Abstract
Objective
The purpose of this article is to review the literature that discusses normal anatomy and biomechanics of the foot and ankle, mechanisms that may result in a lateral ankle sprain or syndesmotic sprain, and assessment and diagnostic procedures, and to present a treatment algorithm based on normal ligament healing principles.
Methods
Literature was searched for years 2000 to 2010 in PubMed and CINAHL. Key search terms were ankle sprain$, ankle injury and ankle injuries, inversion injury, proprioception, rehabilitation, physical therapy, anterior talofibular ligament, syndesmosis, syndesmotic injury, and ligament healing.
Discussion
Most ankle sprains respond favorably to nonsurgical treatment, such as those offered by physical therapists, doctors of chiropractic, and rehabilitation specialists. A comprehensive history and examination aid in diagnosing the severity and type of ankle sprain. Based on the diagnosis and an understanding of ligament healing properties, a progressive treatment regimen can be developed. During the acute inflammatory phase, the goal of care is to reduce inflammation and pain and to protect the ligament from further injury. During the reparative and remodeling phase, the goal is to progress the rehabilitation appropriately to facilitate healing and restore the mechanical strength and proprioception. Radiographic imaging techniques may need to be used to rule out fractures, complete ligament tears, or instability of the ankle mortise. A period of immobilization and ambulating with crutches in a nonweightbearing gait may be necessary to allow for proper ligament healing before commencing a more active treatment approach. Surgery should be considered in the case of grade 3 syndesmotic sprain injuries or those ankle sprains that are recalcitrant to conservative care.
Conclusion
An accurate diagnosis and prompt treatment can minimize an athlete's time lost from sport and prevent future reinjury. Most ankle sprains can be successfully managed using a nonsurgical approach.
Key indexing terms: Ankle joint, Ankle injuries, Chiropractic, Physical therapy
Introduction
Ankle sprains are the most frequent injuries sustained by athletes.1-6 Literature reveals that ankle sprains may account for approximately 20% to 40% of all athletic injuries.7-9 Eighty-five percent of ankle sprains are caused by excessive inversion.10,11 When the ankle rolls inward at a high velocity, it may lead to stretching or tearing of the lateral ligament complex.5,11-13 Ankle sprains are common among athletes who participate in sports that involve running on changing terrains, repetitive jumping, or frequent changes in direction, such as basketball, volleyball, soccer, football, and cross-country.14–16 In basketball, the ankle may roll inward when a player awkwardly lands on an opponent's foot (Fig 1). The injured basketball player may have heard a popping noise. Symptoms may include pain, swelling, and joint stiffness. Depending on the severity of the injury, the athlete may be able to ambulate cautiously with little or no pain, or may be unable or only partially able to bear weight on the injured ankle.2,17-19
Fig 1.
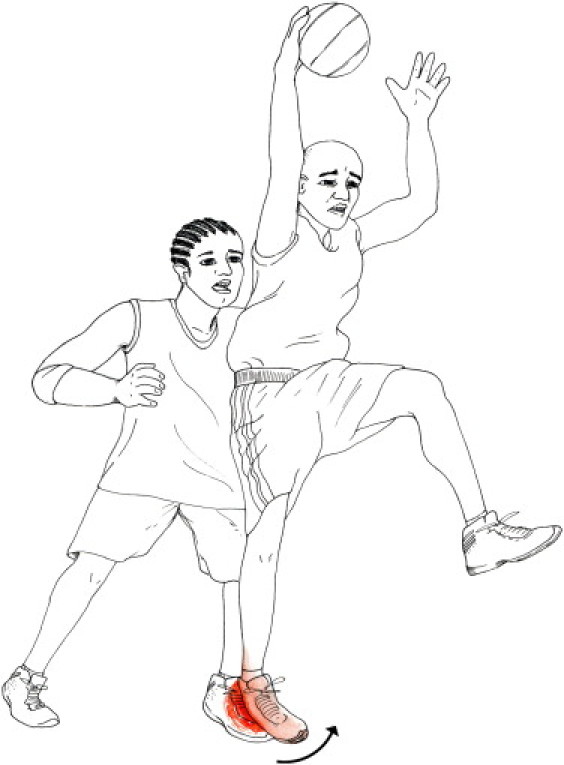
Basketball player sustaining a lateral ankle sprain.
Most ankle sprains can be treated successfully with an aggressive nonsurgical care program that is tailored to the individual athlete.10,18,20-26 The treating physician should have an understanding of the following: the anatomy and biomechanics of the foot and ankle, diagnostic skills to differentiate the type and grade of ankle sprain, knowledge of the different phases and approximate time frames of ligament healing, and the ability to recognize and rule out red flags that may necessitate a period of complete immobilization or surgery. Progression through treatment should be based on the science of ligament healing, the patient's symptoms, and the physician's clinical assessment.27 The purpose of this review is to simplify current research from various health care disciplines to develop a streamlined treatment of lateral and syndesmotic ankle sprains.
Methods
A search of electronic databases was performed to find articles published within the last 10 years. Articles were reviewed based on the title and abstract. Databases used include PubMed and CINAHL. Also used was Google Scholar; The American Journal of Sports Medicine database; and the American Physical Therapy Association's online, Open Door, database. Key search terms were ankle sprain$, ankle injury and ankle injuries, inversion injury, proprioception, rehabilitation, physical therapy, anterior talofibular ligament, syndesmosis, syndesmotic injury, and ligament healing. Text books were also used to review anatomy. Articles were also retrieved based on being references in articles that were found through our initial search process. Only English-language articles were reviewed. Research was not limited to human studies. The intent was to perform a thorough review of high-quality, recent literature on lateral and syndesmotic ankle injuries. The decision to include articles for this review was made by the lead author with a focus on the strength of the article's original research and comprehensiveness. In excess of 200 abstracts were originally reviewed; and ultimately, 74 full-text articles met the inclusion criteria, and a total of 84 references were included for this narrative review.
Discussion
Anatomy and biomechanics of the foot and ankle
The ankle joint connects the lower leg to the foot and consists of 2 separate joints: the talocrural joint (TCJ) (ankle mortise) and the subtalar joint (STJ). The TCJ consists of the articulation of the distal aspect of the tibia and fibula with the talus (Fig 2).26 The distal aspect of the fibula is contained within a vertically oriented groove, the fibula notch, located on the lateral aspect of the tibia and situated between the anterior and posterior tibia tubercles.28 The distal aspect of the tibia and fibula forms a protective housing that surrounds and articulates with the superior aspect of the body of the talus, the trochlea. The medial border of the housing consists of the medial malleolus, the distal portion of the tibia; the superior border consists of the pilon, a horizontal expansion of the tibia; and the lateral border consists of the lateral malleolus, the distal portion of the fibula.19 During gait, range of motion of the TCJ consists of ground reactive dorsiflexion when the tibia moves forward over the foot; and plantar flexion, when the heel lifts off of the ground as the foot prepares for toe-off (Fig 3). Although variability exists, normal range of motion of the TCJ is 50° of plantar flexion and 20° of dorsiflexion.2,29,30
Fig 2.
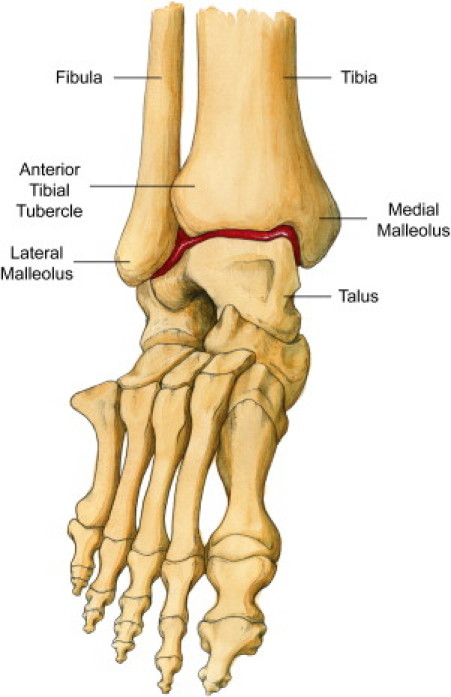
Talocrural joint (indicated by red demarcation). ⁎⁎Also labeled are the fibula, tibia, anterior tibial tubercle, medial malleolus, lateral malleolus, and talus.
Fig 3.
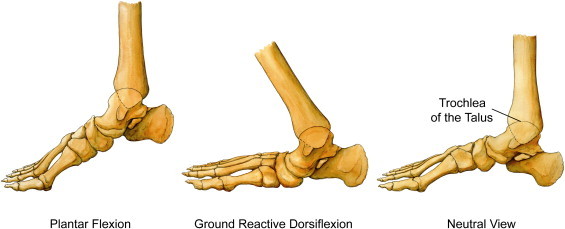
Range of motion of the TCJ. Each picture is labeled: left to right—plantar flexion, ground reactive dorsiflexion, neutral view. The neutral view labels the trochlea of the talus.
