Abstract
A 40-years-old male patient reported to our department with a chief complaint of persistent palatal fluid discharge and large depressed forehead defect. He gave a history of trauma 20 months back due to head on collision to electric pole and underwent surgery twice for open reduction and fixation of facial skeletal fractures. After 9 months of surgery again a third surgery was performed for the removal of frontal bone due to infection and osteomyelitis at the same site. Extra-oral examination revealed a large fronto-cranial defect extending from superior border of frontal bone to supra-orbital margins bilaterally in length, and from frontal right lateral to frontal left lateral side in width, measuring 8.0 cm in length, 10.5 cm in width and 1.5 to 2.0 cm in depth. Intra-oral sinus fluid discharge was from left posterior palatal region. Preoperative CT was taken and reconstruction of fronto-cranial defect was successfully performed with bone cement. Alloplastic implant reconstruction achieved an excellent esthetic result without any complications.
Keywords: Cranial defect, Reconstruction, Intra-oral sinus, Fluid discharge, Frontocranial defect
Introduction
Cranial defects occur most frequently during road traffic accident as a result of accident makes knowledge of cranioplasty. Trauma accounts for most of the cranial defects numerous alloplastic materials have been historically employed for the restoration of cranial defects with varying degrees of success. For a long time cranial defects resulting from trauma or disease have been described. Since the end of nineteenth century, numerous repair procedures have been described and advocated.
Cold polymerized methyl-methacrylate alloplastic cranial implant restored the defect with great success. In this study, a case report has been presented in which self-cure acrylic resin alloplastic implant material used to reconstruct the frontal bone defect.
Case Report
A 40 year old patient reported to our department with a chief complaint of persistent palatal fluid discharge due to history of trauma 20 months back resulting from a head on collision with an electrical pole. He underwent surgery thrice, and the third time the frontal bone was removed due to osteomyelitis 9 months back (Figs. 1, 2, 3, 4, 5, 6, 7, 8, 9).
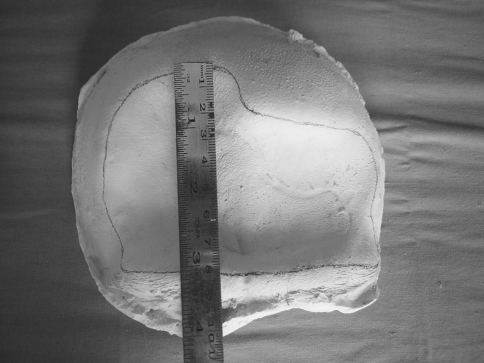
Fig. 1.
Pre-op right lateral view
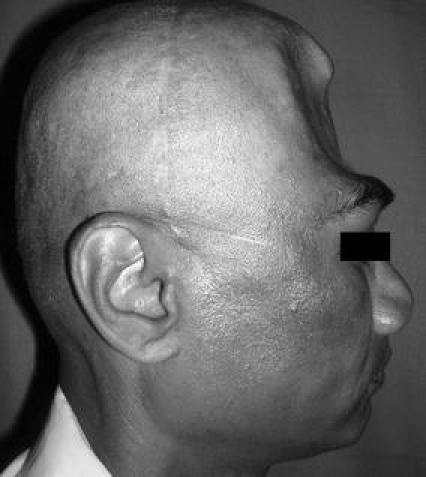
Fig. 2.
Pre-op frontal 3D scan
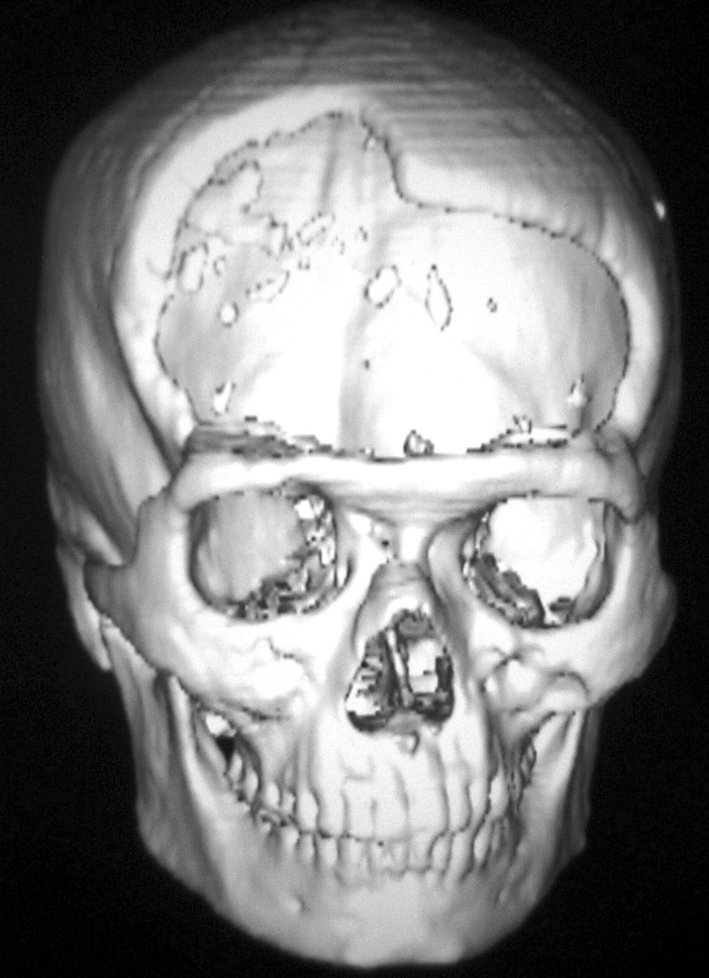
Fig. 3.
