Abstract
Objective
We investigated the clinical and radiological advantages of unilateral laminectomy in posterior lumbar interbody fusion (PLIF) procedure comparing with bilateral laminectomy, under the same procedural condition including bilateral instrumentation and insertion of two cages, in patients with degenerative lumbar disease with unilateral leg symptoms.
Methods
We retrospectively reviewed 124 consecutive cases of PLIF via unilateral or bilateral approach between January 2006 and April 2010. In 80 cases (bilateral group), two cages were inserted via bilateral laminectomy, and in 44 cases (unilateral group), via unilateral laminectomy. The average follow-up duration was 29.5 months. The clinical outcomes were evaluated with the Visual Analogue Scale (VAS) and the Oswestry disability index (ODI). The fusion rates and disc space heights were determined by dynamic standing radiographs and/or computed tomography. Operative times, intra-operative and post-operative blood losses and hospitalization periods were also evaluated.
Results
In clinical evaluation, the VAS and ODI scores showed excellent outcomes in both groups. There were no significant differences in term of fusion rate, but the perioperative blood loss and the operative time of the unilateral group were lower than that of the bilateral group.
Conclusion
Unilateral laminectomy can minimize the operative time and perioperative blood loss in PLIF procedure. However, the different preoperative disc height between two groups is a limitation of this study. Despite this limitation, solid fusion and satisfactory symptomatic improvement could be achieved uniquely by our surgical method. This surgical method can be an alternative surgical technique in patients with unilateral leg pain.
Keywords: Posterior lumbar interbody fusion, Iatrogenic root injury, Unilateral approach, Unilateral leg symptoms
INTRODUCTION
Posterior lumbar interbody fusion (PLIF) was initially introduced by Dr. Ralph Cloward14) in 1953 and has been a commonly performed surgical procedure24). PLIF involving the insertion of bilateral interbody cages is a standard treatment for restoring disc height, immobilizing unstable degenerated intervertebral disc areas, decompressing the dural sac and nerve roots, restoring load bearing to anterior structures, segmental alignment and balance, and obtaining successful fusion4,17). It is used in a variety of spinal diseases, including spinal stenosis, spondylolisthesis, degenerative intervertebral disc disease and trauma15).
Many techniques have been described, but in a standard PLIF technique, two cages are usually inserted via a bilateral approach with extensive laminectomy or posterior facetectomy, and combined pedicle screws are frequently used to provide spinal stability till the formation of a fusion mass7). When PLIF is performed, as recommended with bilateral interbody cages and pedicle screw fixation, it has increased the successful fusion rate6,10,22).
Unfortunately, the extensive exposure required for posterior pedicle screw fixation can cause unnecessary trauma to the posterior element and consequentially increased infection rates and lumbar musculoligamentous complex injury, which can result in poor clinical outcomes6,7). However, PLIF without posterior instrumentation also has complications, such as iatrogenic instability or cage migration11). Hence, additional pedicle screw fixation is frequently performed in PLIF procedure to avoid these complications.
Neural decompression is the most important issue in PLIF procedure to achieve surgical goals. Sufficient decompressive laminectomy or facetectomy can give a satisfactory improvement on the leg symptoms in the degenerative lumbar spinal disease. However, in comparison with partial segmental laminectomy, total laminectomy can increase the risk of perioperative or postoperative complications such as prolonged operative time, increased blood loss, or adjacent segment structural instability12,23,33). It means that extent of laminectomy is the important point in PLIF, regarding perioperative complications, mentioned above. This point raises doubts about that unilateral laminectomy in the PLIF procedure may reduce such complications comparing with bilateral laminectomy, especially in the patients with unilateral sciatica. PLIF through bilateral laminectomy is associated with increased complication rates16,28,30). Elias et al.16) reported a 15% incidence of dural tear and postoperative radiculopathy. It was typically caused by excessive epidural bleeding and prolonged or excessive retraction.
Recently, a variation of the PLIF approach, the transforaminal interbody fusion (TLIF) has allowed unilateral placement of interbody cage. The TLIF approach may reduce operative times, blood losses, dural tears and radiculopathy risks, and yet provide comparable mechanical stability to the PLIF technique2,9,21,27). However, TLIF has an increased potential risk for excessive bleeding in the axilla and medial to the pedicle, inability to distract the interspace adequately, violation of the end plate and non-parallel driving and/or cage placement to the disc space36).