The STJ consists of the articulation between the undersurface of the talus and the calcaneus (heel bone) (Fig 4). Motion of the STJ consists of eversion (the heel pivots outward) and abduction (the foot turns away from the midline), or inversion (the heel pivots inward) and adduction (the foot turns toward the midline) (Fig 5). Although variation exists, average range of motion of the STJ is 25° to 30° of inversion and 5° to 10° of eversion. These ranges of motion are rarely exceeded during a normal walking or running gait.30,31 Normally, “during the stance phase of gait on even ground the heel strikes with minimal inversion at the STJ followed by eversion ranging from 5-10° at 10% of the walking cycle. From there, inversion occurs at the STJ reaching a maximum of 5° at 62% of the walking cycle.”31
Fig 4.
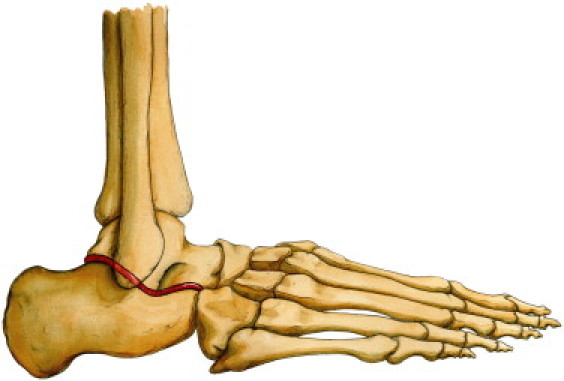
Subtalar joint (indicated by red demarcation).
Fig 5.
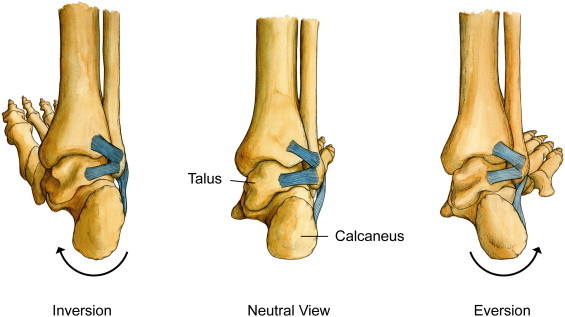
Range of motion of the STJ (right foot). Each picture is labeled: left to right—inversion, neutral view (also identifies the talus and calcaneus), and eversion.
The talus is the centerpiece of the lower extremity that connects the lower leg to the foot through its articulations with the TCJ and STJ. Shortly after the foot strikes the ground, the foot and ankle go through a series of motions that have been termed pronation.32,33 Pronation of the foot and ankle consists of the following movement patterns: dorsiflexion of the TCJ, positioning the wider anterior aspect of the trochlea within the ankle mortise; eversion of the calcaneus at the STJ; and the distal aspect of the talus, the talar head, dropping downward and inward. These adaptations maximize the surface contact area of the talus within the ankle mortise and the underlying calcaneus, temporarily transforming the ankle joint into a solid mass that connects the foot to the leg. Other motions occur during pronation that allow for increased mobility at the knee and midfoot articulations. The tibia rotates internally, allowing the knee joint to flex; and the navicular bone, a tarsal bone anterior to the talus, advances forward, thereby unlocking the midfoot articulations.30-33 Under normal circumstances, pronation of the foot and ankle permits the lower extremity to effectively absorb vertical and rotational forces associated with running, cutting, or landing from a jump without incurring injury.
Ligaments are soft tissue structures that connect one bone to another bone. The ligaments surrounding the ankle joint aid in providing passive support to the STJ and/or TCJ as these joints approach or exceed the end ranges of motion.2 Ligaments are mainly constituted of dense parallel bundles of collagen fibers that are arranged in an undulating pattern (crimp). The crimp of the ligament has been equated to the action of a spring. When the ligament is placed under tension, the crimp of the ligament straightens; and collagen fibers are recruited to dissipate internal forces and resist excessive motion. If these forces do not exceed the mechanical strength of the ligament, pathological motion of the ankle is prevented; and the crimp of the ligament recoils. However, if the load surpasses the mechanical strength of the ligament and is applied at a fast velocity that exceeds the speed of a corrective muscle reflex, it may lead to microscopic failure of the collagen fibers or a complete rupture of the ligament.19,34
The ligaments that surround the ankle joint consist of the lateral collateral ligaments, syndesmotic ligaments, and the medial collateral ligaments (MCLs). The lateral collateral ligaments consist of the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and the posterior talofibular ligament1,26,35,36 (Fig 6A, B). The ATFL and CFL originate from the lateral malleolus; the former inserts onto the neck of the talus and the latter onto the calcaneus. The ATFL resists pathological inversion and plantar flexion of the ankle joint. The CFL resists excessive inversion of the ankle joint and is further stressed at the end ranges of dorsiflexion.37
Fig 6.
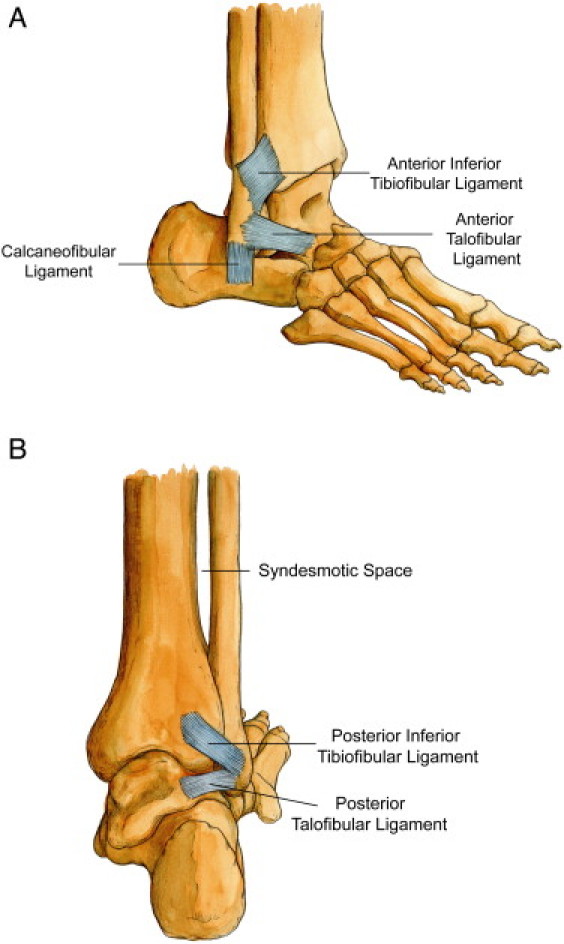
A, Lateral oblique view of the ankle joint. Identifies CFL, AITFL, and ATFL. B, Posterior view of the ankle joint. Identifies syndesmotic space, PITFL, and posterior talofibular ligament.
The syndesmotic ligaments consist of the anterior inferior tibiofibular ligament (AITFL), interosseous ligament, posterior inferior tibiofibular ligament (PITFL), and the transverse ligament. The AITFL originates from the lateral malleolus of the fibula; travels medially, obliquely, and proximally; and inserts onto the anterior lateral tibia tubercle (Fig 6A). The interosseous ligament lies underneath the AITFL, originates from the anterior inferior aspect of the lateral malleolus, and inserts onto the anterior inferior aspect of the tibia. The PITFL originates on the lateral malleolus and inserts onto the posterior lateral tibia process (Fig 6B), and the transverse ligament lies deep to the PITFL.2,19,26,28,38 The function of the syndesmotic ligaments is to hold the fibula tight to the tibia, thereby preventing abnormal widening of the ankle mortise. During ground reactive dorsiflexion, the posterior aspect of the talus rotates 5° externally within the ankle mortise, the fibula rotates 3° to 5° externally, and the ankle mortise widens 1 to 2 mm.39 Ogilvie-Harris et al conducted a study on cadaveric ankle models to evaluate the contribution of each syndesmotic ligament in maintaining an intact ankle mortise. The results indicated the following: AITFL, 35%; PITFL, 33%; interosseous ligament, 22%; and the transverse ligament, 9%.40
The MCLs consist of 3 superficial ligaments—the tibionavicular, tibiocalcaneal, and tibiotalar ligaments—and 2 deep ligaments—the anterior and posterior tibiotalar ligaments. These ligaments resist excessive eversion and external rotation of the ankle joint.19,26,37
Dynamic support structures of the ankle joint
“Preservation of joint stability is dependent on synergistic function of bones, joint capsules, ligaments, muscles, tendons and sensory receptors and their spinal and cortical neural projections and connections in the brain.”34 The dynamic support structures of the ankle consist of the muscles of the leg, associated tendons, and the proprioceptive fibers contained within the surrounding soft tissue structures. Proprioceptive fibers supply sensory afferent input in regards to joint position and stimulate muscle reflexes to position the foot and ankle for proper joint function.19,34,41
Tendons are nonelastic structures that attach muscles to bone and transfer forces generated by the attaching muscle across a joint. Muscles generate force through 3 types of contractions: concentric, eccentric, and isometric. A concentric contraction involves shortening of muscle fibers to generate a particular motion. An eccentric contraction is a controlled lengthening of muscle fibers to decelerate a particular motion. And an isometric contraction involves neither elongation nor shortening of muscles and is useful in the initial stages of a rehabilitation program.42
The peroneus longus and peroneus brevis muscles are located on the outside of the leg, and their tendons pass behind the lateral malleolus. The peroneus longus tendon travels diagonally underneath the foot, inserting onto the plantar surface of the medial cuneiform bone and the base of the first metatarsal, whereas the peroneus brevis tendon inserts onto the dorsal surface of the tuberosity of the fifth metatarsal bone (Fig 7). The tibialis anterior muscle is located on the front of the shin and attaches to the medial and inferior aspect of the medial cuneiform and the base of the first metatarsal bone (Fig 8).43 A concentric contraction of the peroneii musculature promotes ankle eversion. An eccentric contraction of the tibialis anterior musculature and the adjacent extensor musculature of the anterior leg decelerates plantar flexion.
