Abstract
Background
Periprocedural treatment with high-dose statins is known to have cardioprotective and pleiotropic effects, such as anti-thrombotic and anti-inflammatory actions. We aimed to assess the efficacy of high-dose rosuvastatin loading in patients with stable angina undergoing off-pump coronary artery bypass grafting (OPCAB).
Materials and Methods
A total of 142 patients with stable angina who were scheduled to undergo surgical myocardial revascularization were randomized to receive either pre-treatment with 60-mg rosuvastatin (rosuvastatin group, n=71) or no pre-treatment (control group, n=71) before OPCAB. The primary endpoint was the 30-day incidence of major adverse cardiac events (MACEs). The secondary endpoint was the change in the degree of myocardial ischemia as evaluated with creatine kinase-myocardial band (CK-MB) and troponin T (TnT).
Results
There were no significant intergroup differences in preoperative risk factors or operative strategy. MACEs within 30 days after OPCAB occurred in one patient (1.4%) in the rosuvastatin group and four patients (5.6%) in the control group, respectively (p=0.37). Preoperative CK-MB and TnT were not different between the groups. After OPCAB, the mean maximum CK-MB was significantly higher in the control group (rosuvastatin group 10.7±9.75 ng/mL, control group 14.6±12.9 ng/mL, p=0.04). Furthermore, the mean levels of maximum TnT were significantly higher in the control group (rosuvastatin group 0.18±0.16 ng/mL, control group 0.39±0.70 ng/mL, p=0.02).
Conclusion
Our findings suggest that high-dose rosuvastatin loading before OPCAB surgery did not result in a significant reduction of 30-day MACEs. However, high-dose rosuvastatin reduced myocardial ischemia after OPCAB.
Keywords: Off-pump, Coronary artery bypass, Statin
INTRODUCTION
Reduction of plasma cholesterol, particularly cholesterol transported in low-density lipoproteins (LDL), lowers the risk of primary and secondary cardiovascular events. 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase inhibitors, commonly known as statins, can produce significant reductions in cholesterol. It is well known that the beneficial effect of statins on coronary events is related to their hypocholesterolemic properties. However, the immediate product of HMG-CoA reductase, mevalonic acid, is not only a substrate for cholesterol synthesis but also a precursor of isoprenoids and other metabolites involved in different cellular pathways of atherogenesis and thrombosis [1]. As a consequence, statins may result in pleiotropic effects that are independent of cholesterol reduction, which may explain many of the direct anti-atherosclerotic and anti-thrombotic properties of these compounds [1-6].
The ARMYDA (Atorvastatin for Reduction of Myocardial Damage During Angioplasty) trial [7] has shown that a 7-day pretreatment with atorvastatin is associated with an 81% reduction in the risk of periprocedural myocardial infarction in patients with stable angina undergoing elective percutaneous coronary intervention (PCI). Attenuation of endothelial activation may explain this protective role at least in part [8], and preprocedural loading with atorvastatin may even improve outcomes in patients with acute coronary syndrome undergoing early invasive intervention [9].
Recently, statins were shown to be independently associated with a reduced risk of postoperative mortality in patients undergoing major, noncardiac vascular surgery [10]. Furthermore, preoperative statin therapy has been independently associated with a significant reduction in the risk of all-cause mortality in patients undergoing coronary artery bypass grafting (CABG) surgery [11-13]. However, patients were treated with different types of statins and variable doses, and the duration of previous treatment was unknown. Additionally, these findings have not been validated in a randomized trial, and most patients in these studies underwent CABG using cardiopulmonary bypass.
Avoiding the systemic inflammatory response that may result from cardiopulmonary bypass, off-pump coronary bypass grafting (OPCAB) is known to have benefits in high-risk patients. The anti-inflammatory and pleiotropic effects of statins and their effects on clinical outcomes for patients who undergo the OPCAB procedure have not been described. The aim of the current study was to determine whether preoperative rosuvastatin loading is independently associated with reduced myocardial ischemia and clinical outcomes in patients with stable angina undergoing isolated OPCAB.