At present time, a unilateral approach with a variant of PLIF is often used to avoid the complications mentioned above. Many authors have reported similar fusion rates and clinical outcomes comparing bilateral PLIF using two cages via a bilateral approach with unilateral PLIF using a single cage via a unilateral approach8,9,17).
However, in comparative mechanical studies, the mean subsidence rate was higher in unilateral cage models compare to bilateral cages, as the contact pressure when only one cage is used was more intensively distributed onto the vertebral body and thus caused greater subsidence. The unilateral cage model also shifted more stress to the screw, which may lead to screw breakage13).
In this study, however, two cages were used in both groups. Under the same procedural condition, including bilateral posterior instrumentation and insertion of two cages, we investigated the influence of the extent of laminectomy. To the best of our knowledge, there are only few reports on the clinical outcomes of unilateral laminectomy comparing with bilateral laminectomy in PLIF procedure. We retrospectively compared the clinical and radiological outcomes of PLIF via unilateral or bilateral approach in selected patients with unilateral leg pain.
MATERIALS AND METHODS
Patient population
From January 2006 to April 2010, 124 patients who were diagnosed with spinal stenosis with degenerative disc disease, herniated intervertebral disc with lumbar instability or low grade spondylolisthesis underwent a PLIF via bilateral or unilateral approach with additional pedicle screw fixation. Bilateral approach versus unilateral approach was chosen based on surgeon's preference and indication between the two groups was not different retrospectively. Same surgical procedures were performed in two groups, including use of two cages and bilateral pedicle screw fixation, except performing laminectomy unilaterally or bilaterally. Patients who had been followed up for at least 12 months were then reviewed (80 patients in the bilateral group, 44 patients in the unilateral group).
Preoperative variables including age, sex, medical history and clinical findings, as well as original disc height were recorded. The inclusion criteria were as follows : 1) severe spinal stenosis with degeneative disc disease and spondylosis or segmental instability, 2) degenerative spondylolisthesis, grade I, and 3) huge or recurrent herniated nucleus pulposus requiring total laminectomy with facetectomy and fusion. Patients with spondylolytic spondylolisthesis presenting with bilateral leg pain were excluded. All patients had significant unilateral radiculopathy and/or back pain refractory to conservative treatments. Clinical follow-up consisted of appointments at 1, 2, 3 and 6 months and last visit.
Patients were evaluated using the Visual Analogue Scale (VAS) for leg pain and back pain. Magnetic resonance imaging or computed tomography (CT) scan with plain radiographies were performed preoperatively in all the patients.
Surgical procedures
The surgical procedures for unilateral approach were as follows. The patients were placed in the prone position on a Wilson frame under general anesthesia. Bilateral paraspinal muscle was dissected and replaced laterally via a posteromedial approach, and the lamina and facet joints were exposed. The unilateral partial hemilaminectomy and medial facetectomy were performed on the symptomatic side, as well as adequate foraminotomy depending on the cause of disease, preserving the facet joints as much as possible. The dura mater and the nerve root were medially retracted. Extensive removal of the disc and the adjacent endplates including the contralateral side was performed using a pituitary rongeur and a down-biting curette until subchondral bone was exposed. Two cages were inserted through only unilateral laminectomy, and each cage was filled with a local morselized bone graft that was composed of the lamina, the articular process and the spinous process obtained during posterior decompression. The first cage was inserted into the disc space and careful pushing to the contralateral side was performed with the curved curette. The second cage was inserted on the ipsilateral side in the same manner. Pedicle screw fixation was carried out after inserting the cages to prevent iatrogenic instability of the posterior joint. Hemostasis and standard wound closure was then performed. From the third postoperative day, a lumbar orthosis was used when the patient was standing or walking and recommended for 2-3 months after surgery.