Fig 7.
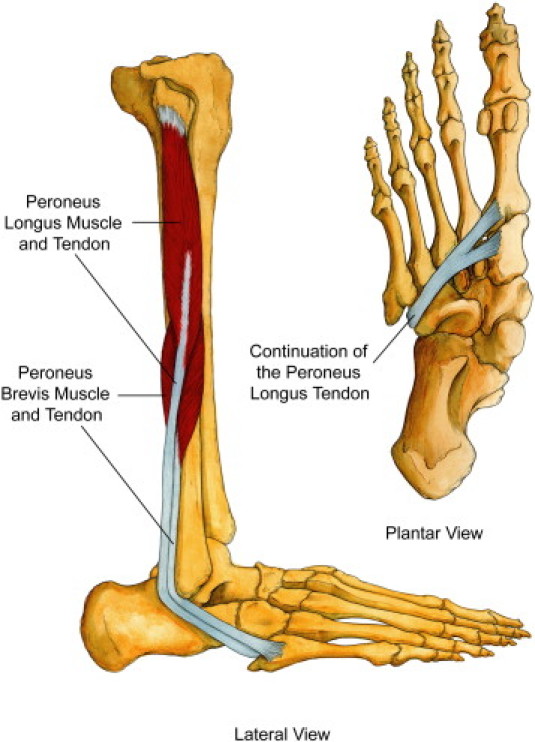
Peroneus longus and brevis muscles and tendons. Identifies lateral-view peroneus longus muscle and tendon, peroneus brevis muscle and tendon, and plantar-view continuation of the peroneus longus tendon.
Fig 8.
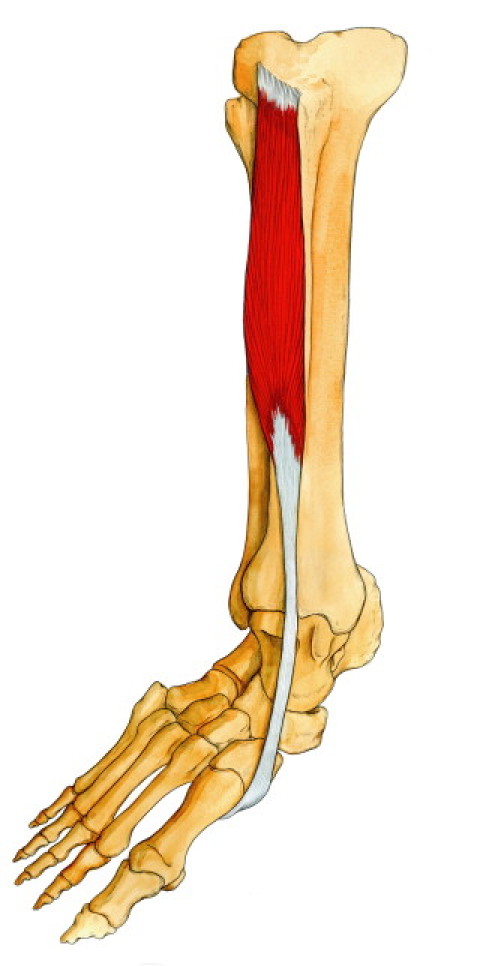
Tibialis anterior muscle.
A normal stride depends on an accurate sense of joint position.44 As the nonweightbearing leg prepares for initial ground contact (terminal swing), the lateral edge of the foot passes only 5 mm above the ground.45 The optimal position of the foot and ankle during terminal swing would be in a slightly dorsiflexed and minimally inverted position. A lateral ankle sprain may occur if the lateral edge of the foot strikes the ground in an excessively inverted position. Results of previous studies have suggested that a proprioceptive muscle reflex response of the peroneal muscles would not be fast enough to prevent a sudden forceful inversion sprain mechanism. However, proprioceptive input can stimulate peroneal and tibialis anterior muscle reflexes, correcting faulty foot biomechanics before initial ground contact.46
Faulty movement patterns, trauma, or awkward landings may predispose to an ankle injury. Depending on the mechanism, an appropriate diagnosis of ligamentous injury can usually be ascertained.19
Mechanisms of ankle sprains
Injury to the lateral collateral ligaments usually occurs when the athlete's center of gravity is shifted over the lateral border of the weightbearing leg, causing the ankle to roll inward at a high velocity.47 The ATFL is the weakest of the lateral collateral ligaments and therefore the first to be injured.2 Injury to the CFL may also occur in more severe sprains.48 Mechanisms of injury may include landing awkwardly on an opponent's foot, catching the outer aspect of the foot on the ground terrain, or a slide tackle that contacts the inside of the opponent's weightbearing leg11 (Fig 9). A study using cadaver foot and ankle models revealed tearing of the lateral collateral ligaments when the talus inverts approximately 30° to 45° within the ankle mortise.19 Other structures that may be injured during a lateral ankle sprain may include the peroneal tendons, lateral joint capsule, and the proprioceptive nerve endings found within these soft tissue structures.35,44 Literature indicates that injury to joint mechanoreceptors may occur during an ankle sprain, resulting in proprioceptive deficits and poor ankle/foot biomechanics.49 Reduced mechanical strength of the ligaments and proprioceptive deficits lead to joint laxity and impaired dynamic support of the surrounding musculature.19,50
Fig 9.
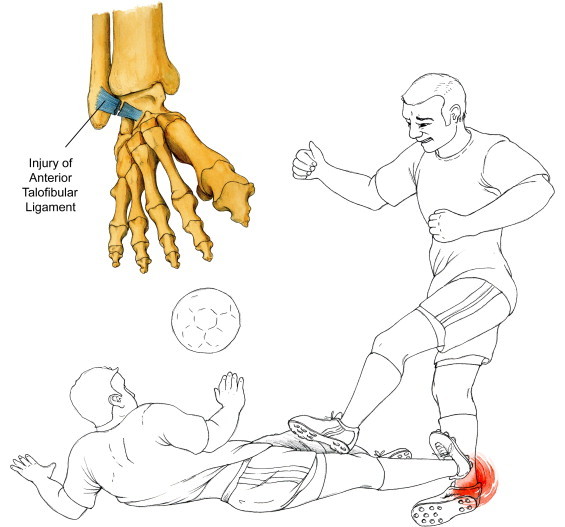
Mechanism of a lateral ankle sprain. Identifies injury of ATFL.
Syndesmotic “high ankle” sprains constitute approximately 10% of all ankle sprains.19,26 These sprains are more prevalent in high-energy contact sports or in sports that involve wearing a stiff boot or skate, such as hockey or skiing.38 Examples of injury may include a skier that catches the inside edge of the uphill ski while attempting to avoid a gate or a football player that pivots suddenly to the inside with the outside foot fixed on the playing surface (Fig 10). Both of these mechanisms of injury may result in an excessive external rotation force on the fibula with respect to the tibia that may lead to disruption of the syndesmotic ligaments, in particular the AITFL.26,51 Severity of injury usually depends on the magnitude of the force and how long it was applied to the ankle mortise. The rehabilitation period for syndesmotic injuries tends to be longer than lateral ankle injuries. A recent study indicated that a syndesmotic sprain may require a treatment period almost twice as long as a grade 3 lateral ankle sprain.39,52
Fig 10.
