic penetrating injury with hemo/pneumothorax. Results are consistent with the traditional age threshold of 55, but were injury-specific. Pulmonary contusions had lower age thresholds compared to rib fractures. Higher severity pulmonary contusions and rib fractures had lower age thresholds compared to lower severity injuries.
This study presents the first quantitatively estimated mortality age thresholds for common isolated thoracic injuries. This data provides information on the ideal ‘threshold’ beyond which age becomes an important factor to patient survival. Results of the current study and future work could lead to improvements in automotive safety design and regulation, automated crash notification, and hospital treatment for the elderly.
INTRODUCTION
In motor vehicle crashes, thoracic injuries rank second only to head injuries in terms of the body region most often injured, number of fatalities and serious injuries, and overall economic cost (Cavanaugh 2002; Ruan, El-Jawahri et al. 2003). Injuries to the thorax account for 13% of all minor to moderate injuries and 29% of all serious to fatal injuries (Ruan, El-Jawahri et al. 2003). Up to 25% of traumatic deaths have been attributed to thoracic injuries (Dougall, Paul et al. 1977; Galan, Penalver et al. 1992; Allen and Coates 1996). While motor vehicle crashes are associated with 60–70% of blunt chest trauma, 20% is attributed to falls that are more commonly seen in elderly patients (Galan, Penalver et al. 1992; Allen and Coates 1996).
Adults 65 years of age and older currently constitute more than 12% of the total population and with increases in life expectancy, the elderly population is projected to reach more than 20% by 2050 (He 2005). Motor vehicle crash is a common source of trauma among the elderly population and elderly individuals have the second highest crash-related death rate compared to all age groups (National Center for Health Statistics 2003). Previous studies have shown that skeletal and physiological resilience decline with age, resulting in a decreased ability for the body to withstand traumatic insults (Burstein, Reilly et al. 1976; Zioupos and Currey 1998). In a study of hospitalized motorcyclists, the incidence of thoracic injuries was significantly higher for individuals 40 years or older (Dischinger, Ryb et al. 2006). The incidence of thoracic injuries increases with age for both belted and unbelted occupants in motor vehicle crashes (Hanna 2009). In the elderly, thoracic injury tolerance has been shown to decrease by 20% for blunt loading and up to 70% for concentrated belt-loading (Zhou 1996).
Thoracic morbidity and mortality increase with age, with older patients presenting with more comorbidities, developing more complications, and requiring more ventilator days, intensive care unit (ICU) days, and longer hospital stays (Finelli, Jonsson et al. 1989; Shorr, Rodriguez et al. 1989; Perdue, Watts et al. 1998; Holcomb, McMullin et al. 2003; Hanna 2009). Complications from thoracic injury include pneumonia, atelectasis, acute respiratory distress syndrome (ARDS), and respiratory failure that often result from hypoventilation due to rib fractures or pulmonary contusion. Elderly patients with rib fractures have two to five times the risk of mortality of younger patients with increases in risk observed as the number of rib fractures increase (Bergeron, Lavoie et al. 2003; Stawicki, Grossman et al. 2004). Each additional rib fracture results in a 19% increase in mortality and 27% increase in pneumonia (Bulger, Arneson et al. 2000). Flail chest has been associated with a 132% increase in mortality per decade after age 55 and prolonged hospitalization with age (Albaugh, Kann et al. 2000; Athanassiadi, Gerazounis et al. 2004). Pulmonary contusion, the leading thoracic soft tissue injury encountered in non-penetrating chest trauma, was also correlated with higher mortality in patients aged 60 years or older (Stellin 1991; Allen and Coates 1996).
Identifying the age at which an individual would be considered physiologically “elderly” is of value and could lead to improvements in countermeasure design and hospital treatment to prevent and mitigate injuries. In the TRISS scoring system and other studies, patients aged 55 years or older have traditionally been designated as elderly for the purposes of severity scoring, benchmarking, estimating comorbidity burden, and predicting survival probability (Boyd, Tolson et al. 1987). However, this age threshold may be injury specific and dependent on the location, severity, and number of injuries. A variety of age thresholds have been reported in the literature describing the increase in morbidity and mortality observed in elderly patients, with one study suggesting increased morbidity from rib fractures occurs as young as age 45 (Holcomb, McMullin et al. 2003). Increased mortality was observed in the 65 and older population in studies of trauma patients and specifically patients with rib fractures (Finelli, Jonsson et al. 1989; Bergeron, Rossignol et al. 2004; Stawicki, Grossman et al. 2004). Other studies have shown patients older than 60 with rib fractures or pulmonary contusion have increased mortality, and mortality is increased in flail chest patients over age 55 (Stellin 1991; Albaugh, Kann et al. 2000; Sirmali, Turut et al. 2003). While it is clear from the literature that morbidity and mortality are increased in older patients, a statistical investigation of trauma data is necessitated to determine the age thresholds for particular injuries that significantly affecting morbidity and mortality. In a previous study, mortality age thresholds estimated for isolated head injuries were found to be near the traditional age threshold (55 years), but were injury specific (Stitzel, Kilgo et al. 2008). This study aims to investigate isolated thoracic injuries in a similar manner and quantify the effect of patient age on mortality outcome.