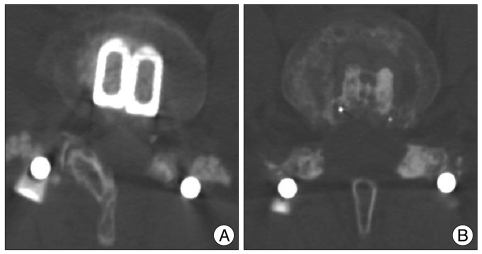
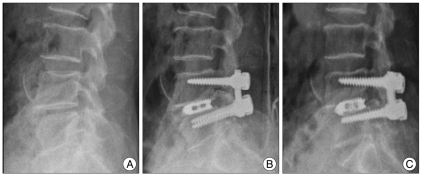
The surgical techniques used for bilateral approach were similar to the unilateral approach except bilateral hemilaminectomy and discectomy were performed (Fig. 1). Each of the two cages was inserted into the disc space through bilateral laminectomy.
Fig. 1.
Computed tomography scans, which were performed postoperatively, show posterior lumbar interbody fusion using two cages via unilateral approach (left partial hemilaminectomy) (A) and via bilateral approach (bilateral partial hemilaminectomy) (B).
Clinical outcome assessment
The postoperative clinical evaluation was based on the VAS and the Oswestry Disability Index (ODI) for back pain and leg pain at multiple time points following surgery. The radiological assessment was carried out with lateral plain radiographs taken preoperatively, immediately postoperatively, 1, 2, 3 and 6 months postoperatively, and at the last follow-up. In some cases, a CT scan was also performed to supplement the plain radiographic findings. The bony union was evaluated with careful assessment of the formation of bone bridging and the absence of radiolucency around the cages. Solid bony union was considered to be obtained when the endplates became invisible on the follow-up radiographs, and the bony trabecular continuity and bone bridging was observed in the intervertebral space. Non-union was defined as disruption of the trabecular continuity or bone bridging, instability on flexion-extension radiographs, over 1 mm radiolucency around the screws and cages, pedicle screw breakage, or showing more than 5 degrees of motion. The measurement of the disc height was based on the corners of adjacent vertebral contour and by averaging the ventral and dorsal disc heights. Intra and postoperative blood loss, length of operation and postoperative hospitalized days were also recorded.
RESULTS
Of the 124 consecutive cases of bilateral PLIF, 80 (65%) were via bilateral approach and 44 (35%) were via unilateral approach. Patients consisted of 49 men and 75 women and mean age was 58.9 years (range, 40-77). The average preoperative disc height was 8.43 mm, ranging from 4.1 to 12.6 mm. The average follow-up duration was 29.5 months, ranging from 12 to 60 months. The indication for surgery was spinal stenosis in 87 cases, herniated disc with instability in 14 cases and spondylolisthesis in 23 cases. Single-level fusion was performed in 111 patients and two-level fusion was performed in 13 patients.
The level of the fusion varied : bilateral approach was performed at L3-4 (11 patients, 13.7%), L4-5 (60 patients, 75%), L5-S1 (2 patients, 2.5µ), L3-4-5 (6 patients, 7.5%) and L4-5-S1 (1 patient, 1.3%), whereas unilateral approach was applied at L3-4 (7 patients, 15.8%), L4-5 (31 patients, 70.7µ), L3-4-5 (4 patients, 9%) and L4-5-S1 (2 patients, 4.5%).
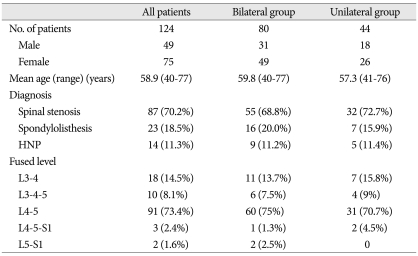
The distribution of age, sex, indications and fused levels were similar between two groups (Table 1).
Table 1.
Demographic and etiologic data in both groups
Clinical results
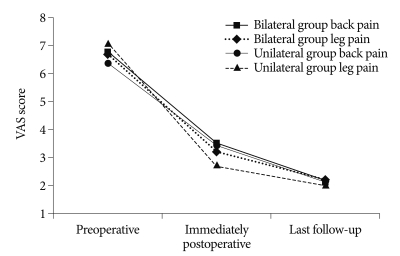
The clinical evaluation showed excellent outcomes in both groups. The VAS score measured preoperatively, immediately postoperatively and at the last follow-up improved significantly (Fig. 2). The ODI scores at the last follow-up were 11.41±3.24 in the bilateral group and 10.56±2.57 in the unilateral group and there were no significant differences between the two groups.
Fig. 2.