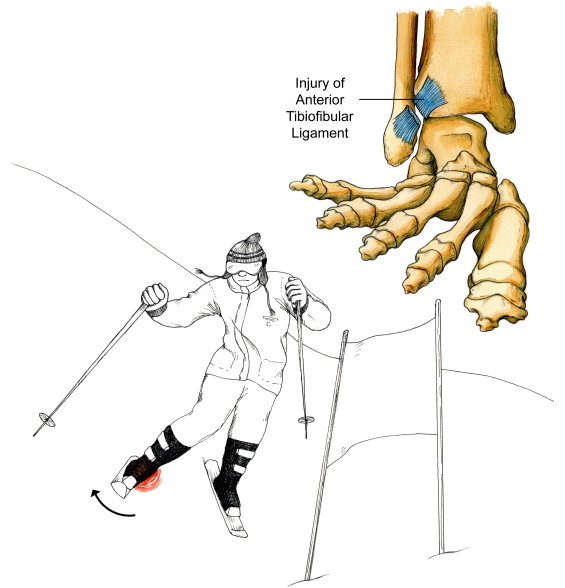
Mechanism of a syndesmotic sprain. Identifies injury of anterior tibiofibular ligament.
Diagnosis
The examining doctor can usually determine the type and severity of ankle sprain based on the history and physical examination. The history should include the following:
-
•
date of injury;
-
•
mechanism of injury;
-
•
presence of a popping sound at time of injury;
-
•
ability to bear weight through the injured leg;
-
•
history of ankle injury, including treatment received;
-
•
sport-specific goals.
It is important to ascertain sport-specific goals that may necessitate prompt diagnosis and more aggressive treatment procedures.2 A detailed physical examination should follow the history.
The physical examination should begin with observation for gross abnormalities, edema, ecchymosis, neurovascular assessment, and palpation for areas of tenderness. Check the dorsal pedal pulse, capillary refill, and sensation to light touch. Edema may be quantified using a tape measure to make a figure-8 measurement that encompasses the medial malleolus, lateral malleolus, navicular, and base of the fifth metatarsal.29 Palpate for regions of tenderness over the lateral collateral ligaments, syndesmotic ligaments, deltoid ligaments, the osseous landmarks used in the figure-8 measurement, and the soft tissue structures of the leg.
The following Ottawa guidelines should be used to determine if radiographs are necessary: palpation that reveals tenderness over the medial malleolus, lateral malleolus, navicular, and/or base of the fifth metatarsal; an inability to bear weight immediately following injury or during the clinical evaluation; or tenderness that extends 6 cm superiorly from the tip of either malleolus, not over the ATFL.1,26,38 Radiographs should be performed immediately if gross abnormalities are visualized. Standard radiographic views include anterior to posterior, lateral, and ankle mortise. Even if radiographs are inconclusive, a Salter-Harris type 1 fracture should be considered in a skeletally immature patient if palpation elicits tenderness over the distal tibia or fibula growth-plates.2,53
Goniometer measurements should be taken of active and passive ranges of motion of the injured and noninjured ankles. Active range of motion measurements assess the musculotendinous integrity of the gastrocnemius/soleus complex, peroneus longus and brevis, tibialis anterior and extensor digitorum longus, and tibialis posterior by having the patient plantarflex, evert, dorsiflex, and invert the ankle, respectively. Passive range of motion measurements of the injured ankle assesses joint integrity and is compared with clinical norms and measurements of the noninjured ankle.
The following orthopedic tests may prove useful in aiding diagnosis1,2,19,23,38,52,54-56:
-
•
Anterior drawer test: Stabilizing the tibia and fibula, the foot is held in 20° of plantar flexion while the talus is drawn forward in the ankle mortise. This tests the integrity of the ATFL and anterior joint capsule. A positive test result would be greater than 5 mm of anterior motion of the STJ as compared with the noninjured ankle, and an audible clunk may be elicited. If the ankle is inverted while conducting the anterior drawer test, it also evaluates the integrity of the CFL.
-
•
Talar tilt test: The ankle is held in anatomical position, and the talus is tilted into adduction and abduction. This primarily tests the integrity of the CFL when the foot is in a neutral position; when the test is performed with plantar flexion, it also evaluates the integrity of the ATFL. A positive test result would be 5° to 10° of increased inversion as compared with the noninjured ankle and would be indicative of a tear of the CFL.
-
•
External rotation test: Manual passive external rotation of the foot and ankle in a neutral or slightly dorsiflexed position would widen the ankle mortise. Pain over the distal syndesmosis is positive for a syndesmotic injury.
-
•
Tibia/fibula squeeze test: Result is positive for a syndesmotic sprain if compression of the tibia and fibula in the midcalf region produces pain over the distal syndesmosis.
-
•
Stabilization test: Tape is applied around the distal syndesmotic region for support. A positive test result for syndesmotic injury would be reduced pain over the distal syndesmosis during ambulation or when performing a heel raise.
These orthopedic tests should be conducted bilaterally. During the initial stages of injury, the findings of these examination tools may be limited because of pain, swelling, and spasm. The anterior drawer and the talar tilt test are found to have a markedly increased sensitivity when performed 4 to 5 days after injury.26
Examination findings of a lateral ankle sprain may include the following:
-
•
Swelling observed distal to the lateral malleolus of the ankle that may extend to the foot if the lateral capsule is torn.
-
•
Tenderness palpated over the ATFL and, in more severe cases, the CFL.
-
•
The anterior drawer and the talar tilt test may reveal joint laxity due to tearing of the ATFL and/or the CFL ligament.
-
•
Stress radiographs may reveal excessive anterior translation of the talus or inversion of the talus.
Lateral ankle sprains are based on a grade 1 to 3 classification. A grade 1 ankle sprain usually entails microscopic tearing of the ATFL. Symptoms may include minimal swelling and point tenderness directly over the ATFL; however, there is no instability, and the athlete can ambulate with little or no pain. A grade 2 ankle sprain involves microscopic tearing of a larger cross-sectional portion of the ATFL. Symptoms may include a broader region of point tenderness over the lateral aspect of the ankle, a painful limp if able to ambulate, and bruising and localized swelling due to tearing of the anterior joint capsule, ATFL, and surrounding soft tissue structures. A grade 3 ankle sprain entails a complete rupture of the ATFL and may also involve microscopic or complete failure of the CFL. The posterior talofibular ligament is rarely injured during inversion ankle sprains. Symptoms may include diffuse swelling that obliterates the margins of the Achilles tendon, inability to ambulate, and tenderness on the lateral and medial aspects of the ankle joint.2,22,26
Examination findings of a syndesmotic sprain may include the following:
-
•
Edema observed proximally to the ankle mortise.
-
•
Tenderness palpated over the AITFL that may extend up the leg. The length of tenderness measured from the distal tip of the fibula proximally up the interosseous space has been called the tenderness length. The tenderness length has been reported to correlate with the severity of a syndesmotic sprain.56
-
•
The external rotation test, squeeze test, and stabilization test result may be positive.
-
•
Standard or stress radiographs may reveal abnormal widening of the ankle mortise.
Syndesmotic sprains have been separated into 3 categories: (1) sprain without diastasis (pathological separation) of the ankle mortise; (2) latent diastasis or diastasis that is only apparent after stress radiographs; and (3) frank diastasis that is usually accompanied by a fracture.26,28
Dynamic ultrasound examination may prove useful in the early diagnosis and grading of syndesmotic sprains. In a preliminary study conducted by Mei-Dan et al,39 dynamic ultrasound examination was accurate in visualizing a tear of the AITFL and abnormal widening of the ankle mortise.
If symptoms persist after 6 weeks of therapy, a computed axial tomography scan or a magnetic resonance imaging test (MRI) may be considered.10,51 These advanced imaging tools may aid in ruling out osteochondral lesions and tumors or in reevaluating the grade of injury.57-60
Stages of ligament healing
Chronology of ligament healing has been separated into 3 distinct phases: inflammatory, reparative, and remodeling. The following healing chronology is based on a completely ruptured ligament.
The initial response to injury would be the acute inflammatory phase, lasting 24 to 72 hours. Damage to the blood vessels within the ruptured ligament and surrounding tissues results in a hematoma that fills the gap between the 2 retracted ligament ends. The capillaries surrounding the injured ligament increase in permeability, resulting in swelling and the migration of plasma proteins and leukocytes (white blood cells). The white blood cells engulf and eliminate the damaged cells and dead debris, a process termed phagocytosis. Chemical mediators are released during phagocytosis that promote new blood vessel formation, neovascularization. Oxygen and nutrients are now available for the process of tissue repair.18,19,34,61
The reparative phase of healing begins 3 to 5 days postinjury. Dead or damaged tissue is repaired or replaced with healthy cells and connective tissue. At approximately 5 days postinjury, the gap between the 2 retracted ligament ends is filled with granulation connective tissue, consisting of macrophages, new blood vessels, and fibroblasts. The fibroblasts produce proteoglycan and collagen, the subunits necessary for ligament repair. Collagen production intensifies; and by 10 to 14 days, disorganized collagen now connects the 2 ligament ends. The ligament may now be able to resist low-level tensile forces.