METHODS
This study sought to characterize the effect of age on hospital survival in patients that sustained serious to severe thorax injuries. Further, age thresholds that optimally discriminate survival for a given injury were estimated.
Injury severity was classified using the Abbreviated Injury Scale (AIS). The AIS coding system is a consensus-derived classification lexicon that categorizes injuries based on body region, anatomic structure affected, and other injury specifics. An injury severity metric is associated with each injury that quantifies severity on an ordinal scale from 1 (minor injury) to 6 (thought to be unsurvivable).
Inclusion Criteria
Patients of all ages and all mechanisms of injury were eligible for entry into the study. Patients with missing age, missing survival status or patients with injury classifications from other scales were excluded from the study, as were patients with serious or severe injuries greater than AIS 3 in other body regions. Patients older than 89 years in the National Trauma Data Bank (NTDB) are given an age of −1. Since their exact age is not provided and is needed for the statistical analysis, patients older than 89 years were excluded from this study. Thus, the final subject pool consisted of patients with a single thorax injury of severity 3 or higher and no other injury greater than AIS of 2 in any other body region. Patients with multiple serious thorax injuries were excluded so that a more precise estimate of age effects attributable to the thorax injury could be measured.
Once a pool of patients who fit the above criteria was identified, a simple logistic regression algorithm was performed separately for each injury to assess the univariate association between age and mortality. Those injuries with a significant association between age and mortality were subset for further study to estimate age threshold values.
Data Source and Sample
Data used was from the American College of Surgeons (ACS) NTDB version 7, Motor Vehicle Crash cases from Jan 1, 2003 to Dec 31, 2007. The NTDB is the most complete national trauma database available. Data regarding demographics, injury severity and injury origin is collected as well as descriptive accounts of the incident. Criteria for participation in the database include the reporting institution’s trauma accreditation and hospital or emergency department admission. Patients who are dead upon arrival are not included in the NTDB.
A total of 957,845 NTDB patients had specific injuries in one of the eight body regions and were coded with the AIS system. This original sample includes patients from 517 trauma centers and hospitals. Of these, 137,119 have a single thorax injury (most with injuries to other body regions too). When sub-setting patients with serious thorax injuries (AIS ≥ 3) and minimal injury severity in the other regions (AIS < 3), the patient pool shrinks to 30,369, of which 29,185 patients have non-missing age and death status. Thus, the set of patients who meet the entry criteria total 29,185 from 341 hospitals including 55 Level I and 55 Level II trauma centers. However, not all of these patients were studied because not all serious thorax injuries were studied. The final patient pool includes 13963 (47.8%) motor vehicle crashes (MVC) and 14853 cases of other traumatic etiology; cause of injury was missing in 369 cases. The death rate for MVC and Other trauma cases was 4.2% and 5.3%, respectively.
Data submitted to NTDB are rigorously examined using both the NTRACS system institutionally and an additional logical checks system created and enforced by NTDB administrators. All institutions that contribute to the NTDB are either ACS-verified, state-designated, or self-designated as trauma centers.
Statistical Analysis
Separate logistic regression models were fit and used to identify injuries that exhibit a significant relationship between survival and age (at this stage, age is measured numerically in years). Injuries that have a statistically discernible relationship between survival and age were further studied to try to estimate an age threshold, that is, a cutoff value that maximally discriminates between survivors and those who died in-hospital. Age thresholds are often used in trauma as a proxy for pre-existing comorbidities but are also used to help clinicians have a better understanding of the varying effects of age on morbidity and mortality across a spectrum of different injuries in a single body region.
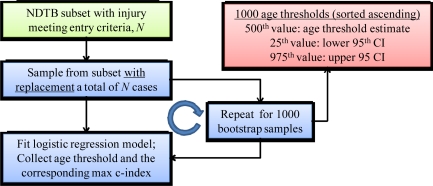
The analysis of each injury occurred in a two-stage process. The first stage consisted of an algorithm designed to estimate the age threshold of the injury (Figure 1). Bootstrapping, a re-sampling scheme, was employed to provide the age threshold estimate along with 95% confidence intervals (CI). For each injury, 1000 bootstrap replication samples were drawn with replacement from the sample of patients with the injury under consideration. The sample size of each of the 1000 replicates was equal to the number cases in the original patient pool that exhibited the injury. For each of the 1000 bootstrap samples, 70 different logistic regression models were fit, representing 70 different age cutoffs in one-year increments for ages 20–89. For each of the 70 models, the c-index, a measure of model discrimination (equivalent to the area under the ROC curve in these models) was measured. In each replicated sample, the age cutoff that produced the largest c-index and the value of the c-index was collected. Thus, after the algorithm is complete, 1000 different estimates of the optimal age threshold are available. After ordering the 1000 age threshold estimates from smallest to largest, the median (500th ordered value) was used as the final estimate and the 25th and 975th ordered values represented the lower and upper bounds of a 95% confidence interval around the estimate. The reason that bootstrapping is employed, as opposed to just estimating the age threshold from the observed sample, is that the resampling algorithm offers the opportunity to provide an interval estimate (95% confidence bounds) that are not estimable otherwise.