Pre-op defect height
Fig. 4.
Retraction of flap
Fig. 5.
PMMA cold cure resin-bone cement
Fig. 6.
Ab-Gel adaptation
Fig. 7.
Reconstruction with PMMA resin over Ab-Gel
Fig. 8.
Post-op lateral view of skull—after 6 months
Fig. 9.

Post-op frontal view—after 6 months
Patient was healthy with the vital signs within normal limits. Extra-oral examination revealed a large fronto-cranial defect extending from superior border of frontal bone to supra-orbital margins bilaterally in length, and from frontal right lateral to frontal left lateral side in width, measuring 8.0 cm in length, 10.5 cm in width and 1.5 to 2.0 cm in depth. Intra-oral sinus fluid discharge from left posterior palatal region was observed.
Based on the history and clinical presentation routine radiographs were advised. Posteroanterior view and lateral skull radiographs revealed large radiolucent defect.
For the detailed study coronal, axial sections and 3D-CT reconstruction was advised which revealed large fronto-cranial defect. Patient was admitted and prepared for the surgery under general anesthesia for the reconstruction. Routine blood investigations with consent of the physician, anesthetist and neurosurgeon were taken.
Case was planned and done for reconstruction of large fronto-cranial bone defect with bone cement (Surgical Simplex—Radiopaque Poly-Methylmethacrylate auto-polymerised resin material (PMMA)) through bicoronal incision approach along with closure of palatal sinus defect.
After 6 months posteroanterior and lateral views of skull were advised as follow-up. Excellent adaptation was seen both clinically and radiographically.
Discussion
Various acrylic resin materials have been utilized as bone substitutes in dentistry, neurosurgery, and orthopedic surgery. These materials have been used successfully for chin implants, facial deformities, mandibular defects, orbital repairs, and temporomandibular joint interpositional arthroplasty [1]. Alloplastic cranioplasty can be successfully performed with a variety of different materials [2]. General indications of for cranioplasty include (1) pulsating and painful defects, (2) danger of trauma at the site of the defect, (3) deforming and unsightly defects, (4) headache and other symptoms such as pain, apprehension, or tenderness at the site of the defect [3]. The result of this study indicate that cranioplasty is compatible with tissues [1].
Complications such as swelling and infection [5], headache, implant mobilization, drooping of the implant, bitemporal hemianopia and third nerve palsy were not seen in this case postoperatively during the follow-up period of 6 months [4, 5].
Conclusion
Cranioplasty can be successfully performed with self-cure PMMA material which offers inexpensive method that is easily adapted and contoured intraoperatively to a defect of any size defect and provides great impact on resistance and it does not integrate into the surrounding tissues.
References
- 1.Miller GP, Hinkle S, Narang R. Comparative biologic responses to various methyl methacrylate bone substitutes. J Prosthet Dent. 1976;36(1):95–100. doi: 10.1016/0022-3913(76)90239-0. [DOI] [PubMed] [Google Scholar]
- 2.Bone Cements- Orthopedics Quick Pick- Medcompare
- 3.Martin JW, Ganz SD, King GE, Jacob RF, Kramer DC. Cranial implant modification. J Prosthet Dent. 1984;52(3):414–416. doi: 10.1016/0022-3913(84)90457-8. [DOI] [PubMed] [Google Scholar]
- 4.Kumar S, Gupta S, Prabhu N. Reconstruction of a cranial defect with an alloplastic implant. J Ind Prosth Soc. 2007;7(3):150–152. doi: 10.4103/0972-4052.37680. [DOI] [Google Scholar]
- 5.Sabin H. Cranial implant problems. J Prosthet Dent. 1975;34(6):659–665. doi: 10.1016/0022-3913(75)90064-5. [DOI] [PubMed] [Google Scholar]