The remodeling phase of healing begins 15 to 28 days postinjury. The newly formed collagen fibers align themselves longitudinally, and cross-linkages form. By 3 weeks, as collagen maturation continues, the ligament may regain approximately 60% of its tensile strength. By 3 months, the ligament may regain its preinjury strength.
The ligament healing process can be expedited by immediately instituting an aggressive nonsurgical treatment protocol that initially minimizes pain, inflammation, and swelling and incorporates early controlled motion. The treatment approach should be individualized and under the careful observation of the treatment staff. Studies indicate that early progressive rehabilitation has a favorable outcome in restoration of ligament tensile strength, encourages lymphatic drainage, restores proprioception, decreases muscle atrophy, and minimizes excessive arthrofibrosis or scarring.19,56
Treatment of grade 1 and 2 ankle sprains—for which types/severity of injuries?
The goals of therapy are to accentuate the normal healing process and protect the ligament from further injury. The acronym PRICESMMS stands for proprioception training, rest/modified activity, ice, compression, elevation, stabilization, medications (nonsteroidal anti-inflammatory drugs), mobilization, and strength training.20 These rehabilitation techniques should be applied appropriately during each phase of treatment. Progression of the treatment plan depends on the severity of injury, the patient's response to therapy, and the achievement of goals during each treatment phase.26,40
Acute inflammatory phase (24-72 hours)
The initial goals of therapy are to limit inflammation, reduce pain, and protect from further injury.2,25,26
-
•
Ice therapy should be applied for 20 minutes on/1 hour off throughout the day, with a compression bandage and the leg elevated above the heart. Cryotherapy reduces pain, edema, and secondary hypoxic damage to injured tissues.2,55,62,63
-
•
Nonsteroidal anti-inflammatory drugs, electric muscle stimulation, pulsed ultrasound, antiedema massage, and low-level laser therapy may help in reducing inflammation.2,26,34
-
•
Ankle pumps, 10 to 20 pumps per hour, should be conducted in a pain-free range to decrease edema and increase circulation.26
-
•
Ambulate—weightbearing as tolerated—with axillary crutches if necessary. A semirigid orthosis, lace-up style brace, or tape provides mechanical joint stability in the frontal plane.64,65
-
•
Depending on the severity of injury, pain-free modified activity can be used to maintain cardiovascular fitness. Examples of modified activity may include deep-water pool running, swimming with a pool buoy between the legs, or stationary cycling.5,26,29
-
•
Several studies were conducted on grade 1 and grade 2 ankle inversion injuries using manipulation of the TCJ. Two studies showed manipulation of the talus in an anterior to posterior vector improved range of motion in dorsiflexion at the ankle mortise.66,67 Another study showed that manipulation of the joints and soft tissue improved dorsiflexion as well as reduced pain and edema.68
-
•
Active or passive soft tissue techniques such as Active Release Technique, Graston Technique, muscle energy technique, and transverse friction massage can be applied directly to the ligament and surrounding soft tissue structures to facilitate early ligament healing.
Numerous clinical studies support the use of transverse friction massage in the treatment of ligament sprains.69 Recently, Loghmani and Warden70 conducted a study on instrument-assisted cross-fiber massage (IACFM) and its effect on ligament healing. Bilateral MCL injuries were induced on the knees of 51 rodents. The IACFM was commenced with a Graston handheld tool on one of the rodent's MCLs 1 week postinjury, at a frequency of 3 sessions per week and for a duration of a minute. The contralateral MCL was used as the nontreated control. Histological sections were obtained 4 weeks postinjury. The scar region of the IACFM-treated ligaments, as compared with the contralateral nontreated ligaments, appeared to have greater cellularity; and the collagen fibers appeared to be aligned more longitudinally. This study suggests that IACFM may accelerate early tissue-level healing.70
A more cautious approach to treatment may be necessary if there is suspicion of a grade 3 lateral ankle sprain.26 In the opinion of one of the authors, if the initial examination reveals severe swelling, pain, and inability to bear weight, the athlete should be placed in a functional walking orthosis and instructed to ambulate with crutches in a nonweightbearing gait. Nonsteroidal anti-inflammatory drugs, ice, compression, and elevation should be used to attempt to reduce swelling and pain. A reexamination should be conducted 3 days later. If there is no observable improvement, an MRI study should be used to assess the severity of injury. If the MRI indicates a completely torn ligament, the athlete should continue to follow the above regimen for approximately 4 more days, thereby allowing the retracted ligament ends to heal appropriately before progressing to the next stage of treatment.
A brief period of nonweightbearing (1-4 days) may be necessary in the initial treatment of a syndesmotic sprain where frank diastasis of the ankle mortise is not visualized on radiographs.56 Early weightbearing may lead to undue stress on the injured syndesmotic ligaments, possibly predisposing to heterotrophic ossification in the interosseous space between the tibia and fibula.38 In the case of a syndesmotic sprain that reveals diastasis of the ankle mortise greater than 6 mm, surgical fixation with screws would be necessary to stabilize the ankle mortise and allow for proper ligament healing.26,40,51 An intact ankle mortise is necessary when attempting to push off the ground to propel forward or for cutting activities of most sports.40
Reparative phase (3-5 days, collagen production intensifies 10-14 days)
Goals include reducing inflammation, facilitating the ligament healing process, restoring active and passive ranges of motion, minimizing loss of strength, maintaining cardiovascular fitness, and starting proprioceptive rehabilitation.5,25,26
-
•
Joint mobilization and soft tissue techniques of the TCJ and the STJ to free up joint restrictions and aid in improving range of motion.2,26,66-68
-
•
Passive stretch of the gastrocnemius and soleus musculature with a towel, 3 sets of 30-second holds. Stretching on a slant board or with a pro-stretch can be incorporated when the patient can at least partially bear weight with minimal pain.
-
•
Isometric exercise should be conducted as soon as the patient can tolerate it to prevent muscle atrophy.34 Active and passive range of motion can be conducted with minimal pain in dorsiflexion, plantar flexion, eversion, and the pain-free range of inversion. The therapist may conduct 3 sets of 10 with a 3- to 5-second hold at the passive end range. The patient can conduct isometric exercises at home.
-
•
Strengthen the peroneii, tibialis anterior and extensors, and the triceps surae with Thera-Band, 3 sets of 10 to 15 reps for each muscle group.26 Also strengthen the gluteus medius musculature to prevent lateral sway.47 Once the patient can fully weight bear without pain, he can add resistance greater than body weight as tolerated. This may include standing and seated calf raises. If no weights are available, teach the patient to go up on the toes on both feet and then shift all the weight to the injured side and lower down on that leg.
-
•
Standing proprioception training can be conducted on the floor, a wobble board, or an air-filled cushion. Start with single-leg standing on a flat surface, 3 times with 30-second holds; use upper extremity support from a counter if necessary. Progress to eyes closed. Progress to exercises on an air-filled cushion. Have patient balance on a wobble board for 30 to 60 seconds conducting various drills.3,18,29 Proprioception training has been shown to reduce the occurrence and reoccurrence of ankle sprains.71,72
-
•
Proprioception training in the seated position with the Biomechanical Ankle Platform System (BAPS) board. BAPS board exercises activate the peroneus longus, tibialis anterior, and gastrocnemius musculature.73 Have the patient tap the BAPS board to the floor at 12:00, 3:00, 6:00, and 9:00 pm and then add 1:30, 4:30, 7:30, and 10:30 pm. Conduct 3 sets for 2 minutes each set. The patient may also alternate counterclockwise. When the patient can fully weight bear without pain and has demonstrated proficiency in the seated position, the BAPS exercises can be conducted standing with upper extremity support as needed.
-
•
Shoe gear modification depending on the athlete's foot structure and the playing surface.19
-
•
Modified activity can be progressed appropriately. A program to incorporate restoration of cardiovascular fitness with running may include a 5-minute warm-up with walking, followed by a 3-minute run at a very easy intensity, and then followed by a 2-minute walk; repeat run/walk repetitions for 20 to 30 minutes. When the athlete can conduct a 20-to 30-minute run session without rest periods and there is no noticeable pain or postswelling, the weekly mileage can be increased by 10%. The intensity of the training runs should only progress when the athlete regains the preinjury duration.74,75
-
•
At the end of each treatment session, apply ice therapy and other modalities to control inflammation.2
The above exercises should be conducted relatively pain-free and progressed based on the patient's response to therapy and based on the principles of ligament healing. After demonstrating proficiency in conducting the exercises under the supervision of a therapist, the patient can be given a home exercise routine. If there is an excessive increase in swelling or pain, temporarily reduce the intensity or duration of the exercises followed by inflammation control.
