Abstract
Background
Goniometers can be used to assess shoulder ROM with reasonable accuracy, but not internal rotation. Vertebral level, as determined by the hand-behind-the-back method, is used frequently but its reproducibility is questionable. We therefore devised a new measuring tape-based method for determining vertebral level.
Questions/purposes
We (1) compared the accuracy of a measuring tape-based and conventional vertebral-level method; (2) determined whether BMI affects their accuracy; and (3) devised a formula for converting distances measured using a measuring tape to vertebral levels.
Patients and Methods
We assessed internal rotation in 61 patients with shoulder pain. An electrode was taped to the skin where the thumb reached maximally behind the back. The vertebral-level method involved determining the vertebral level of the electrode by palpating bony landmarks whereas the measuring tape method involved measuring the distance between the C7 spinous process and the electrode. True vertebral levels of the electrode were confirmed by radiography.
Results
In nonobese patients, the accuracies of the upper thoracic and lumbar-level measurements were better for the measuring tape method than the vertebral-level method (r = 0.861 and 0.700, respectively in upper thoracic; 0.913 and 0.710, respectively in lumbar). Patient BMI affected the accuracy of the vertebral-level method but not that of the measuring tape method. The distances obtained using the measuring tape method could be converted into vertebral-level units using the formula: estimated vertebral level = 0.031 × [distance between C7 spinous process and thumb behind back] − 0.044 × [patient height] + 7.277.
Conclusions
The measuring tape-based method reflected shoulder internal rotation with higher accuracy than the vertebral-level method, and unlike the vertebral-level method, the measuring tape method was not affected by obesity.
Level of Evidence
Level II, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Careful physical examinations are an important aspect of patient assessment, and thus, all elements of physical examinations should be reliable and valid [6]. Conversely, the results of any examination are of limited value if they are not repeatable by the same or different clinicians [11]. The universal goniometer frequently is used to measure ROM and is reasonably reliable for determining shoulder flexion, extension, abduction, and external rotation [4, 13]. However, shoulder internal rotation is particularly difficult to measure using a goniometer because the abdomen prevents maximal internal rotation. The vertebral-level method frequently is used to reflect internal rotation, and is based on the location of the highest vertebral level reached by the thumb behind the back. However, this motion involves not only internal rotation of the shoulder but also extension of the shoulder and flexion of the elbow [8, 10]. Furthermore, although viewed as standard by some authors [7], the accuracy of the vertebral-level method has not been well established [1]. In addition, two studies raised questions regarding the reliability of the method, that is, one suggested that the interobserver reliability of the vertebral-level method is poor [5], whereas the other found the method is acceptable [7]. Therefore, a more objective method is needed to reflect internal rotation of the shoulder.
Edwards et al. [5] recommended recording internal rotation as “5 cm above the level of the iliac crest” as determined using a measuring tape. We propose a new method whereby the distance between the C7 spinous process and the maximal position reached by the thumb behind the back is measured using a measuring tape, which we refer to as the measuring tape method. The C7 spinous process is an easily palpated structure, regardless of patient weight or position [14], and therefore, it was used as a reference structure of the measuring tape method in the current study.
We sought (1) to determine the accuracies of the measuring tape-based method and the conventional vertebral-level method at different back levels; (2) to determine whether BMI affects these accuracies; and (3) to devise a formula for converting distances measured using the measuring tape to vertebral levels.
Patients and Methods
We recruited 72 patients from May 2010 to October 2010 who had shoulder pain. We excluded nine of the 72 patients with a spine, elbow, wrist, or hand disability as determined by medical history or physical examination; we also excluded two patients who were pregnant and unable to maintain a sitting position. This left 61 patients for the study. All patients were older than 18 years. Mean patient height was 164.3 cm (range, 146–182 cm), and mean weight was 62.4 kg (range, 48–89 kg). This study was approved by the ethical committee at Ajou University, and informed consent was obtained from all patients.