MATERIALS AND METHODS
1) Study population and design
This trial was a single-center, randomized, prospective trial performed at our hospital. Inclusion criteria were the presence of stable angina, age between 18 and 80 years, and a need for isolated surgical myocardial revascularization. Exclusion criteria were evidence of recent myocardial infarction and unstable angina, emergent or urgent operation, history of prior cardiac surgery, any increase in liver enzymes, renal failure with serum creatinine >3 mg/dL, left ventricular ejection fraction <35%, and history of liver or muscle disease. From October 2007 to December 2008, a total of 214 patients who met the inclusion criteria were initially evaluated; 7 patients were excluded because of previous cardiac surgery, 15 for increased liver enzymes, 16 for renal failure with creatinine >3 mg/dL, 19 for low ejection fraction, 5 for history of liver disease, and 10 for refusal to participate in the study. Eligible patients (n=142) were randomized to receive rosuvastatin (40 mg loading dose 12 hours before surgery and a second 20 mg dose 2 hours before surgery) or no pretreatment (control group). Patients were assigned in a 1 : 1 ratio using a computer-generated randomization sequence. This study protocol was approved by the Institutional Review Board of Yonsei University College of Medicine and individual patient consent was obtained.
2) Operative technique
We have previously described the operative technique and graft strategy [14,15]. The operation was performed through a full sternotomy incision or minimal incision through the left fifth intercostal space, and the left internal mammary artery was harvested in a semi-skeletonized fashion. The second choice of graft was the radial artery, which was harvested with a harmonic scalpel (Ethicon Endosurgery Inc., Cincinnati, OH). The right internal mammary artery, saphenous vein, or right gastroepiploic artery was also harvested if necessary. Heparin (0.7~1.0 mg/kg) was administered to achieve a target activated clotting time (≥300 seconds) before ligation of the distal internal mammary artery. Target arteries were stabilized with a tissue stabilizer and heart positioner. During anastomosis, blood was removed from the arteriotomy sites with a misted carbon dioxide blower and irrigation with warm saline. After surgery, patients were transferred to the intensive care unit and managed as usual.
3) Cardiac enzyme assay
In all patients, blood samples were collected before OPCAB and at 24, 48, and 72 hours after OPCAB to determine the levels of creatine kinase-myocardial band (CK-MB) isoenzyme and troponin-T. Normal limits of CK-MB and troponin T were defined as ≤5 ng/mL and <0.1 µg/L, respectively.
4) Data collection and definition of terms
Preoperative, intraoperative, and postoperative data were collected prospectively from the registry database, medical notes, and medical charts. Detailed data were collected on the admission when cardiac surgery was performed. Complete revascularization was defined as the placement of at least one graft onto each of the three major vascular regions that exhibited stenosis of more than 50% of diameter [16,17]. Perioperative MI was defined as an increase in biomarkers greater than 5 times the 99th percentile of the upper reference limit (URL) plus one of the following: either new pathological Q waves or new LBBB, angiographically documented new graft or native coronary artery occlusion, or imaging evidence of new loss of viable myocardium [18]. Other variables were defined according to the Society of Thoracic Surgeons Adult Cardiac Database Definition of Terms version 2.61 (http://www.sts.org/documents/pdf/AdultCVDataSpecifications2.61.pdf).
5) Endpoints
The primary endpoint was the occurrence of major adverse cardiac events (MACEs), which included the following: death from all causes, non-fatal myocardial infarction (MI), and repeat revascularization by percutaneous intervention or bypass surgery within 30 days after the operation. The secondary endpoint was the difference in the degree of myocardial ischemia between the two groups after OPCAB. The degree of myocardial ischemia was measured by the highest level of cardiac enzymes after OPCAB.
6) Statistical analysis
Categorical variables were expressed as mean±standard deviation (SD). Categorical variables were compared by χ2 test or Fisher's exact test. A Student's t-test was used to compare continuous variables for normal distribution; otherwise, the Mann-Whitney U test was used. Data were analyzed using SPSS for Windows, version 15.0 (SPSS, Inc, Chicago, IL). p-values equal to or less than 0.05 indicated a significant difference, and all p-values were two-tailed.