Figure 1.
Flow chart of bootstrapping algorithm to estimate age threshold
The second stage of analysis for each injury employed the age threshold estimate from the first stage and defined a dichotomous cutoff variable based on its value. Then, a logistic regression model was fit to the original patient sample who exhibited the injury. The number of patients and the number of deaths for each injury was noted. Also, to verify that the distribution of deaths was wide enough to estimate a middle-range age threshold, the mean age of the dead patients, along with the range, was recorded and checked for adequate spread. The odds ratio associated with the age threshold, along with a 95% CI, was calculated which is a very close approximation (because event rates are so low) to the additional mortality risk associates with being older than the threshold age. Additionally, the c-index for the injury sample was measured to describe the ability of the model to discriminate between survivors and non-survivors at a particular age threshold.
All analyses were performed with SAS Version 9.2 (Cary, NC). The alpha level for each test was set to 0.05.
RESULTS
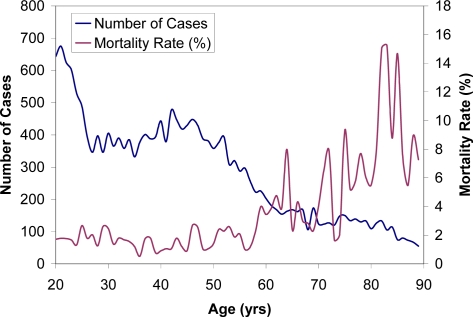
Twelve thoracic injuries met all of the study criteria. Unilateral and bilateral pulmonary contusion (AIS 3/4), hemo/pneumothorax, rib fractures with and without hemo/pneumothorax (AIS 3/4), bilateral flail chest, and thoracic penetrating injury with hemo/pneumothorax were all identified and included in the study. The twelve types of thoracic injuries are listed in Table 1 along with AIS codes, injury descriptions, frequency of incidence, and mortality results. The total number of patients in the study was 20603 and mortality for the injuries ranged from 0.5 to 43.9%. A plot of the distribution of the cases and mortality rate with age is provided in the Appendix (Figure 5).
Table 1.
Injuries considered in the NTDB analysis
| AIS Code | Abbrev. | Injury Description | Cases | Deaths (%) |
|---|---|---|---|---|
| 441406.3 | LCU | Unilateral lung contusion | 3332 | 15 (0.5) |
| 441410.4 | LCB | Bilateral lung contusion | 1237 | 38 (3.1) |
| 450230.3 | RF4 | Rib fracture, > 3 one side, <= 3 other side | 2585 | 43 (1.7) |
| 450222.3 | RFHP2 | Rib fracture, 2–3, HTX/PTX | 2505 | 34 (1.4) |
| 450232.4 | RFHP4 | Rib fracture, > 3 one side, <= 3 other side, HTX/PTX | 1567 | 43 (2.7) |
| 442202.3 | HP | Thoracic cavity injury, NFS, HTX/PTX | 7031 | 231 (3.3) |
| 450211.3 | RFHP | Multiple rib fractures, NFS, HTX/PTX | 192 | 3 (1.6) |
| 450252.4 | ORFHP | Open/displaced/comminuted rib fracture, > 1, HTX/PTX | 235 | 11 (4.7) |
| 450214.3 | RFHP1 | Single rib fracture, HTX/PTX | 1663 | 24 (1.4) |
| 450266.5 | FCB | Bilateral flail chest | 41 | 18 (43.9) |
| 441402.3 | LC | Lung contusion, NFS | 2418 | 42 (1.7) |
| 416008.3 | TPIHP | Thoracic penetrating injury, NFS, HTX/PTX, except tension PTX | 1129 | 51 (4.5) |
NFS: not further specified, HTX: hemothorax, PTX: pneumothorax
A separate analysis of NASS/CDS 2000–2008 data was conducted to determine the frequency of thoracic injuries in the population of motor vehicle crash victims. Table 2 lists the AIS codes, the number of weighted and unweighted NASS cases, and the frequency percent and ranking of each injury among all AIS 3+ thoracic injuries in NASS. Injuries selected for the age threshold analysis were among the 16 top-ranked injuries in terms of occurring frequency in the population and account for 76% of the total AIS 3+ thoracic injuries.