Patient age, height, and weight were recorded. Before taking measurements, all examiners were educated regarding the levels of certain bony landmarks including the C7 vertebral spinous process, the spine of the scapula at T3, the tip of the scapula at T7, and the top of the iliac crest at L4 [2]. Measurements were performed by one orthopaedic specialist (DHL), one orthopaedic resident (JJ), and one registered nurse specializing in orthopaedics (MHE). With the patient sitting, a radiopaque ECG electrode was taped on the skin where the examiner placed the hand of the patient with the thumb up at maximal height in the midline of the back. The electrode was used to evaluate the true vertebral level of the thumb by radiography. The location of the C7 spinous process was determined by assisted movement of the cervical spine into extension, in which the C6 spinous process moves anteriorly in normal healthy subjects, while C7 is the first cervical spinous process remaining stationary during this movement [9]. The vertebral level of the electrode was determined in one of two ways: palpating and counting the spinous processes down from C7 (the vertebral-level method) or measuring the distance between the C7 spinous process and the electrode with a measuring tape (the measuring tape method) (Fig. 1). Both methods were made independently by all three examiners and the examiners were unaware of the results of their colleagues. After clinical examination, each patient had one lateral radiograph of C7 to L5 with the patient seated. To assess the accuracy of the vertebral-level method, we bounded the region on the skin corresponding to the upper and lower levels of the seventh thoracic vertebral body with horizontal lines from the centers of the intervertebral disc above and below the vertebral body (Fig. 2A). This was performed using PACS software (PiView; Infinitt Co, Seoul, Korea) by a physician (SHH) unaware of the patients’ clinical information (Table 1). To determine the accuracy of