RESULTS
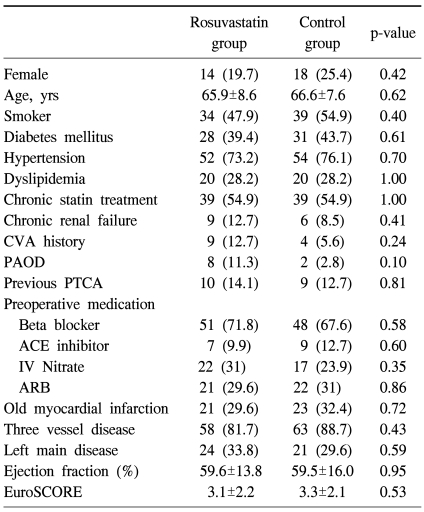
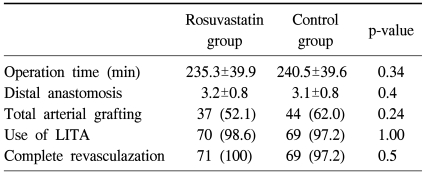
Seventy-one patients were allocated to each group. Patient demographics and baseline clinical characteristics are displayed in Table 1. The two groups were similar in regards to the following: age; prevalence of females; smoking status; prevalence of diabetes mellitus, hypertension, dyslipidemia chronic renal failure, and peripheral arterial obstructive disease; chronic statin treatment for more than one month; history of cerebrovascular accidents and percutaneous transluminal coronary angioplasty; medication use; degree of coronary artery disease; and left ventricular ejection fraction. Preoperative risk, as assessed by EuroSCORE, was not significantly different between the groups (rosuvastatin group 3.1±2.2, control group 3.3±2.1, p=0.53). There were no significant differences in the duration of the operation, number of distal anastomosis, total arterial grafting, or complete revascularization (Table 2).
Table 1.
Demographics and baseline clinical characteristics
CVA=Cerebrovascular accident; PAOD=Peripheral artery obstructive disease; PTCA=Percutaneous transluminal coronary angioplasty; ACE=Angiotensin converting enzyme; IV=Intravenous; ARB=Angiotensin II receptor blocker; EuroSCORE=European system for cardiac operative risk evaluation.
Table 2.
Operative data
LITA=Left internal thoracic artery.
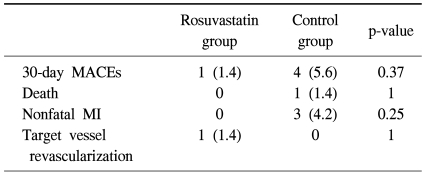
The primary endpoint was evaluated at 30 days (Table 3). The composite primary endpoint of death, myocardial infarction, and target vessel revascularization occurred in 3.5% of patients (5 of 142), one patient (1.4%) in the rosuvastatin group and four patients (5.6%) in the control group. No significant difference was found between groups in overall (p=0.37) or individual cardiac events. One patient with chronic renal failure died in the control group due to the aggravation of renal and respiratory failure.
Table 3.
Incidence of the primary endpoint
MACEs=Major adverse cardiac events; MI=Myocardial infarction.
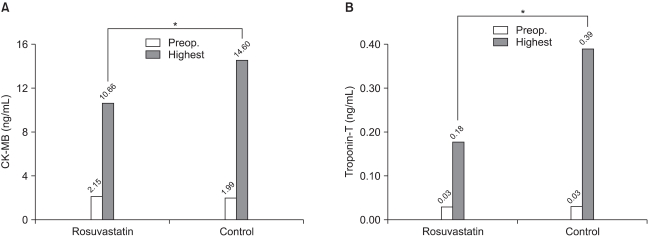
Changes in cardiac enzymes are displayed in Fig. 1. Preoperative CK-MB and troponin T were not different between groups (CK-MB, rosuvastatin group 2.15±0.85 ng/mL, control group 1.99±0.76 ng/mL, p=0.24; troponin T, rosuvastatin group 0.03±0.07 ng/mL, control group 0.03±0.09 ng/mL, p=0.52). After OPCAB, the mean maximum CK-MB was significantly higher in the control group (rosuvastatin group 10.7±9.75 ng/mL, control group 14.6±12.9 ng/mL, p=0.04). Furthermore, the levels of the mean maximum troponin T were significantly higher in the control group (rosuvastatin group 0.18±0.16 ng/mL, control group 0.39±0.70 ng/mL, p=0.02). In the rosuvastatin group, CK-MB decreased by 26.7% and troponin T decreased by 53.8% compared to the control group.