Remodeling phase (15-28 days, 3 weeks regain ≅60% strength, 3 months regain ≅100% strength)
Goals include restoration of tensile strength, proprioception, and return to sport.25,26
-
•
Modified training may progress and include activities such as jumping rope, higher-intensity training runs, or sprints.
-
•Incorporation of multidirectional agility drills can begin at this stage. Start with controlled exercises that are on both legs; then progress to single leg. Progress to jumping over a height, such as a low cone. Progress to increasing in speed. It is important to vary the speed and intensity of sport-specific exercises to continually challenge the proprioceptive system.76 All progressions should be performed only as pain, comfort, and stability allow.
-
◦Begin jumping forward and backward over a line.
-
◦Progress to jumping laterally over a line.
-
◦Progress to box drills: Draw a box on the floor with tape and number the boxes starting in the upper-left corner and progressing clockwise. Jump from box 1 to 4, landing as close to the exact middle of the box as possible. Variations include reversing order from box 4 to 1 and adding diagonal patterns such as 1, 3, 4, and 2.
-
◦
-
•Incorporate multidirectional sport-specific proprioceptive exercises once the athlete is able to perform the proprioceptive exercises described in the reparative phase.
-
◦On level ground, begin single-leg standing exercises incorporating sport-specific exercises such as kicking a ball, catching and throwing a ball, or swinging a bat. Progress to standing on an air-filled or foam cushion.
-
◦Begin by keeping the exercise, such as catching a ball, close to the body. Progress to throwing the ball farther from the body to force the athlete to shift his center of gravity (Fig 11A, B).
-
◦
-
•
Ladder drills can be incorporated with the athlete's program. This stage is used to create exercises and movement patterns that will increasingly challenge the neuromuscular coordination of the injured athlete. Example A—side shuffle: The athlete begins with both feet at position 1 where the L and R are located. Move the left foot first to outside of the box in front, then the right into the box next to it. Proceed as depicted. Example B—carioca: Step over with the left leg first, then behind with the right leg.
Fig 11.
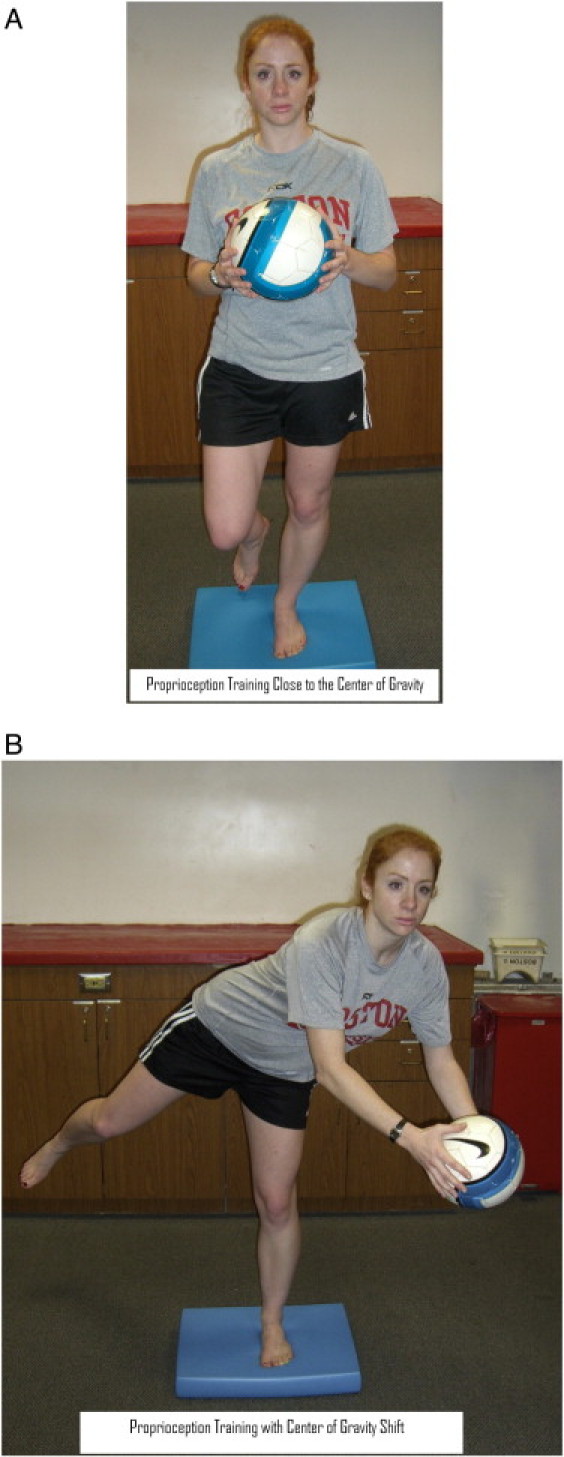
A, Proprioception training close to the center of gravity. B, Proprioception training with center of gravity shift.
The above exercises prepare the athlete to begin sport-specific drills. The athlete must be able to demonstrate proficiency in stopping, changing direction, jumping, and landing as pertaining to the specific sport before returning to practice or competition. A supportive ankle brace or taping has been shown to be an effective aid in preventing reinjury without impeding performance.77-80 Technical training (on jumping and landing), proprioceptive training, and orthosis have all been shown to decrease risk of reinjury, with technical training and proprioceptive training being more effective in those with a history of 4 or more sprains.81
Poor compliance with therapy may predispose to functional instability of the ankle. The athlete may complain of impeded sport performance due to the feeling that the ankle is unstable and fear of reinjury. Although the injured ligament may have regained preinjury tensile strength, complete proprioception rehabilitation may take longer. Upon initial return to sport, the athlete should continue to support the ankle with tape or a brace.82 To prevent reinjury, proprioception rehabilitation should continue until the athlete demonstrates improved functional skills particular to the individual sport.
After being discharged from care, the athlete should be encouraged to continue a home exercise program to ensure full restoration of impairments and to prevent reinjury. McHugh et al83 had football players with a history of ankle sprains perform single-leg stance on a foam stability pad for 5 minutes each leg. This was done 5 days a week for 4 weeks of preseason and 2 days a week for 9 weeks during the season. This was the only preventative exercise used and was done on their own. The study showed a 77% decrease in injury incidence. A study by Hupperts et al84 showed a similar decrease in injury risk with unsupervised exercises, demonstrating that a home program can be an effective tool in rehabilitation.
Limitations
A limitation of this study is that the design was not a systematic review of the literature and not all relevant literature was considered for inclusion. Therefore, not all relevant content was reviewed. As well, because this was not a systematic review, the quality of article content was not critically appraised or evaluated. Although the author team was interdisciplinary, other professions were not included; thus, resulting content may have been different if other disciplines were included. The selection of articles was that solely of the authors; therefore, there was some selection and interpretation bias. In the future, more rigorous methods should be considered for literature reviews.