the measuring tape method, we drew a line horizontally from the center of the tip of the C7 spinous process to the skin (Fig. 2B). Distances between the skin reference points of the C7 spinous process and the electrode also were measured using PACS software (Table 2). All radiographic distances were adjusted for magnification. To obtain radiographs with consistent magnification, the distance between the patient and the x-ray tube was set at 3 m.
Fig. 1.
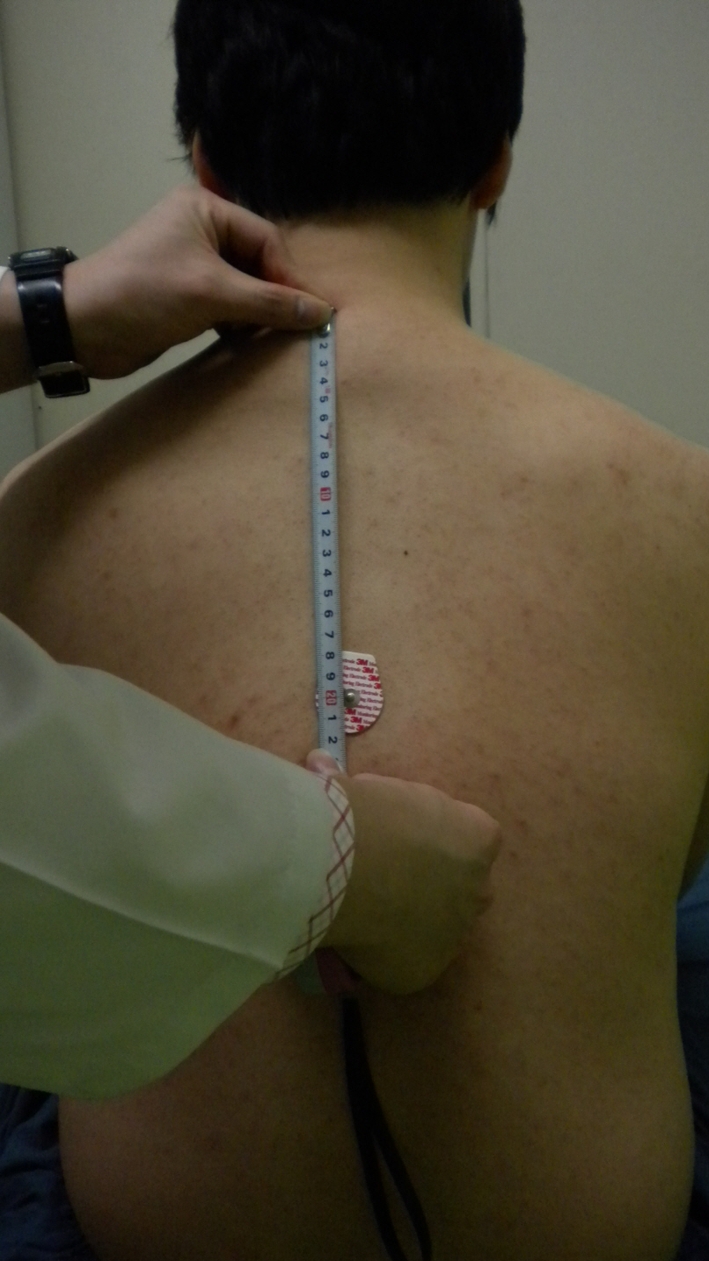
To confirm true vertebral level radiographically, a radiopaque electrode was taped onto the skin where a patient’s thumb reached maximally behind his or her back. The distance between the C7 spinous process and the electrode then was measured by an examiner for the distance method.
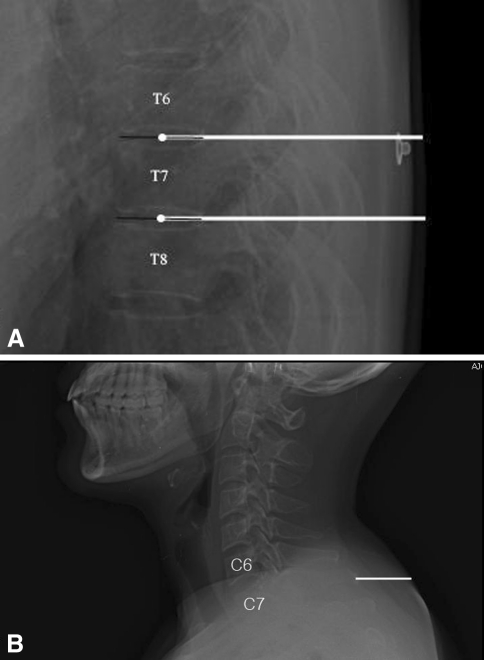
Fig. 2A–B.
(A) The skin at T7 was bounded with horizontal lines drawn from the midpoints of the intervertebral discs above and below the seventh thoracic vertebra. (B) The skin reference point on the back corresponding to the C7 spinous process was determined by drawing a horizontal line through the center of the C7 spinous process.
Table 1.
Categorical data of the vertebral level method measured by examiners
| Vertebral level of the thumb | Number of cases | ||
|---|---|---|---|
| Examiner 1 | Examiner 2 | Examiner 3 | |
| T3 | 0 (0%) | 0 (0%) | 0 (0%) |
| T4 | 3 (4.9%) | 3 (4.9%) | 2 (3.3%) |
| T5 | 3 (4.9%) | 2 (3.3%) | 2 (3.3%) |
| T6 | 9 (14.8%) | 3 (4.9%) | 17 (27.9%) |
| T7 | 12 (19.7%) | 18 (29.5%) | 6 (9.8%) |
| T8 | 6 (9.8%) | 6 (9.8%) | 6 (9.8%) |
| T9 | 2 (3.3%) | 5 (8.2%) | 3 (4.9%) |
| T10 | 1 (1.6%) | 5 (8.2%) | 2 (3.3%) |
| T11 | 2 (3.3%) | 0 (0%) | 2 (3.3%) |
| T12 | 6 (9.8%) | 3 (4.9%) | 5 (8.2%) |
| L1 | 4 (6.6%) | 4 (6.6%) | 5 (8.2%) |
| L2 | 2 (3.3%) | 3 (4.9%) | 1 (1.6%) |
| L3 | 2 (3.3%) | 1 (1.6%) | 0 (0%) |
| L4 | 5 (8.2%) | 5 (8.2%) | 5 (8.2%) |
| L5 | 4 (6.6%) | 3 (4.9%) | 5 (8.2%) |
| Total | 61 (100%) | 61 (100%) | 61 (100%) |
Table 2.