Fig. 1.
Changes in cardiac enzymes after operation. (A) Change in the level of CK-MB. (B) Change in the level of troponin T. Preop=Preoperative level (white bar); Highest=Highest level at postoperative period (gray bar). *=p-value<0.05.
DISCUSSION
This study is the first single-center randomized trial to evaluate the efficacy of high-dose rosuvastatin loading (60 mg) before OPCAB in patients with stable angina. At the 1-month clinical follow-up assessment, the occurrence of major cardiac events was not significantly different between the control and 60-mg rosuvastatin pretreatment groups. However, our study suggests that high-dose rosuvastatin loading before OPCAB may decrease myocardial ischemia as determined by CK-MB and troponin T after OPCAB.
The benefit of periprocedural treatment with statins in on-pump CABG is well established. In the Multicenter Study of Perioperative Ischemia (McSPI) Epidemiology II Study [13], the authors reported that preoperative statin therapy was independently associated with a significant reduction in the risk of early cardiac death after elective on-pump CABG, but was not associated with a reduced risk of postoperative non-fatal, in-hospital MI. Powell et al. [19] evaluated the influence of lipid-lowering therapy for 30 days before CABG. In this observational study with 4,739 patients, in-hospital mortality was significantly lower in the lipid-lowering therapy group than in the nonlipid-lowering therapy group (1.4% vs. 2.2%, odds ratio 0.62, 95% CI 0.40~0.96, p=0.03). Even though the multivariable model demonstrated a loss of statistical significance for the effect of lipid-lowering therapy on in-hospital mortality, they suggested that patient risk factors and the use of other cardioprotective medications associated with the use of preoperative lipid-lowering therapy appeared to explain the association with improved survival. Several prospective trials have been conducted to validate these findings of statin pre-treatment in PCI and CABG settings. In the ARMYDA-ACS trial [9], short-term atorvastatin loading conferred an 88% risk reduction in 30-day MACEs in patients with acute coronary syndrome before PCI. Mannacio et al. evaluated the effect of 20 mg/d rosuvastatin pretreatment for 1 week before on-pump CABG. Troponin I, myoglobin, and CK-MB mass values were assessed, and all biological markers were significantly lower in the rosuvastatin pretreatment group. However, few studies have evaluated statin pretreatment in OPCAB patients. Song et al. [20] reported that preoperative loading with atorvastatin for 3 days before OPCAB significantly reduced the occurrence of postoperative atrial fibrillation.
A total of 60 mg rosuvastatin was loaded before OPCAB in this study. According to a well-reviewed paper [21] about pre-procedural statin therapy, the loading dosages of various statins before PCI or CABG were mostly determined by researchers. In our preliminary study, 40 mg rosuvastatin loading 12 hours before OPCAB did not result in significant decreases of cardiac enzymes and inflammatory markers. 20 mg of rosuvastatin were added 2 hours before OPCAB, and no serious side effects of 60 mg rosuvastatin loading were found.
This study found no significant reduction in 30-day MACEs. The effects of high-dose rosuvastatin loading in this study could not be determined because the incidence of clinical events was low in both patient groups. However, there was a tendency toward a lower number of MACEs in the rosuvastatin loading group and further study with more patients is warranted.
In this study, statin loading before OPCAB significantly lowered the degree of myocardial ischemia as assessed by cardiac enzymes. Although these beneficial effects of statin loading on myocardial protection cannot be completely explained, this early protective effect of statins is unlikely to be the result of its effect on cholesterol. Instead, statins exert pleiotropic effects that may be initiated before its lipid-lowering effects [22]. Previous studies show the improvement of myocardial ischemia after OPCAB that we observed in this study. Protection from aggravation of myocardial ischemia may result from the pleiotropic effects of statins, such as the improvement of endothelial function, dilatation of coronary microvessels, anti-thrombotic effects, and anti-inflammatory action [23,24].
Our study had several limitations. First, two surgeons from a single center conducted the trial. Second, myocardial ischemia was only assessed by CK-MB and troponin T, which may have lower specificity in certain conditions, such as renal dysfunction. Third, sample size was relatively small with low clinical morbidity and mortality, and accordingly, a statistical difference may not have been detected. These factors should be addressed using larger cohorts in multicenter trials that evaluate the effects of statin loading before OPCAB surgery.
