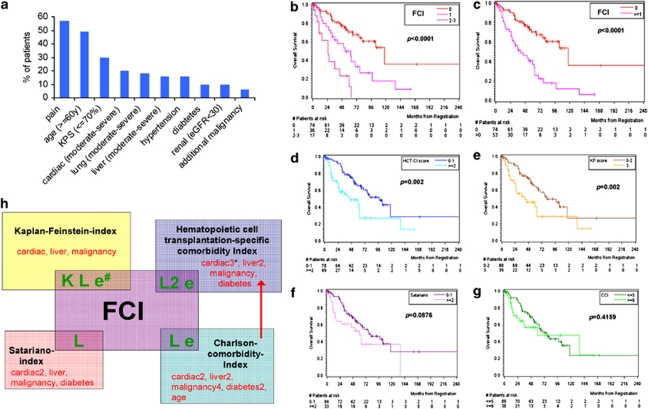
Figure 1.
Analysis of comorbidities, and survival with different comorbidity scores in MM patients. (a) Distribution of specific comorbidities and patient characteristic features. Pain (57%) and a diminished KPS (30%) were most frequently impaired attributes in our MM cohort. Common organ comorbidities were cardiac (20%), lung (18%) and moderate-to-severe liver disease (16%), hypertension (16%), diabetes (10%) and renal impairment (10%). Additional malignancies occurred in 6%. Age ⩾60 years was present in 49% of the patients. All of our assessed comorbidity conditions are also captured in the KF, HCT-CI, CCI and SI, accept for pain (see also Supplementary Table 1). (b) On the basis of our univariate and multivariate results, a prognostic model was constructed, combining the KPS (⩽70%), lung impairment and eGFR (<30 ml/min/1.73 m2) in a comorbidity sum score (FCI). This allowed to define largely different patient groups: OS was significantly different among patients with no (−), 1(−), 2 or 3 (−) risk factors, with median survival times of 118 (n=74), 53 (n=36) and 25 months (n=17), respectively, (P=0.0033 and P<0.0001). (c) FCI stratification into two patient risk groups: OS was again significantly different in patients with no (−) vs 1–3 (−) risk factors, with median OS of 117 (n=74) vs 41 months (n=53, P<0.0001), respectively. (d–g) OS differences of low-risk vs high-risk patients as stratified via HCT-CI (d), KF (e), SI (f) and CCI (g). The differences among risk groups as scored via HCT and KF were significant (P<0.05), whereas via SI and CCI less distinctive. (h) The established four CIs (KF, HCT-CI, SI and CCI) are compared with the FCI. The number of weighted factors is given behind each comorbidity factor. The number of evaluated comorbidities in our univariate and multivariate analyses that led to the FCI covered 8/12, 10/17, 10/20 and 7/7 comorbidities as included in the established KF, HCT-CI, CCI and SI, respectively. The figure depicts why the FCI, KF and HCT-CI were more valuable in MM than in SI: the KF includes the appraisal of a reduced KPS (K), lung disease (L) and renal impairment (e) that were all highly valuable in our MM cohort; both the HCT-CI and CCI also include lung disease and renal impairment in their score, whereas the SI includes only lung impairment in its comorbidity assessment.