Continuous data of the distance method measured by examiners
| Distance between C7 spinous process and thumb | Length (mm) (n = 61) | ||
|---|---|---|---|
| Examiner 1 | Examiner 2 | Examiner 3 | |
| Mean (SD) | 280.4 (107.9) | 265.7 (107.7) | 279.9 (107.7) |
| 95% CI | 252.7–308.0 | 238.2–293.3 | 252.3–307.5 |
SD = standard deviation; CI = confidence interval.
We used Spearman’s rho to correlate the accuracies of the two methods. The effect of BMI on accuracy was evaluated by linear regression, and the formula used to convert distances measured using a tape to vertebral levels was determined by linear regression. SPSS® (Version 12.0.1; SPSS Inc, Chicago, IL, USA) was used for the statistical analysis.
Results
The accuracy of upper thoracic measurements in the overweight (BMI > 25.0 kg/m2) group was better (p = 0.008) for the measuring tape method (r = 0.872) than for the vertebral-level method (r = 0.516). Furthermore, the accuracies of upper thoracic-level measurements (p = 0.026) and lumbar-level measurements (p = 0.008) in the patients who were not overweight (BMI ≤ 25.0 kg/m2) also were better for the measuring tape method than for the vertebral-level method (Table 3).
Table 3.
Accuracies of the distance and vertebral-level methods
| Patient group | True level of the thumb | Spearman’s rho | p Value | |
|---|---|---|---|---|
| Distance method | Vertebral method | |||
| Overweight (BMI > 25.0) (n = 21) | Upper thoracic (T3–T7) | 0.872 | 0.516 | 0.008 |
| Lower thoracic (T8–T12) | 0.866 | 0.805 | 0.453 | |
| Lumbar (L1–L5) | 0.293* | 0.105* | ||
| Not overweight (BMI ≤ 25.0) (n = 40) | Upper thoracic (T3–T7) | 0.861 | 0.700 | 0.026 |
| Lower thoracic (T8–T12) | 0.924 | 0.839 | 0.168 | |
| Lumbar (L1–L5) | 0.913 | 0.710 | 0.008 | |
* Value showed no significant agreement with reference value; BMI = body mass index.
BMI affected the accuracy of the vertebral-level method (p = 0.029) but not that of the measuring tape method (p = 0.123).
The following formula was derived to convert distances measured using the measuring tape method to vertebral levels (Table 4): estimated vertebral level = 0.031 × [the distance between the C7 spinous process and position of the thumb (mm)] − 0.044 × [patient height (cm)] + 7.277. When results were rounded to the nearest whole numbers, 1 represented T3, 2 represented T4, and 3 represented T5. L5 was represented by 15. The strength of this formula to predict the true vertebral level was 96.2%.
Table 4.
Linear regression for predicting the true vertebral level by the formula*
| Parameter | Unstandardized | Standardized coefficients | t Value | p Value | |
|---|---|---|---|---|---|
| Beta (95% CI) | Standard error | Beta | |||
| Constant | 7.277 (4.547, 10.006) | 1.383 | 5.260 | 0.000 | |
| Distance between the C7 spinous process and the thumb | 0.031 (0.030, 0.032) | 0.001 | 0.955 | 46.881 | 0.001 |
| Height of patient | −0.044 (−0.060, −0.028) | 0.008 | −0.108 | −5.305 | 0.001 |
* Estimated vertebral level = 0.031 × [the distance between the spinous process of C7 and the thumb behind the back] − 0.044 × [patient height] + 7.277; R = 0.962; F = 1115.0; p < 0.001; CI = confidence interval.