Table 2.
Select AIS 3+ thoracic injuries in NASS/CDS 2000–2008
| NASS Cases | AIS 3+ Thorax Injury Freq. | ||||
|---|---|---|---|---|---|
| AIS Code | Abbrev. | Weighted | Unweighted | Percent (%) | Ranking |
| 441406.3 | LCU | 131695 | 1540 | 22.4 | 1 |
| 441410.4 | LCB | 85124 | 1383 | 14.5 | 2 |
| 450230.3 | RF4 | 48965 | 678 | 8.3 | 3 |
| 450222.3 | RFHP2 | 43339 | 542 | 7.4 | 4 |
| 450232.4 | RFHP4 | 39349 | 611 | 6.7 | 5 |
| 442202.3 | HP | 30294 | 462 | 5.1 | 6 |
| 450211.3 | RFHP | 20768 | 268 | 3.5 | 7 |
| 450252.4 | ORFHP | 14510 | 217 | 2.5 | 9 |
| 450214.3 | RFHP1 | 13177 | 221 | 2.2 | 10 |
| 450266.5 | FCB | 11978 | 286 | 2.0 | 11 |
| 441402.3 | LC | 7479 | 111 | 1.3 | 16 |
| 416008.3 | TPIHP | NA | NA | NA | NA |
Table 3 shows the results of the statistical analysis to determine the age thresholds for each of the twelve thoracic injuries selected for this study. The mean age of mortality, along with the range, are reported for each injury. The age threshold associated with increased mortality risk is reported for each injury, along with 95% confidence intervals. All age thresholds and confidence intervals were found to lie in the age ranges of deaths, verifying the distribution of deaths was wide enough to estimate the middle-range age threshold. For each injury, the odds ratio for death at the age threshold is provided, along with a 95% confidence interval. This ratio estimates the additional mortality risk associated with being older than the threshold age. Statistical parameters such as the mean peak ROC value of 1000 replication samples and the peak c-index are listed.
Table 3.
Statistical results for age threshold analysis of twelve thoracic injuries
| AIS Code | Abbrev. | Mean Age (Range) Among Deaths | Mean Peak ROC Value of 1000 Replicates | Age Threshold (95% CI) | Odds ratio of death at Threshold Age (95%CI) | Peak C-index |
|---|---|---|---|---|---|---|
| 441406.3 | LCU | 46 (11–89) | 0.685 | 58 (22–71) | 8.58 (3.09–23.82) | 0.687 |
| 441410.4 | LCB | 47 (2–85) | 0.651 | 46 (46–47) | 5.04 (2.62–9.71) | 0.678 |
| 450230.3 | RF4 | 70 (1–89) | 0.719 | 63 (63–64) | 8.54 (3.95–18.49) | 0.738 |
| 450222.3 | RFHP2 | 67 (15–88) | 0.673 | 69 (59–75) | 7.80 (3.88–15.70) | 0.723 |
| 450232.4 | RFHP4 | 67 (30–88) | 0.718 | 60 (56–69) | 6.59 (3.36–12.96) | 0.720 |
| 442202.3 | HP | 45 (3–89) | 0.629 | 55 (43–61) | 4.19 (3.17–5.54) | 0.621 |
| 450211.3 | RFHP | 69 (50–85) | 0.788 | 50 (50–50) | Infinity | -- |
| 450252.4 | ORFHP | 55 (22–78) | 0.681 | 47 (47–47) | 5.1 (1.08–24.14) | 0.675 |
| 450214.3 | RFHP1 | 67 (30–86) | 0.792 | 61 (61–63) | 17.3 (6.40–46.7) | 0.806 |
| 450266.5 | FCB | 53 (21–87) | 0.622 | 58 (58–58) | 0.35 (0.10–1.32) | 0.622 |
| 441402.3 | LC | 46 (0–89) | 0.686 | 54 (41–63) | 6.34 (3.40–11.82) | 0.685 |
| 416008.3 | TPIHP | 38 (20–76) | 0.623 | 37 (21–53) | 2.79 (1.58–4.90) | 0.619 |
The results are consistent with the threshold of age 55 used in the Trauma Injury Severity Score (TRISS), with half of the computed age thresholds falling within the 50–60 year range. The highest age threshold was for 2–3 rib fractures with hemo/pneumothorax (AIS code 450222.3, Age=69 years, 95% CI 59–75, Odds Ratio=7.80, 95% CI 3.88–15.70), while the lowest age threshold was for a thoracic penetrating injury with hemo/pneumothorax (AIS code 416008.3, Age=37 years, 95% CI 21–53, Odds Ratio=2.79, 95% CI 1.58–4.90). Pulmonary contusions tended to have lower age thresholds compared with rib fractures.