Conclusion
An accurate diagnosis and prompt treatment can minimize an athlete's time lost from sport and prevent future reinjury. Most of these injuries respond favorably to an aggressive nonsurgical treatment approach. A comprehensive history and examination aid the therapist in diagnosing the severity and type of ankle sprain. Based on the diagnosis and an understanding of ligament healing properties, a progressive treatment regimen can be developed using PRICESMMS. During the acute inflammatory phase, the goal of care is to reduce inflammation and pain and to protect the ligament from further injury. During the reparative and remodeling phase, the goal is to progress the rehabilitation appropriately to facilitate healing and restore the mechanical strength and proprioception. Radiographic imaging techniques may need to be used to rule out fractures, complete ligament tears, or instability of the ankle mortise. A period of immobilization and ambulating with crutches in a nonweightbearing gait may be necessary to allow for proper ligament healing before commencing a more active treatment approach. Surgery should be considered in the case of grade 3 syndesmotic sprain injuries or those ankle sprains that are recalcitrant to conservative care.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Safran M.R., Bendetti R.S., Bartolozzi A.R., III, Mandelbaum B.R. Lateral ankle sprains: a comprehensive review part 1: etiology, pathoanatomy, histopathogenesis, and diagnosis. Med Sci Sports. 1999;31(7):S429–S437. doi: 10.1097/00005768-199907001-00004. [DOI] [PubMed] [Google Scholar]
- 2.Reid D.C. Sports injury assessment and rehabilitation. Churchill Livingston Inc.; New York: 1992. pp. 215–268. [Google Scholar]
- 3.Wester J.U., Jespersen S.M., Nielsen K.D., Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23(5):332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- 4.Munn J., Beard D., Refshauge K.M., Lee R.Y.W. Eccentric muscle strength in functional ankle instability. Med Sci Sports. 2003;35(2):245–250. doi: 10.1249/01.MSS.0000048724.74659.9F. [DOI] [PubMed] [Google Scholar]
- 5.Beynnon B.D., Vacek P.M., Murphy D., Alosa D., Paller D. First time inversion ankle ligament trauma. Am J Sports Med. 2005;33(10):1485–1491. doi: 10.1177/0363546505275490. [DOI] [PubMed] [Google Scholar]
- 6.Olmsted L.C., Vela L.I., Denegar C.R., Hertel J. Prophylactic ankle taping and bracing: a numbers-needed-to-treat and cost-benefit analysis. J Athl Train. 2004;39(1):95–100. [PMC free article] [PubMed] [Google Scholar]
- 7.LeBrun C.T., Krause J.O. Variations in mortise anatomy. Am J Sports Med. 2005;33(6):852–855. doi: 10.1177/0363546504271207. [DOI] [PubMed] [Google Scholar]
- 8.Sawkins K., Refshauge K., Kilbreath S., Raymond J. The placebo effect of ankle taping. Med Sci Sports. 2007;39(5):781–787. doi: 10.1249/MSS.0b013e3180337371. [DOI] [PubMed] [Google Scholar]
- 9.DiStefano L.J., Padua D.A., Brown C.N., Guskiewicz K.M. Lower extremity kinematics and ground reaction forces after prophylactic lace-up ankle bracing. J Athl Train. 2008;43(3):234–241. doi: 10.4085/1062-6050-43.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takao M., Uchio Y., Naito K., Fukazawa I., Ochi M. Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain. Am J Sports Med. 2005;33(5):686–692. doi: 10.1177/0363546504270566. [DOI] [PubMed] [Google Scholar]
- 11.Andersen T.E., Floerenes T.W., Arnason A., Bahr R. Video analysis of the mechanisms for ankle injury in football. Am J Sports Med. 2004;32(1):69S–79S. doi: 10.1177/0363546503262023. [DOI] [PubMed] [Google Scholar]
- 12.Giza E., Fuller C., Junge A., Dvorak J. Mechanisms of foot and ankle injuries in soccer. Am J Sports Med. 2003;31(4):550–554. doi: 10.1177/03635465030310041201. [DOI] [PubMed] [Google Scholar]
- 13.Valderrabano V., Hintermann B., Horisberger M., Fung T.S. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34(4):612–620. doi: 10.1177/0363546505281813. [DOI] [PubMed] [Google Scholar]
- 14.Purcell S.B., Schuckman B.E., Docherty C.L., Schrader J., Poppy W. Difference in ankle range of motion before and after exercise in 2 tape conditions. Am J Sports Med. 2009;37(2):383–389. doi: 10.1177/0363546508325925. [DOI] [PubMed] [Google Scholar]
- 15.Borowski L.A., Yard E.E., Fields S.K., Comstock R.D. The epidemiology of US high school basketball injuries, 2005-2007. Am J Sports Med. 2008;36(12):2328–2335. doi: 10.1177/0363546508322893. [DOI] [PubMed] [Google Scholar]
- 16.Halasi T., Kynsburg A., Tallay A, Berkes I. . Development of a new activity score for the evaluation of ankle instability. Am J Sports Med. 2004;32(4):899–908. doi: 10.1177/0363546503262181. [DOI] [PubMed] [Google Scholar]
- 17.Hyde T. Conservative management of sports injury. Williams & Wilkins; Baltimore: 1997. pp. 483–493. [Google Scholar]
- 18.Van Os A.G., Bierma-Zeinstra S.M.A., Verhagen A.P., De Bie R.A., Luijsterburg P.A.J., Koes B.W. Comparison of conventional treatment and supervised rehabilitation for treatment of acute lateral ankle sprains: a systematic review of the literature. J Orthop Sports Phys Ther. 2005;35(2):95–105. doi: 10.2519/jospt.2005.35.2.95. [DOI] [PubMed] [Google Scholar]
- 19.Banks A.S., Downey M.S., Martin D.E., Miller S.J. Foot and ankle surgery. Lipincott Williams & Wilkins; Philadelphia: 2001. pp. 1898–1902. [Google Scholar]
- 20.Chorley J.N. Ankle sprain discharge instructions from the emergency department. Pediatr Emerg Care. 2005;21(8):498–501. doi: 10.1097/01.pec.0000173346.15154.f3. [DOI] [PubMed] [Google Scholar]
- 21.Lamb S.E., Nakash R.A., Withers E.J., Clark M., Marsh J.L., Wilson S. Clinical and cost effectiveness of mechanical support for severe ankle sprains: design of a randomized controlled trial in the emergency department. BMC Musculoskelet Disord. 2005;6(1):61. doi: 10.1186/1471-2474-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beynnon B.D., Renstrom P.A., Haugh L., Uh B.S., Barker H. A prospective, randomized clinical investigation of the treatment of first-time ankle sprains. Am J Sports Med. 2006;34(9):1401–1412. doi: 10.1177/0363546506288676. [DOI] [PubMed] [Google Scholar]
- 23.Bahr R., Engebretsen L. Acute ankle sprains: a functional treatment plan for injured athletes. Consultant; 1996. pp. 675–688. [Google Scholar]
- 24.Sujitkumar P., Hadfield J.M., Yates D.W. Sprain or fracture? An analysis of 2000 ankle injuries. Arch Emerg Med. 1986;3:101–106. doi: 10.1136/emj.3.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Safran M.R., Zachazewski J.E., Benedetti R.S., Bartolozzi A.R., III, Mandelbaum R. Lateral ankle sprains: a comprehensive review part 2; treatment and rehabilitation with an emphasis on the athlete. Med Sci Sports. 1999;31(7):S438–S447. doi: 10.1097/00005768-199907001-00005. [DOI] [PubMed] [Google Scholar]
- 26.Veenema K.R. Ankle sprain: primary care evaluation and rehabilitation. J Musculoske Med. September 2000:563–576. [Google Scholar]
- 27.Williams G.N., Jones M.H., Amendola A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;25(7):1197–1207. doi: 10.1177/0363546507302545. [DOI] [PubMed] [Google Scholar]
- 28.Clanton T.O., Paul P. Syndesmotic injuries in athletes. Foot Ankle Clin N Am. 2002;7:529–549. doi: 10.1016/s1083-7515(02)00045-1. [DOI] [PubMed] [Google Scholar]
- 29.Malliaropoulos N., Ntessalen M., Papacostas E., Longo U.G., Maffulli N. Reinjury after acute lateral ankle sprains in elite track and field athletes. Am J Sports Med. 2009;10(10):1–7. doi: 10.1177/0363546509338107. [DOI] [PubMed] [Google Scholar]
- 30.Inman V.T. The Williams & Wilkins Company; Baltimore: 1976. The joints of the ankle. [Google Scholar]
- 31.Sarrafian S.K. Biomechanics of the subtalar joint complex. Clin Orthop Relat Res. 1993;290:17–26. [PubMed] [Google Scholar]
- 32.Donatelli R.A. 2nd Ed. F.A. Davis; Philadelphia: 1996. The biomechanics of the foot and ankle. [Google Scholar]
- 33.Michaud T.C. Thomas C Michaud; Newton MA: 1997. Foot orthosis and other forms of conservative foot care. [Google Scholar]
- 34.Scott W.N. The knee, volume 1. Mosby Inc.; Saint Louis MO: 1994. [Google Scholar]
- 35.Hertel J., Denegar C., Monroe M.M., Stokes W.L. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports. 1999;31(11):1501–1508. doi: 10.1097/00005768-199911000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Burks R.T., Morgan J. Anatomy of the lateral ankle ligaments. Am J Sports Med. 1994;22(1):72–76. doi: 10.1177/036354659402200113. [DOI] [PubMed] [Google Scholar]