Discussion
We propose a new method to reflect internal rotation of the shoulder based on the measurement of distance between the C7 spinous process and the maximal position reached by the thumb behind the back with a measuring tape. Although the vertebral-level method is the standard for measuring shoulder internal rotation, we believe this method is likely to be affected by obesity. The accuracies of these two methods were evaluated according to the level of the back. We also derived a formula to convert the measuring tape-determined distances to vertebral levels.
Certain study limitations should be noted. First, there were only three examiners, although the number of patients was substantially larger than in similar studies [5, 7], so that the statistical power of this study was adequate to show accuracy. Second, the measuring tape method cannot be used in patients with severe limitations of shoulder internal rotation in whom the hand will not reach the back or in patients with a back deformity, such as severe kyphosis.
Two studies have addressed the reliability of the vertebral-level method to determine internal rotation of the shoulder (Table 5). Green et al. [7] reported acceptable interobserver reliability (intraclass correlation coefficient [ICC] = 0.75) after examining six subjects, whereas Edwards et al. [5] considered the interobserver reliability as poor (ICC ≤ 0.27) after examining three subjects. However, these subject numbers were too small to take into account the effects of factors such as obesity [14]. We found the vertebral-level and the measuring tape methods had similar accuracies for lower thoracic measurements but the vertebral-level method was less accurate for upper thoracic and lumbar measurements. Furthermore, the accuracy of the vertebral method for upper thoracic measurements in overweight patients was only moderate. One might question whether there is a need to assess vertebral level more accurately (eg, with a measuring tape and/or a calculator) because most shoulder function scoring systems assign groups of two or three vertebral levels the same scores. One vertebral-level difference between L4 and L3 is worth two points in the Constant-Murley scoring system [3], which could be important in a clinically or legally specific situation. We would therefore argue more accuracy is needed.
Table 5.
Accuracies of the vertebral level of the hand behind the back method.
| Study | Population | Number of examiners | Accuracy |
|---|---|---|---|
| Green et al. [7] | Patient with shoulder pain (n = 6) | Six physiotherapists | Interobserver ICC = 0.75 |
| Edwards et al. [5] | Normal subjects (n = 3) | Eleven orthopaedic surgeons, and two physiotherapists | Interobserver ICC = 0.12, 0.27, 0.25 (each of three rounds) |
| Current study | Patients with shoulder pain (n = 61) | One orthopaedic surgeon, one orthopaedic resident, and one registered nurse (specializing in orthopaedics) | Spearman’s rho in upper thoracic (T3–T7) = 0.654, lower thoracic (T8–T12) = 0.799, lumbar (L1–L5) = 0.654 |
ICC = intraclass correlation coefficient.
Various bony landmarks such as the spine, the tip of the scapula, and the top of the iliac crest can be used to determine internal rotation of the shoulder. However, it is not easy to palpate the top of the iliac crest accurately in patients who are obese while they are sitting or standing [12, 15], and in these patients the vertebral-level method is less accurate than the method we propose.
Since some scoring systems devised for assessing shoulder function [3] require a measure of internal rotation based on vertebral level, clinicians use the vertebral-level method, as it allows them to compare their clinical results with those of others. Therefore, we devised a simple formula by linear regression that allows distance in the measuring tape method to be converted into vertebral-level units. For example, if the height of a patient is 167 cm and the distance between the C7 spinous process and the thumb position is 352 mm, the formula gives a result of 11, indicating L1. This should allow a more accurate reflection of internal rotation in the scores.
A new distance method using a measuring tape showed better accuracy for upper thoracic and lumbar measurements than the vertebral-level method. Furthermore, the method was unaffected by obesity, and a simple formula was derived to allow the measuring tape method to be used in clinical settings.
Acknowledgments
We thank Min-Hee Eun RN (specializing in orthopaedics) [MHE] for performing the physical examinations, Joo-Yun Lee for collecting data, Hyun-Yung Lee for helping with statistical analysis, and Do-Yung Park MD for editing our English.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This study was approved by the Ethical Committee of Ajou University (Approval No. AJIRB-MED-MDB-10-061).