In general, age thresholds for higher severity pulmonary contusions and higher severity rib fractures are lower than those for lower severity injuries. An exception is seen in the case of bilateral flail chest (AIS 450266.5), in that an AIS 5 injury received a higher age threshold (58 years) than seven AIS 3 and 4 injuries. Bilateral flail chest had a very high mortality risk (43.9%) that, when compared with other injury types, may not be as dependent on age. The odds ratio (0.35, 95% CI 0.10–1.32) for bilateral flail chest also suggests there is not an increased risk of mortality for individuals older than the age threshold.
For the other injuries in the analysis, the odds ratios indicate that individuals older than the estimated age threshold for each injury are 2.79 to 17.3 times more likely to die than individuals under the age threshold. AIS 3 rib fractures had the highest odds ratios ranging from 7.80 to 17.3.
Thresholds presented in this study are associated with good discrimination between survivors and non-survivors. The c-index represents the proportion of survivors that have a higher predicted survival than a non-survivor for a particular injury. Maximal c-index values in this study ranged from 0.62 – 0.81 suggesting relatively good model discrimination.
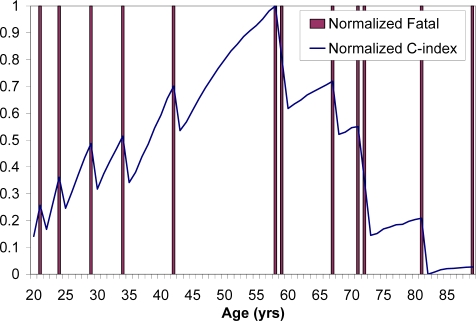
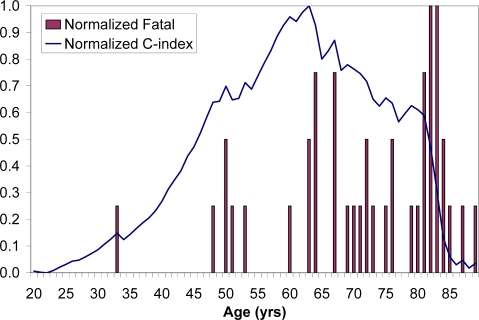
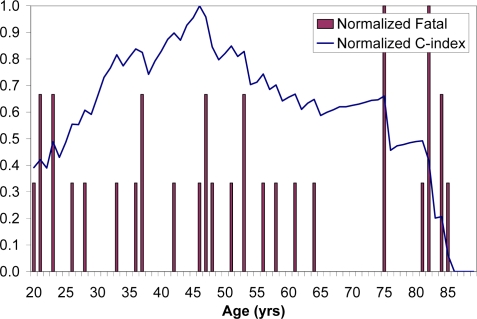
We sought to qualitatively evaluate the effect of fatalities on the overall variation in the c-index using normalized histograms of the study population and the fatality incidence in these cases (Figures 2–4). Plots are provided for the three most frequent thoracic injuries in NASS. In these plots, c-index is normalized by subtracting the minimum from the dataset and dividing by the maximum to put c-indexes on a scale from 0 to 1. Fatalities, a maximum of four per age group, are normalized by the maximum to appear on a scale from 0–1 as well. Maximum discrimination of survival occurs at the age threshold corresponding to the peak c-index and is influenced by the proportion of fatalities with age.
Figure 2.
Normalized fatalities and c-index for unilateral lung contusion, AIS 441406.3
Figure 4.
Normalized fatalities and c-index for rib fracture, > 3 one side, <= 3 other side, AIS 450230.3
DISCUSSION
Choosing an age threshold which best discriminates mortality due to an injury is a difficult task. Traditionally, as in TRISS, patients 55 and over are classified as elderly. However, a variety of other age thresholds have been used in the literature to examine increased mortality risk in the elderly following injury. These thresholds can be injury specific and determining the age at which mortality risk increases is valuable to clinicians who may take extra precautions when treating high-risk patients. Currently, physicians may assess the mortality risk of a patient based on their clinical experience or the AIS code of the injury. Numerous studies have correlated AIS to injury mortality, but this scoring system is not age-specific (Meredith, Evans et al. 2002). Also, for patients with multiple serious injuries, calculating the mortality age threshold associated with individual injuries becomes more complex. This study attempts to remove the effect of other injuries by selecting cases with an isolated AIS 3+ thorax injury with AIS 2- injuries in all other body regions.
The current study investigated twelve common types of thoracic injuries. These injuries account for the majority (76%) of all AIS 3+ thoracic injuries in NASS, a population-based database of motor vehicle crashes. These twelve isolated injuries had an average of 1,995 cases in NTDB, an average mortality of 5.9%, and an average of 46 deaths per injury from which to draw conclusions regarding the relationship between the isolated injury and mortality in these populations.
