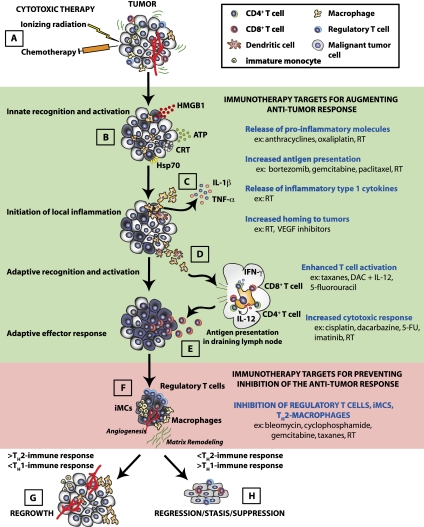
Figure 1.
Schematic of immune response pathways induced following cytotoxic therapy. Traditional cytotoxic therapies (e.g., CTX and RT) trigger an immune response in tissues (A), leading to the release of inflammatory mediators (including HMGB1, calreticulin, ATP, and Hsp70) from tumor cells (B). (C) These molecules activate resident immune cells such as DCs and tissue macrophages through cognate receptors, including TLR4 and P2RX7, which triggers the release of TNF-α and IL-1, which further recruits peripheral blood leukocytes (PBLs) from the circulation. (D) Activation of resident DCs and tissue macrophages stimulates their migration to the lymphoid tissue bearing tumor antigens. In the lymphoid tissue, the DCs and macrophages present antigen to CD4+ and CD8+ T cells, leading to their activation. (E) Activated CD4+ and CD8+ T cells then re-enter the circulation and return to the tumor to eliminate tumor cells. (F) Throughout this process, a portion of the PBLs recruited from the circulation into the tumor also possess suppressive function (e.g., Treg cells and various subtypes of myeloid cells), and these become increasingly dominant as the tumor is cleared by a cytotoxic response (primarily CD8+ T cells and NK cells) and function to reduce the anti-tumor cytotoxic response by a diverse array of mechanisms. (H) If the malignant cells are completely eradicated, the tissue can return to a normal, homeostatic state. (G) However, if incomplete eradication of malignant cells occurs, then, over time, tumor regrowth is evident in the form of recurrent disease at the primary site or metastases at distal sites. Events in the immune response that might serve as targets to enhance the immune response (shaded green) or prevent suppression of the immune response (shaded red) are outlined on the right with examples of cytotoxic agents that can mediate each of these events.