The mean VAS scores during the follow-up period in both groups
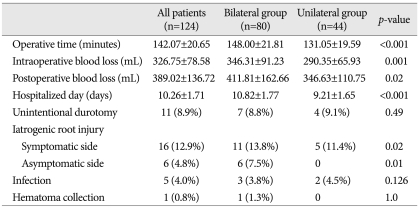
Unintentional durotomy occurred in 7 patients (8.8%) in the bilateral group and in 4 patients (9.1%) in the unilateral group, but subsequent postoperative CSF fistula was not observed. Iatrogenic nerve root dysfunction on the symptomatic side occurred in 11 patients (13.8%) in the bilateral group and 5 patients (11.4%) in the unilateral group, but on the asymptomatic side occurred only in the bilateral group (6 patients), although all cases of nerve root dysfunction were transient and resolved in a few weeks. There was a similar incidence of wound infection between two groups. All the patients safely underwent surgery without severe complications, but one patient underwent reoperation due to disc herniation at the adjacent segment in the unilateral group and one patient required revision in the early postoperative period in the bilateral group due to hematoma causing cauda equine syndrome. No implant migrations or fractures occurred in either group.
The mean operation times in the unilateral group (131.05±19.59 min) were significantly shorter than in the bilateral group (148.00±21.81 min), (p<0.001). The amount of blood loss during the operation in the unilateral group (290.35±65.93 cc) was less than in the bilateral group (346.31±91.23 cc) with significance (p=0.001). The amount of blood loss during the postoperative period in the unilateral group (346.63±110.75 cc) was less than in the bilateral group (411.81±162.66 cc) with significance (p=0.02). The mean hospitalization period in the unilateral group (9.21±1.65 days) was shorter than in the bilateral group (10.82±1.77 days) with significance (p<0.001) (Table 2).
Table 2.
The clinical results and complications in both groups
Radiological results
Solid fusion was observed in 60 cases at 6 months (75%), 70 cases at 12 months (88%) and 95% at last visit in the bilateral group. In the unilateral group, the corresponding fusion rates were 70%, 89% and 95%. No significant difference was observed between the two groups in term of fusion rate. There were no cases of instability in any patient who could not achieve fusion and no instrument failure including cage retropulsion. Radiolucency around the cages and pedicle screw was not observed in any of the patients at the last follow-up (Fig. 3, 4).
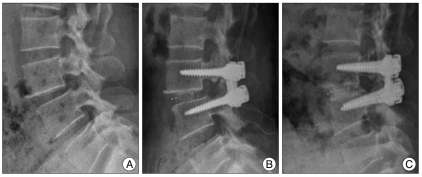
Fig. 3.
A 56 year-old female who presented with lower back pain and right leg pain. A : The preoperative lateral view shows a decreased disc height at L4-5. B : The postoperative immediately checked lateral view shows restoration of the disc height. C : At 13 months after surgery, the lateral view shows solid fusion.
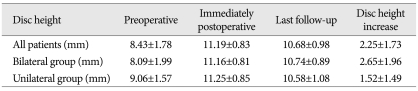
Fig. 4.
A 48 year-old female who presented with longstanding back pain and left leg pain. A : The preoperative lateral view shows spondylolisthesis at L3-4. B : The postoperative immediately checked lateral view shows restoration of the disc height. C : The last follow-up radiograph, 30 months later, shows solid fusion and maintenance of the reduction.
The average intervertebral disc height in the bilateral group significantly improved from 8.09±1.99 mm preoperatively to 11.16±0.81 mm immediately postoperatively to resolve at 10.74±0.89 mm at the last follow-up. In the unilateral group height improved from 9.06±1.57 mm to 11.25±0.85 mm then 10.58±1.08 mm. The disc height after the PLIF procedure was increased significantly in both groups. The mean increase of the intervertebral disc height from the preoperative measurement to the last follow-up measurement in the bilateral group (2.65±1.96 mm) was longer than in the unilateral group (1.52±1.49 mm), with statistical significance between two groups (p=0.001) (Table 3).
Table 3.
Changes of the intervertebral disc height during the follow-up period in both groups
DISCUSSION
Lumbar spinal fusion surgery has been commonly performed for patients who present with chronic back pain with neurological symptoms. A variety of surgical techniques have been developed for lumbar spinal fusion, such as anterior lumbar interbody fusion (ALIF), PLIF, TLIF and posterolateral fusion (PLF). PLF has been widely used for lumbar degenerative disease3), but it carries the risk of musculoligamentous complex injury caused by extensive wide exposure. Furthermore, it cannot restore the disc height, even when additional posterior instrumentation is used10).