References
- 1.Bovens AM, Baak MA, Vrencken JG, Wijnen JA, Verstappen FT. Variability and reliability of joint measurements. Am J Sports Med. 1990;18:58–63. doi: 10.1177/036354659001800110. [DOI] [PubMed] [Google Scholar]
- 2.Chakraverty R, Pynsent P, Isaacs K. Which spinal levels are identified by palpation of the iliac crests and the posterior superior iliac spines? J Anat. 2007;210:232–236. doi: 10.1111/j.1469-7580.2006.00686.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 4.Croft P, Pope D, Boswell R, Rigby A, Silman A. Observer variability in measuring elevation and external rotation of the shoulder. Primary Care Rheumatology Society Shoulder Study Group. Rheumatology (Oxford) 1994;33:942–946. doi: 10.1093/rheumatology/33.10.942. [DOI] [PubMed] [Google Scholar]
- 5.Edwards TB, Bostick RD, Greene CC, Baratta RV, Drez D. Interobserver and intraobserver reliability of the measurement of shoulder internal rotation by vertebral level. J Shoulder Elbow Surg. 2002;11:40–42. doi: 10.1067/mse.2002.119853. [DOI] [PubMed] [Google Scholar]
- 6.Fess EE. The need for reliability and validity in hand assessment instruments. J Hand Surg Am. 1986;11:621–623. doi: 10.1016/s0363-5023(86)80001-6. [DOI] [PubMed] [Google Scholar]
- 7.Green S, Buchbinder R, Forbes A, Bellamy N. A standardized protocol for measurement of range of movement of the shoulder using the Plurimeter-V inclinometer and assessment of its intrarater and interrater reliability. Arthritis Care Res. 1998;11:43–52. doi: 10.1002/art.1790110108. [DOI] [PubMed] [Google Scholar]
- 8.Kumar VP, Satku SK. Documenting rotation at the glenohumeral joint: a technical note. Acta Orthop Scand. 1994;65:483–484. doi: 10.3109/17453679408995498. [DOI] [PubMed] [Google Scholar]
- 9.Magee DJ. Orthopedic Physical Assessment. 4. Philadelphia, PA: WB Saunders; 2002. [Google Scholar]
- 10.Mallon WJ, Herring CL, Sallay PI, Moorman CT, Crim JR. Use of vertebral levels to measure presumed internal rotation at the shoulder: a radiographic analysis. J Shoulder Elbow Surg. 1996;5:299–306. doi: 10.1016/S1058-2746(96)80057-7. [DOI] [PubMed] [Google Scholar]
- 11.Marx RG, Bombardier C, Wright JG. What do we know about the reliability and validity of physical examination tests used to examine the upper extremity? J Hand Surg Am. 1999;24:185–193. doi: 10.1053/jhsu.1999.jhsu24a0185. [DOI] [PubMed] [Google Scholar]
- 12.McKenzie AM, Taylor NF. Can physiotherapists locate lumbar spinal levels by palpation? Physiotherapy. 1997;83:235–239. doi: 10.1016/S0031-9406(05)66213-X. [DOI] [Google Scholar]
- 13.Riddle DL, Rothstein JM, Lamb RL. Goniometric reliability in a clinical setting: shoulder measurements. Phys Ther. 1987;67:668–673. doi: 10.1093/ptj/67.5.668. [DOI] [PubMed] [Google Scholar]
- 14.Robinson R, Robinson HS, Bjørke G, Kvale A. Reliability and validity of a palpation technique for identifying the spinous processes of C7 and L5. Man Ther. 2009;14:409–414. doi: 10.1016/j.math.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Snider KT, Kribs JW, Snider EJ, Degenhardt BF, Bukowski A, Johnson JC. Reliability of Tuffier’s line as an anatomic landmark. Spine (Phila Pa 1976) 2008;33:E161–E165. doi: 10.1097/BRS.0b013e318166f58c. [DOI] [PubMed] [Google Scholar]