CONCLUSION
Our findings suggest that high-dose rosuvastatin loading before OPCAB surgery did not result in a significant reduction of 30-day MACEs. However, high-dose rosuvastatin reduced myocardial ischemia after OPCAB.
Footnotes
This work was supported by the Korea Research Foundation Grant, funded by the Korean Government (MOEHRD, Basic Research Promotion Fund) (KRF-2008-331-E00198).
References
- 1.Goldstein JL, Brown MS. Regulation of the mevalonate pathway. Nature. 1990;343:425–430. doi: 10.1038/343425a0. [DOI] [PubMed] [Google Scholar]
- 2.Bernini F, Didoni G, Bonfadini G, Bellosta S, Fumagalli R. Requirement for mevalonate in acetylated LDL induction of cholesterol esterification in macrophages. Atherosclerosis. 1993;104:19–26. doi: 10.1016/0021-9150(93)90172-q. [DOI] [PubMed] [Google Scholar]
- 3.Corsini A, Mazzotti M, Raiteri M, et al. Relationship between mevalonate pathway and arterial myocyte proliferation: in vitro studies with inhibitors of HMG-CoA reductase. Atherosclerosis. 1993;101:117–125. doi: 10.1016/0021-9150(93)90107-6. [DOI] [PubMed] [Google Scholar]
- 4.Grunler J, Ericsson J, Dallner G. Branch-point reactions in the biosynthesis of cholesterol, dolichol, ubiquinone and prenylated proteins. Biochimica et Biophysica Acta. 1994;1212:259–277. doi: 10.1016/0005-2760(94)90200-3. [DOI] [PubMed] [Google Scholar]
- 5.Corsini A, Raiteri M, Soma MR, Bernini F, Fumagalli R, Paoletti R. Pathogenesis of atherosclerosis and the role of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors. Am J Cardiol. 1995;76:21A–28A. doi: 10.1016/s0002-9149(05)80011-6. [DOI] [PubMed] [Google Scholar]
- 6.Bellosta S, Ferri N, Arnaboldi L, Bernini F, Paoletti R, Corsini A. Pleiotropic effects of statins in atherosclerosis and diabetes. Diabetes Care. 2000;23(Suppl 2):B72–B78. [PubMed] [Google Scholar]
- 7.Pasceri V, Patti G, Nusca A, Pristipino C, Richichi G, Di Sciascio G. Randomized trial of atorvastatin for reduction of myocardial damage during coronary intervention: results from the ARMYDA (Atorvastatin for Reduction of MYocardial Damage during Angioplasty) study. Circulation. 2004;110:674–678. doi: 10.1161/01.CIR.0000137828.06205.87. [DOI] [PubMed] [Google Scholar]
- 8.Patti G, Chello M, Pasceri V, et al. Protection from procedural myocardial injury by atorvastatin is associated with lower levels of adhesion molecules after percutaneous coronary intervention: results from the ARMYDA-CAMs (Atorvastatin for Reduction of MYocardial Damage during Angioplasty-Cell Adhesion Molecules) substudy. J Am Coll Cardiol. 2006;48:1560–1566. doi: 10.1016/j.jacc.2006.06.061. [DOI] [PubMed] [Google Scholar]
- 9.Patti G, Pasceri V, Colonna G, et al. Atorvastatin pretreatment improves outcomes in patients with acute coronary syndromes undergoing early percutaneous coronary intervention: results of the ARMYDA-ACS randomized trial. J Am Coll Cardiol. 2007;49:1272–1278. doi: 10.1016/j.jacc.2007.02.025. [DOI] [PubMed] [Google Scholar]
- 10.Poldermans D, Bax JJ, Kertai MD, et al. Statins are associated with a reduced incidence of perioperative mortality in patients undergoing major noncardiac vascular surgery. Circulation. 2003;107:1848–1851. doi: 10.1161/01.CIR.0000066286.15621.98. [DOI] [PubMed] [Google Scholar]
- 11.Pan W, Pintar T, Anton J, Lee VV, Vaughn WK, Collard CD. Statins are associated with a reduced incidence of perioperative mortality after coronary artery bypass graft surgery. Circulation. 2004;110:II45–II49. doi: 10.1161/01.CIR.0000138316.24048.08. [DOI] [PubMed] [Google Scholar]