Interbody fusion has become a standard surgical technique, because it has the advantages of high fusion rates due to a large surface area for fusion with the graft, relatively lower rates of musculoligamentous injury and early stabilization with the use of posterior instrumentation10,11,20,24,35). Interbody fusion can be achieved through the anterior or posterior approach. Although ALIF has higher fusion rates than PLIF, it may have complications such as iliac vessel injury and retrograde ejaculation5,31,32). Furthermore, there are several reports stating that ALIF should be supplemented with posterior instrumentation for higher fusion rates37).
PLIF has been a commonly performed surgical technique for several decades, since it can restore the disc height and sagittal plane alignment, stabilize the unstable degenerative intervertebral disc and reinforce weight-bearing to the anterior column15). The PLIF procedure has been used for many indications, including spinal stenosis, instability, degenerative disc disease, spondylolisthesis and spondylosis. PLIF using a cage alone has been widely performed, but wide laminectomy with bilateral facetectomy is necessary for cage insertion bilaterally into the disc space and additional posterior pedicle screw fixation should be performed to prevent iatrogenic instability7,25).
Posterior pedicle screw fixation following PLIF can prevent iatrogenic instability but may give rise to an iatrogenic soft tissue injury18). Excessive intraoperative paraspinal muscle exposure can also lead to denervation and atrophy, which results in a failed back syndrome34). In patients with chronic back pain with unilateral leg pain, wide bilateral exposure may produce iatrogenic flat back syndrome or contralateral leg pain, despite the improvement in the ipsilateral leg pain.
However, PLIF without posterior instrumentation can cause various postoperative complications including iatrogenic instability or cage migration. Chen et al.11) reported that lack of posterior instrumentation may contribute to the cage migration. They noted that total facetectomy is also associated with the cage migration.
Decompressive laminectomy or facetectomy to achieve goals of surgical treatment for lumbar spinal degenerative diseases is essential procedure in PLIF technique. However, wide decompressive laminectomy or facetectomy can increase the risk of perioperative or postoperative complications such as prolonged operative time, increased blood loss, or adjacent segment structural instability. Lai et al.23) reported the importance of a tension band mechanism by the posterior column structure as a risk factor for adjacent segment degeneration. They noted that total laminectomy, including removal of the spinous process, supraspinous ligament and interspinous ligament, aggravated the integrity of the posterior complex and lead to the adjacent segment instability. Chen et al.12) also investigated that total laminectomy accompanied with posterior instrumentation is more likely to develop adjacent instability than partial laminectomy in porcine model. Hence, we performed partial laminectomy rather than total laminectomy in both groups. In our study, we did not evaluate about postoperative adjacent segment instability, but we could compare operative time and perioperative blood loss in both groups. Seong et al.33) reported that mean operating time and perioperative blood loss were less in a partial segmental laminectomy group than in a wide laminectomy group. Concerning advantages of the shorter operating time, Motosuneya et al.29) reported that shorter operating time can minimize postoperative back muscle atrophy or persistent back pain. These studies state that extent of laminectomy is associated with perioperative or postoperative complications, mentioned above, and we could have statistically better results in unilateral group, concerning operating time and perioperative blood loss.
Abumi et al.1) found that a unilateral facetectomy produced smaller increases in the motions of flexion and axial rotation and concluded that solid fusion can be achieved by avoiding bilateral facet disruption. However, fusion rate was not significantly different between the two groups in our study.
Currently, the TLIF technique is commonly performed, because it has simpler and safer surgical procedure as the PLIF technique19,38) and many studies report that one cage is enough in PLIF or TLIF. Zhao et al.39) reported that PLIF using a single threaded cage with a supplementary transpedicular screw and rod instrumentation enables sufficient decompression and solid interbody fusion to be achieved. They inserted a single long threaded cage obliquely via a unilateral facetectomy and hemilaminectomy. Molinari et al.28), Fogel et al.17) and Chang et al.8) also reported good results with unilateral cages and showed that patients with a unilateral cage had equal fusion and clinical success compared to those with bilateral cages. The advantages of unilateral TLIF include a lower risk of epidural fibrosis and injury to neural structures related to excessive root retraction26). In our study, however, we used two cages in both groups. We wanted to investigate about advantages of unilateral laminectomy comparing with bilateral laminectomy under the same procedural condition, including bilateral instrumentation and insertion of two cages.