Age thresholds were identified by local and overall maximums in the c-index (equivalent to the area under the ROC curve). These maximums on the ROC curve are associated with shifts in the actual versus predicted mortality and occur at the age thresholds that produce the best discrimination of survivors and non-survivors. In this study, the age thresholds indicating increased mortality risk for specific thoracic injuries were below the average human life span, with the majority falling in the 50–60 year age range. The average estimated age threshold for all twelve thoracic injuries was 54.8 years, which is consistent with the traditional age threshold of 55 years used to classify trauma patients as elderly. If age did not have an effect on mortality in the injured, age thresholds in the 80–90 year range might be expected due to normal human life span and physiological changes with age. Therefore, results of this study suggest that it is the injury and not just normal physiological changes the cause increased mortality risk beyond a certain age for a particular thoracic injury.
Higher severity pulmonary contusions were associated with lower mortality age threshold. While AIS 3 unilateral/non-specified pulmonary contusions had age thresholds near the traditional 55 year cutoff, AIS 4 bilateral contusions had an age threshold nearly a decade below the traditional threshold. Pulmonary contusions can result in severe respiratory complications that can result in death or long-term respiratory impairment. Adult respiratory distress syndrome (ARDS) is observed in 5–20 percent of pulmonary contusion cases and patients developing ARDS have a mortality risk of 20–50 percent (Allen and Coates 1996; Miller, Croce et al. 2002). Pulmonary contusion and age over 65 years are both independent predictors of ARDS, which suggesting elderly patients with pulmonary contusion may have a higher risk of developing ARDS and a subsequently higher mortality risk. Volumes of contusion greater than 20% have also been associated with an increased risk of ARDS, which could possibly explain the lower age threshold in bilateral versus unilateral contusions (Miller, Croce et al. 2001). Pneumonia and pulmonary sepsis affect 5 to 50 percent of pulmonary contusion cases (Allen and Coates 1996). The incidence of pneumonia increases with age and is associated with higher morbidity and mortality in the elderly (Fein 1999).
For rib fractures without flail chest, injuries with a higher severity (AIS 4 versus AIS 3) also had lower mortality age thresholds. The presence of hemothorax/pneumothorax in the case of rib fractures, > 3 one side, <= 3 other side (AIS 450232.4) resulted in a slightly lower age threshold of 60 versus 63 for AIS 450230.3. For open/displaced/comminuted rib fractures with hemo/pneumothorax (AIS 450252.4), the best discrimination of survival occurred at an age threshold of 47 years. Overall, the average age threshold was 61 years for AIS 3 fractures versus 54 years for AIS 4 fractures. Mortality has been shown to increase with the number of rib fractures and increases more significantly in the elderly. Patients with rib fractures are at risk of developing pulmonary complications such as pneumonia that increase the risk of death. Elderly patients are not only more likely to develop pneumonia after sustaining rib fractures, but they are more likely to die from it compared to a younger cohort (Bulger, Arneson et al. 2000).
Despite injury severity, age thresholds for bilateral flail chest (AIS 450266.5) and rib fracture, > 3 1 side, <= 3 other side, with HTX/PHX (AIS 450232.4) were higher than several of the AIS 3 injuries. In the case of these severe injuries where mortality risk is elevated, the effect of age on mortality appears to not be as pronounced as it is compared to several AIS 3 thoracic injuries. However, age has previously been shown to be the strongest predictor of patient outcome with flail chest and is associated with increased mortality in patients aged 55 and older (Albaugh, Kann et al. 2000). The threshold used by Albaugh et al. (2000) is consistent with the 58 year age threshold identified in this study to discriminate between survivors and non-survivors of bilateral flail chest.
The number of fatal cases for each injury had some influence on the overall predictions. In the case of the AIS 450211.3 injury, only three fatalities were present in the dataset. The algorithm was unable to compute an odds ratio and peak c-index for this injury because there were no fatalities under 50 years of age. The number of fatal cases also affected the confidence intervals for particular injuries. The three injuries with the lowest number of fatal cases also had very narrow confidence intervals (AIS 450211.3, 450252.4, and 450266.5). For the remaining nine injuries, there was less uncertainty regarding the threshold as a good predictor of survival. Inspection plots of the c-index versus age indicate a clear maximum discrimination of the model at a particular age threshold.
One limitation of this study is the NTDB does not always include pre-existing comorbidities, which are important in estimating mortality risk in the aged. The objective of the current study was to determine the age threshold that best discriminates between survival and non-survival for a particular injury, but the effects of age and comorbidities are not separated in the analysis. Current trauma scoring systems assume age as a surrogate for comorbidities. However, there is no uniformly agreed upon way to adjust for comorbidities and solely investigate the effect of age, presenting a limitation to the current study. Future work could include an analysis of comorbidities and their effect on the survival age threshold for these thoracic injuries.