- 12.Clark LL, Ikonomidis JS, Crawford FA, Jr, et al. Preoperative statin treatment is associated with reduced postoperative mortality and morbidity in patients undergoing cardiac surgery: an 8-year retrospective cohort study. J Thorac Cardiovasc Surg. 2006;131:679–685. doi: 10.1016/j.jtcvs.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 13.Collard CD, Body SC, Shernan SK, Wang S, Mangano DT. Preoperative statin therapy is associated with reduced cardiac mortality after coronary artery bypass graft surgery. J Thorac Cardiovasc Surg. 2006;132:392–400. doi: 10.1016/j.jtcvs.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 14.Youn YN, Kwak YL, Yoo KJ. Can the EuroSCORE predict the early and mid-term mortality after off-pump coronary artery bypass grafting? Ann Thorac Surg. 2007;83:2111–2117. doi: 10.1016/j.athoracsur.2007.02.060. [DOI] [PubMed] [Google Scholar]
- 15.Yang H, Youn YN, Yoo KJ. Correlation of akinesia with graft patency and cardiac enzyme after off-pump coronary artery bypass graft surgery. Circ J. 2010;74:1564–1569. doi: 10.1253/circj.cj-09-0857. [DOI] [PubMed] [Google Scholar]
- 16.Vander Salm TJ, Kip KE, Jones RH, et al. What constitutes optimal surgical revascularization? Answers from the Bypass Angioplasty Revascularization Investigation (BARI) J Am Coll Cardiol. 2002;39:565–572. doi: 10.1016/s0735-1097(01)01806-x. [DOI] [PubMed] [Google Scholar]
- 17.Sabik JF, Blackstone EH, Lytle BW, Houghtaling PL, Gillinov AM, Cosgrove DM. Equivalent midterm outcomes after off-pump and on-pump coronary surgery. J Thorac Cardiovasc Surg. 2004;127:142–148. doi: 10.1016/j.jtcvs.2003.08.046. [DOI] [PubMed] [Google Scholar]
- 18.Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007;50:2173–2195. doi: 10.1016/j.jacc.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Powell BD, Bybee KA, Valeti U, et al. Influence of preoperative lipid-lowering therapy on postoperative outcome in patients undergoing coronary artery bypass grafting. Am J Cardiol. 2007;99:785–789. doi: 10.1016/j.amjcard.2006.10.036. [DOI] [PubMed] [Google Scholar]
- 20.Song YB, On YK, Kim JH, et al. The effects of atorvastatin on the occurrence of postoperative atrial fibrillation after off-pump coronary artery bypass grafting surgery. Am Heart J. 2008;156:373.e9–373.e16. doi: 10.1016/j.ahj.2008.04.020. [DOI] [PubMed] [Google Scholar]
- 21.Winchester DE, Wen X, Xie L, Bavry AA. Evidence of pre-procedural statin therapy a meta-analysis of randomized trials. J Am Coll Cardiol. 2010;56:1099–1109. doi: 10.1016/j.jacc.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 22.Wassmann S, Faul A, Hennen B, Scheller B, Bohm M, Nickenig G. Rapid effect of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibition on coronary endothelial function. Circ Res. 2003;93:e98–e103. doi: 10.1161/01.RES.0000099503.13312.7B. [DOI] [PubMed] [Google Scholar]
- 23.Hinoi T, Matsuo S, Tadehara F, Tsujiyama S, Yamakido M. Acute effect of atorvastatin on coronary circulation measured by transthoracic Doppler echocardiography in patients without coronary artery disease by angiography. Am J Cardiol. 2005;96:89–91. doi: 10.1016/j.amjcard.2005.02.050. [DOI] [PubMed] [Google Scholar]
- 24.Ray KK, Cannon CP. Early time to benefit with intensive statin treatment: could it be the pleiotropic effects? Am J Cardiol. 2005;96:54F–60F. doi: 10.1016/j.amjcard.2005.06.027. [DOI] [PubMed] [Google Scholar]