In this retrospective study, the surgical indication was not different between two groups. However, regarding the preoperative disc height and the increase of the disc height, unilateral group had higher preoperative disc height and less increase of the disc height than bilateral group. These results may be caused by selection bias. We assume that unilateral PLIF was performed in a patient with relatively higher disc height to insert cages easily. Therefore, the limitation of this current study is that two groups had different disc heights preoperatively and could not have reliable results about the advantages of the PLIF through unilateral laminectomy. For the reliable comparative study between both groups, prospective study will be necessary.
CONCLUSION
PLIF via a unilateral approach using two cages with bilateral pedicle screw fixation provides good clinical and radiological outcomes comparable to bilateral approach, while minimizing the operative time and perioperative blood loss. However, the different preoperative disc height between two groups is a significant limitation of this study, and prospective study will be necessary for reliable comparative study. Despite this limitation, solid fusion and satisfactory symptomatic improvement could be achieved uniquely by our surgical method. This surgical method can be an alternative surgical technique in patients with chronic degenerative disc disease with unilateral leg pain combined with radiological instability without unnecessary nerve root exposure.
References
- 1.Abumi K, Panjabi MM, Kramer KM, Duranceau J, Oxland T, Crisco JJ. Biomechanical evaluation of lumbar spine stability after graded facectectomies. Spine (Phila Pa 1976) 1990;15:1142–1147. doi: 10.1097/00007632-199011010-00011. [DOI] [PubMed] [Google Scholar]
- 2.Ames CP, Acosta FL, Jr, Chi J, Iyengar J, Muiru W, Acaroglu E, et al. Biomechanical comparison of posterior lumbar interbody fusion and transforaminal lumbar interbody fusion performed at 1 and 2 levels. Spine (Phila Pa 1976) 2005;30:E562–E566. doi: 10.1097/01.brs.0000180505.80347.b1. [DOI] [PubMed] [Google Scholar]
- 3.Axelsson P, Johnsson R, Strömqvist B, Arvidsson M, Herrlin K. Posterolateral lumbar fusion. Outcome of 71 consecutive operations after 4 (2-7) years. Acta Orthop Scand. 1994;65:309–314. doi: 10.3109/17453679408995459. [DOI] [PubMed] [Google Scholar]
- 4.Bagby GW. Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics. 1988;11:931–934. doi: 10.3928/0147-7447-19880601-13. [DOI] [PubMed] [Google Scholar]
- 5.Beaubien BP, Derincek A, Lew WD, Wood KB. In vitro, biomechanical comparison of an anterior lumbar interbody fusion with an anteriorly placed, low-profile lumbar plate and posteriorly placed pedicle screws or translaminar screws. Spine (Phila Pa 1976) 2005;30:1846–1851. doi: 10.1097/01.brs.0000174275.95104.12. [DOI] [PubMed] [Google Scholar]
- 6.Briggs H, Miligan PR. Chip fusion of the low back following exploration of the spinal canal. J Bone Joint Surg Am. 1944;26:125–130. [Google Scholar]
- 7.Carmouche JJ, Molinari RW. Epidural abscess and discitis complicating instrumented posterior lumbar interbody fusion : a case report. Spine (Phila Pa 1976) 2004;29:E542–E546. doi: 10.1097/01.brs.0000146802.38753.38. [DOI] [PubMed] [Google Scholar]
- 8.Chang TS, Chang JH, Wang CS, Chen HY, Cheng CW. Evaluation of unilateral cage-instrumented fixation for lumbar spine. J Orthop Surg Res. 2010;5:86. doi: 10.1186/1749-799X-5-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen HH, Cheung HH, Wang WK, Li A, Li KC. Biomechanical analysis of unilateral fixation with interbody cages. Spine (Phila Pa 1976) 2005;30:E92–E96. doi: 10.1097/01.brs.0000153703.80747.16. [DOI] [PubMed] [Google Scholar]