While the NTDB is an expansive dataset of traumatic injuries, one limitation is it’s reliance on voluntary participation from individual trauma centers. This could possibly result in unequal representation and discrepancies in the coding schemes across centers.
Another limitation of NTDB is the exclusion of patients that die before hospital admission. This could affect the results by underpredicting the proportion of fatalities. The underprediction of fatalities is expected to be more prominent as the severity (AIS) of the thoracic injury increases.
One of the stronger aspects of this study is its focus on isolated injuries with only AIS < 3 in other body regions as it moderates issues with injury interaction or the combined effects of injuries in the patients selected for the study. Overall there are limitations to this study including the fact that selecting for individual injuries with only moderate other injuries might have resulted in enrolling individuals with more severe injuries who died of the most severe injury and other more severe injuries might have been missed or not coded. The limitation of the study cohort to individuals with only one AIS 3+ injury lowered the number of fatalities that could be included in the study populations and may limit generalizability of the study. However, the selection of individuals with one severe injury and other lower severity injuries increased the numbers of individuals that could be considered beyond that that would be available selecting only for isolated injuries. Overall odds ratios and confidence intervals were statistically significant indicating the approach accomplished the stated objective of the study.
CONCLUSION
This study presents the first quantitatively estimated mortality age thresholds for common isolated thoracic injuries. These thresholds indicate the age beyond which mortality risk is increased for a particular injury. The estimated adjusted threshold ages appear to be injury specific, but are fairly close to the traditional age threshold (55 years). This research could be expanded to investigate mortality age thresholds in patients with multiple injuries or injuries in other body regions. Results of the current study and future work could lead to improvements in automotive safety design and regulation, automated crash notification, and hospital triage and treatment that is more sensitive to age.
Figure 3.
Normalized fatalities and c-index for bilateral lung contusion, AIS 441410.4
Acknowledgments
Work was performed for the Crash Injury Research and Engineering Network (CIREN) Project at Wake Forest University School of Medicine in cooperation with the United States Department of Transportation/National Highway Traffic Safety Administration (USDOT/NHTSA). Funding has been provided by Toyota Motor North America Inc. under Cooperative Agreement Number DTNH22-05-H-61001. Views expressed are those of the authors and do not represent the views of any of the sponsors or NHTSA.
APPENDIX
Figure 5.
Distribution of number of cases and mortality rate with age
REFERENCES
- Albaugh G, Kann B, et al. “Age-adjusted outcomes in traumatic flail chest injuries in the elderly.”. Am Surg. 2000;66(10):978–81. [PubMed] [Google Scholar]
- Allen GS, Coates NE. “Pulmonary contusion: a collective review.”. Am Surg. 1996;62(11):895–900. [PubMed] [Google Scholar]
- Athanassiadi K, Gerazounis M, et al. “Management of 150 flail chest injuries: analysis of risk factors affecting outcome.”. European Journal of Cardio-Thoracic Surgery. 2004;26(2):373–376. doi: 10.1016/j.ejcts.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Bergeron E, Lavoie A, et al. “Elderly Trauma Patients with Rib Fractures Are at Greater Risk of Death and Pneumonia.”. J Trauma. 2003;54(3):478–485. doi: 10.1097/01.TA.0000037095.83469.4C. [DOI] [PubMed] [Google Scholar]
- Bergeron E, Rossignol M, et al. “Improving the TRISS methodology by restructuring age categories and adding comorbidities.”. J Trauma. 2004;56(4):760–7. doi: 10.1097/01.ta.0000119199.52226.c0. [DOI] [PubMed] [Google Scholar]
- Boyd CR, Tolson MA, et al. “Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score.”. J Trauma. 1987;27(4):370–8. [PubMed] [Google Scholar]
- Bulger EMMD, Arneson MAMD, et al. “Rib Fractures in the Elderly.”. Journal of Trauma-Injury Infection & Critical Care. 2000;48(6):1040–1047. doi: 10.1097/00005373-200006000-00007. [DOI] [PubMed] [Google Scholar]