- 10.Chen L, Tang T, Yang H. Complications associated with posterior lumbar interbody fusion using Bagby and Kuslich method for treatment of spondylolisthesis. Chin Med J (Engl) 2003;116:99–103. [PubMed] [Google Scholar]
- 11.Chen L, Yang H, Tang T. Cage migration in spondylolisthesis treated with posterior lumbar interbody fusion using BAK cages. Spine (Phila Pa 1976) 2005;30:2171–2175. doi: 10.1097/01.brs.0000180402.50500.5b. [DOI] [PubMed] [Google Scholar]
- 12.Chen LH, Lai PL, Tai CL, Niu CC, Fu TS, Chen WJ. The effect of interspinous ligament integrity on adjacent segment instability after lumbar instrumentation and laminectomy--an experimental study in porcine model. Biomed Mater Eng. 2006;16:261–267. [PubMed] [Google Scholar]
- 13.Chiang MF, Zhong ZC, Chen CS, Cheng CK, Shih SL. Biomechenical comparison of instrumented posterior lumbar interbody fusion with one or two cages by finite element analysis. Spine (Phila Pa 1976) 2006;31:E682–E689. doi: 10.1097/01.brs.0000232714.72699.8e. [DOI] [PubMed] [Google Scholar]
- 14.Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg. 1953;10:154–168. doi: 10.3171/jns.1953.10.2.0154. [DOI] [PubMed] [Google Scholar]
- 15.Diedrich O, Luring C, Pennekamp PH, Perlick L, Wallny T, Kraft CN. [Effect of posterior lumbar interbody fusion on the lumbar sagittal spinal profile] Z Orthop Ihre Grenzgeb. 2003;141:425–432. doi: 10.1055/s-2003-41561. [DOI] [PubMed] [Google Scholar]
- 16.Elias WJ, Simmons NK, Kaptain GJ, Chadduck JB, Whitehill JB, Whitehill R. Complications of posterior lumbar interbody fusion when using a titanium threaded cage device. J Neurosurg. 2000;93:45–52. doi: 10.3171/spi.2000.93.1.0045. [DOI] [PubMed] [Google Scholar]
- 17.Fogel GR, Toohey JS, Neidre A, Brantigan JW. Is one cage enough in posterior lumbar interbody fusion : a comparison of unilateral single cage interbody fusion to bilateral cages. J Spinal Disord Tech. 2007;20:60–65. doi: 10.1097/01.bsd.0000211251.59953.a4. [DOI] [PubMed] [Google Scholar]
- 18.Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine : preliminary clinical results. J Neurosurg. 2002;97:7–12. doi: 10.3171/spi.2002.97.1.0007. [DOI] [PubMed] [Google Scholar]
- 19.Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U. Transforaminal lumbar interbody fusion : a safe technique with satisfactory three to five year results. Eur Spine J. 2005;14:551–558. doi: 10.1007/s00586-004-0830-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hitchon PW, Goel V, Rogge T, Dooris A, Drake J, Torner J. Spinal stability with anterior or posterior ray threaded fusion cages. J Neurosurg. 2000;93:102–108. doi: 10.3171/spi.2000.93.1.0102. [DOI] [PubMed] [Google Scholar]
- 21.Kettler A, Schmoelz W, Kast E, Gottwald M, Claes L, Wilke HJ. In vitro stabilizing effect of a transforaminal compared with two posterior lumbar interbody fusion cages. Spine (Phila Pa 1976) 2005;30:E665–E670. doi: 10.1097/01.brs.0000186466.01542.8c. [DOI] [PubMed] [Google Scholar]
- 22.Kim YB, Park SW, Hwang SN, Choi DY. The effect of additional transpedicular instrumentation for patients with symptomatic degenerative spondylosis with instability treated with posterior lumbar interbody fusion using autologous iliac bone dowels. J Korean Neurosurg Soc. 2002;32:102–106. [Google Scholar]
- 23.Lai PL, Chen LH, Niu CC, Fu TS, Chen WJ. Relation between laminectomy and development of adjacent segment instability after lumbar fusion with pedicle fixation. Spine (Phila Pa 1976) 2004;29:2527–2532. doi: 10.1097/01.brs.0000144408.02918.20. discussion 2532. [DOI] [PubMed] [Google Scholar]