- Burstein AH, Reilly DT, et al. “Aging of bone tissue: mechanical properties.”. J Bone Joint Surg Am. 1976;58(1):82–6. [PubMed] [Google Scholar]
- Cavanaugh JM. Alan JM, Nahum M. Accidental Injury: Biomechanics and Prevention. New York: Springer-Verlag; 2002. Biomechanics of Thoracic Trauma; pp. 374–404. [Google Scholar]
- Dischinger PC, Ryb GE, et al. “Injury patterns and severity among hospitalized motorcyclists: a comparison of younger and older riders.”. Annu Proc Assoc Adv Automot Med. 2006;50:237–49. [PMC free article] [PubMed] [Google Scholar]
- Dougall AM, Paul ME, et al. “Chest Trauma-Current Morbidity and Mortality.”. J Trauma. 1977;17(7):547–553. [PubMed] [Google Scholar]
- Fein AM. “Pneumonia in the elderly: overview of diagnostic and therapeutic approaches.”. Clin Infect Dis. 1999;28(4):726–9. doi: 10.1086/515218. [DOI] [PubMed] [Google Scholar]
- Finelli FC, Jonsson J, et al. “A Case Control Study for Major Trauma in Geriatric Patients.”. J Trauma. 1989;29(5):541–548. doi: 10.1097/00005373-198905000-00001. [DOI] [PubMed] [Google Scholar]
- Galan G, Penalver JC, et al. “Blunt chest injuries in 1696 patients.”. Eur J Cardiothorac Surg. 1992;6(6):284–7. doi: 10.1016/1010-7940(92)90143-l. [DOI] [PubMed] [Google Scholar]
- Hanna R, Hershman Lawrence. Washington, DC: National Highway Traffic Safety Administration; 2009. Evaluation of Thoracic Injuries Among Older Motor Vehicle Occupants. [Google Scholar]
- He W, Sengupta Manisha, Velkoff Victoria A, DeBarros Kimberly A. Washington, DC: U.S. Government Printing Office; 2005. 65+ in the United States: 2005 US Census Bureau, Current Population Reports; pp. 23–209. [Google Scholar]
- Holcomb JB, McMullin NR, et al. “Morbidity from rib fractures increases after age 45.”. J Am Coll Surg. 2003;196(4):549–55. doi: 10.1016/S1072-7515(02)01894-X. [DOI] [PubMed] [Google Scholar]
- Meredith JW, Evans G, et al. “A comparison of the abilities of nine scoring algorithms in predicting mortality.”. J Trauma. 2002;53(4):621–8. doi: 10.1097/00005373-200210000-00001. discussion 628–9. [DOI] [PubMed] [Google Scholar]
- Miller PR, Croce MA, et al. “ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients.”. J Trauma. 2001;51(2):223–8. doi: 10.1097/00005373-200108000-00003. discussion 229–30. [DOI] [PubMed] [Google Scholar]
- Miller PR, Croce MA, et al. “Acute respiratory distress syndrome in blunt trauma: identification of independent risk factors.”. Am Surg. 2002;68(10):845–50. discussion 850–1. [PubMed] [Google Scholar]
- National Center for Health Statistics, N 2003. Health, United States, 2002, Special Excerpt: Trend Tables on 65 and Older Population, Centers for Disease Control and Prevention/National Center for Health Statistics, Department of Health and Human Services.
- Perdue PW, Watts DD, et al. “Differences in Mortality between Elderly and Younger Adult Trauma Patients: Geriatric Status Increases Risk of Delayed Death.”. J Trauma. 1998;45(4):805–810. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- Ruan J, El-Jawahri R, et al. “Prediction and analysis of human thoracic impact responses and injuries in cadaver impacts using a full human body finite element model.”. Stapp Car Crash J. 2003;47:299–321. doi: 10.4271/2003-22-0014. [DOI] [PubMed] [Google Scholar]
- Shorr RM, Rodriguez A, et al. “Blunt Chest Trauma in the Elderly.”. J Trauma. 1989;29(2):234–237. doi: 10.1097/00005373-198902000-00016. [DOI] [PubMed] [Google Scholar]
- Sirmali M, Turut H, et al. “A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management.”. Eur J Cardiothorac Surg. 2003;24(1):133–8. doi: 10.1016/s1010-7940(03)00256-2. [DOI] [PubMed] [Google Scholar]
- Stawicki SP, Grossman MD, et al. “Rib fractures in the elderly: a marker of injury severity.”. J Am Geriatr Soc. 2004;52(5):805–8. doi: 10.1111/j.1532-5415.2004.52223.x. [DOI] [PubMed] [Google Scholar]
- Stellin G. “Survival in trauma victims with pulmonary contusion.”. Am Surg. 1991;57(12):780–4. [PubMed] [Google Scholar]
- Stitzel JD, Kilgo PD, et al. “Age thresholds for increased mortality of three predominant crash induced head injuries.”. Annu Proc Assoc Adv Automot Med. 2008;52:235–44. [PMC free article] [PubMed] [Google Scholar]
- Zhou Q, Rouhana Stephen W, Melvin John W. “Age Effects on Thoracic Injury Tolerance.”. Stapp Car Crash J. 1996.
- Zioupos P, Currey JD. “Changes in the stiffness, strength, and toughness of human cortical bone with age.”. Bone. 1998;22(1):57–66. doi: 10.1016/s8756-3282(97)00228-7. [DOI] [PubMed] [Google Scholar]