- 24.Lin PM. Posterior lumbar interbody fusion technique : complications and pitfalls. Clin Orthop Relat Res. 1985:90–102. [PubMed] [Google Scholar]
- 25.Lin PM. Posterior lumbar interbody fusion (PLIF) : past, present, and future. Clin Neurosurg. 2000;47:470–482. [PubMed] [Google Scholar]
- 26.Lowe TG, Tahernia AD. Unilateral transforaminal posterior lumbar interbody fusion. Clin Orthop Relat Res. 2002:64–72. doi: 10.1097/00003086-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Mehta VA, McGirt MJ, Garcés Ambrossi GL, Parker SL, Sciubba DM, Bydon A, et al. Trans-foraminal versus posterior lumbar interbody fusion : comparison of surgical morbidity. Neurol Res. 2011;33:38–42. doi: 10.1179/016164110X12681290831289. [DOI] [PubMed] [Google Scholar]
- 28.Molinari RW, Sloboda J, Johnstone FL. Are 2 cages needed with instrumented PLIF? A comparison of 1 versus 2 interbody cages in a military population. Am J Orthop. 2003;32:337–343. discussion 343. [PubMed] [Google Scholar]
- 29.Motosuneya T, Asazuma T, Tsuji T, Watanabe H, Nakayama Y, Nemoto K. Postoperative change of the cross-sectional area of back musculature after 5 surgical procedures as assessed by magnetic resonance imaging. J Spinal Disord Tech. 2006;19:318–322. doi: 10.1097/01.bsd.0000211205.15997.06. [DOI] [PubMed] [Google Scholar]
- 30.Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Posterior interbody fusion : a retrospective study of complications after facet joint excision and pedicle screw fixation in 148 cases. Acta Orthop Scand. 1999;70:329–334. doi: 10.3109/17453679908997819. [DOI] [PubMed] [Google Scholar]
- 31.Sasso RC, Best NM, Mummaneni PV, Reilly TM, Hussain SM. Analysis of operative complications in a seriese of 471 anterior lumbar interbody fusion procedures. Spine (Phila Pa 1976) 2005;30:670–674. doi: 10.1097/01.brs.0000155423.18218.75. [DOI] [PubMed] [Google Scholar]
- 32.Sasso RC, Kenneth Burkus J, LeHuec JC. Retrograde ejaculation after anterior lumbar interbody fusion : transperitoneal versus retroperitoneal exposure. Spine (Phila Pa 1976) 2003;28:1023–1026. doi: 10.1097/01.BRS.0000062965.47779.EB. [DOI] [PubMed] [Google Scholar]
- 33.Seong YJ, Lee JS, Suh KT, Kim JI, Lim JM, Goh TS. Posterior decompression and fusion in patients with multilevel lumbar foraminal stenosis : a comparison of segmental decompression and wide decompression. Asian Spine J. 2011;5:100–106. doi: 10.4184/asj.2011.5.2.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sihvonen T, Herno A, Paljärvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine (Phila Pa 1976) 1993;18:575–581. doi: 10.1097/00007632-199304000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Tencer AF, Hampton D, Eddy S. Biomechanical properties of threaded inserts for lumbar interbody spinal fusion. Spine (Phila Pa 1976) 1995;20:2408–2414. doi: 10.1097/00007632-199511001-00007. [DOI] [PubMed] [Google Scholar]
- 36.Vaccaro AR, Albert TJ. Spine surgery : Tricks of the trade. New York: Thieme; 2009. pp. 65–66. [Google Scholar]
- 37.Wang JM, Kim DJ, Yun YH. Posterior pedicular screw instrumentation and anterior interbody fusion in adult lumbar spondylolysis or grade I spondylolisthesis with segmental instability. J Spinal Disord. 1996;9:83–88. [PubMed] [Google Scholar]
- 38.Yan DL, Pei FX, Li J, Soo CL. Comparative study of PLIF and TLIF treatment in adult degenerative spondylolisthesis. Eur Spine J. 2008;17:1311–1316. doi: 10.1007/s00586-008-0739-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhao J, Hou T, Wang X, Ma S. Posterior lumbar interbody fusion using one diagonal fusion cage with transpedicular screw/rod fixation. Eur Spine J. 2003;12:173–177. doi: 10.1007/s00586-001-0376-4. [DOI] [PMC free article] [PubMed] [Google Scholar]