- 37.Beumer A., van Hemert W.L.W., Swierstra B.A., Jasper L.E., Belkoff S.M. A biomechanical evaluation of the tibiofibular and tibiotalar ligaments of the ankle. Foot Ankle Int. 2003;24(5):426–429. doi: 10.1177/107110070302400509. [DOI] [PubMed] [Google Scholar]
- 38.Kennedy M.A., Sama A.E., Sigman M. Tibiofibular syndesmosis and ossification. Case report: sequelae of ankle sprain in an adolescent football player. J Emerg Med. 2000;18(2):233–240. doi: 10.1016/s0736-4679(99)00201-2. [DOI] [PubMed] [Google Scholar]
- 39.Mei-Dan O., Kots E., Barchilon V., Massarwe S., Nyska M., Mann G. A dynamic ultrasound examination for the diagnosis of ankle syndesmotic injury in professional athletes. Am J Sports Med. 2009;37(5):1009–1016. doi: 10.1177/0363546508331202. [DOI] [PubMed] [Google Scholar]
- 40.Taylor D.C., Tenuta J.J., Uhorchak J.M., Arciero R.A. Aggressive surgical treatment and early return to sports in athletes with grade III syndesmosis sprains. Am J Sports Med. 2007;35(11):1833–1838. doi: 10.1177/0363546507304666. [DOI] [PubMed] [Google Scholar]
- 41.Santilli V., Frascarelli M.A., Paoloni M., Frascarelli F., Camerota F., DeNatale L. Peroneus longus muscle activation pattern during gait cycle in athletes affected by functional ankle instability. Am J Sports Med. 2005;33(8):1183–1187. doi: 10.1177/0363546504274147. [DOI] [PubMed] [Google Scholar]
- 42.Baechle T.R. Human Kinetics; Champaign IL: 1994. Essentials of strength training and conditioning. [Google Scholar]
- 43.Moore K.L., Dalley A.F. Lippincott Williams & Wilkins; Philadelphia: 1999. Clinically oriented anatomy. [Google Scholar]
- 44.Konradsen L., Olesen S., Hansen H.M. Ankle sensorimotor control and eversion strength after acute ankle inversion injuries. Am J Sports Med. 1998;26(1):72–77. doi: 10.1177/03635465980260013001. [DOI] [PubMed] [Google Scholar]
- 45.Konradsen L., Voigt M., Hojsgaard C. Ankle inversion injuries: the role of the dynamic defense mechanism. Am J Sports Med. 1997;25(1):54–55. doi: 10.1177/036354659702500110. [DOI] [PubMed] [Google Scholar]
- 46.Delahunt E., Monaghan K., Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am J Sports Med. 2006;34(12):1970–1976. doi: 10.1177/0363546506290989. [DOI] [PubMed] [Google Scholar]
- 47.Wilkerson G.B., Pinerola J.J., Caturano R.W. Invertor versus evertor peak torque and power deficiencies associated with later ankle ligament injury. J Orthop Sports Phys Ther. 1997;26(2):78–86. doi: 10.2519/jospt.1997.26.2.78. [DOI] [PubMed] [Google Scholar]
- 48.Hollis J.M., Blasier R.D., Flahiff C.M. Simulated lateral ankle ligamentous injury: change in ankle stability. Am J Sports Med. 1995;23(6):672–676. doi: 10.1177/036354659502300606. [DOI] [PubMed] [Google Scholar]
- 49.Verhagen E., Van der Beek A., Twisk J., Bouter L., Bahr R., Van Mechelen W. The effect of a proprioceptive balance board training program for the prevention of ankle sprains. Am J Sports Med. 2004;32(6):1385–1393. doi: 10.1177/0363546503262177. [DOI] [PubMed] [Google Scholar]
- 50.Palmieri-Smith R., Hopkins J.T., Brown T.N. Peroneal activation deficits in persons with functional ankle instability. Am J Sports Med. 2009;37(5):982–988. doi: 10.1177/0363546508330147. [DOI] [PubMed] [Google Scholar]
- 51.Uys H.D., Rijke A.M. Clinical association of acute lateral ankle sprain with syndesmotic involvement. Am J Sports Med. 2002;30(6):816–822. doi: 10.1177/03635465020300061101. [DOI] [PubMed] [Google Scholar]
- 52.Wright R.W., Barile R.J., Surprenant D.A., Matava M.J. Ankle syndesmosis sprains in national hockey league players. Am J Sports Med. 2004;32(8):1941–1945. doi: 10.1177/0363546504264581. [DOI] [PubMed] [Google Scholar]
- 53.Haraguchi N., Toga H., Shiba N., Kato F. Avulsion fracture of the lateral ankle ligament complex in severe inversion injury: incidence and clinical outcome. Am J Sports Med. 2007;35(7):1144–1152. doi: 10.1177/0363546507299531. [DOI] [PubMed] [Google Scholar]
- 54.Takao M., Innami K., Matsushita T., Uchio Y., Ochi M. Arthroscopic and magnetic resonance image appearance and reconstruction of the anterior talofibular ligament in cases of apparent functional ankle instability. Am J Sports Med. 2008;36(8):1542–1547. doi: 10.1177/0363546508315537. [DOI] [PubMed] [Google Scholar]
- 55.McGrew C.A., Schenck R.C., Jr Ankle sprains: how to avoid the pitfalls, resolve the symptoms, and return patients to full function. J Musculoske Med. 2003;20(i1):34–37. [Google Scholar]
- 56.Nussbaum E.D., Hosea T.M., Sieler S.D., Incremona B.R., Kessler D.E. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29(1):31–35. doi: 10.1177/03635465010290011001. [DOI] [PubMed] [Google Scholar]
- 57.Verhagen R.A.W., Mass M., Dijkgraaf M.G.W., Tol J.L., Van Dijk C.N. Prospective study on diagnostic strategies in osteochondral lesions of the talus: is MRI superior to helical CT? J Bone Joint Surg Am. 2005;87-B(1):41–46. [PubMed] [Google Scholar]
- 58.Alanen V., Taimela S., Jaakko K., Koskinen K.S., Karaharju E. Incidence and clinical significance of bone bruises after supination injury of the ankle: a double-blind, prospective study. J Bone Joint Surg Am. 1998;80-B(3):513–515. doi: 10.1302/0301-620x.80b3.8404. [DOI] [PubMed] [Google Scholar]
- 59.Nam E.K., Ferkel R.D., Applegate G.R. Autologous chondrocyte implantation of the ankle. Am J Sports Med. 2009;37(2):274–283. doi: 10.1177/0363546508325670. [DOI] [PubMed] [Google Scholar]
- 60.O'Loughlin P.F., Heyworth B.E., Kennedy J.G. Current concepts in the diagnosis and treatment of osteochrondral lesions of the ankle. Am J Sports Med. 2009;20(10):1–13. doi: 10.1177/0363546509336336. [DOI] [PubMed] [Google Scholar]
- 61.Cotran R.S., Kumar V., Robbins S.L. 4th Ed. WB Saunders Company; Philadelphia: 1989. Robbins pathologic basis of disease. [Google Scholar]
- 62.Bleakley C.M., O'Connor S., Tully M.A., Rocke L.G., MacAuley D.C., McDonough S.M. The PRICE study (protection rest ice compression elevation): design of a randomized controlled trial comparing standard versus cryokinetic ice applications in the management of acute ankle sprain. BMC Musculoskelet Disord. 2007;8:125. doi: 10.1186/1471-2474-8-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bleakley C., McDonough S., MacAuley D. The use of ice in the treatment of acute soft-tissue injury. Am J Sports Med. 2004;32(1):251–261. doi: 10.1177/0363546503260757. [DOI] [PubMed] [Google Scholar]
- 64.Cordova M.L., Ingersoll C.D., Palmieri R.M. Efficacy of prophylactic ankle support: an experimental perspective. J Athl Train. 2002;37(4):446–457. [PMC free article] [PubMed] [Google Scholar]
- 65.Cordova M.L., Scott B.D., Ingersoll C.D., Leblanc M.J. Effects of ankle support on lower-extremity functional performance: a meta-analysis. Med Sci Sports. 2005;37(4):635–641. doi: 10.1249/01.mss.0000159141.78989.9c. [DOI] [PubMed] [Google Scholar]
- 66.Green T., Refshauge K., Crosbie J., Adams R. A randomized control trial of a passive accessory joint mobilization on acute ankle inversion sprains. Phys Ther. 2001;81(4):984–994. [PubMed] [Google Scholar]
- 67.Lopez-Rodriguez S., Penas C.F., Alburquerque-Sendin F., Rodriguez-Blanco C., Palomeque-del-Cerro L. Immediate effects of manipulation of the talocrural joint on stabilometry and baropodometry in patients with ankle sprain. J Manipulative Physiol Ther. 2007:186–192. doi: 10.1016/j.jmpt.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 68.Eisenhart A.W., Gaeta T.J., Yens D.P. Osteopathic manipulative treatment in the emergency department for patients with acute ankle injuries. J Am Osteopath Assoc. 2003;103(9):417–421. [PubMed] [Google Scholar]
- 69.Walker J.M. Deep transverse frictions in ligament healing. J Orthop Sports Phys Ther. 1984;6(2):89–94. doi: 10.2519/jospt.1984.6.2.89. [DOI] [PubMed] [Google Scholar]
- 70.Loghmani M.T., Warden S.J. Instrument-assisted cross-fiber massage accelerates knee ligament healing. J Orthop Sports Phys Ther. 2009;39(7):506–514. doi: 10.2519/jospt.2009.2997. [DOI] [PubMed] [Google Scholar]
- 71.McGuine T.A., Keene J.S. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2006;34(7):1103–1111. doi: 10.1177/0363546505284191. [DOI] [PubMed] [Google Scholar]
- 72.Tyler T.F., McHugh M.P., Mirabella M.R., Mullaney M.J., Nicholas S.J. Risk factors for noncontact ankle sprains in high school football players. Am J Sports Med. 2006;34(3):471–475. doi: 10.1177/0363546505280429. [DOI] [PubMed] [Google Scholar]
- 73.Soderberg G.L., Cook T.M., Rider S.C., Stephenitch B.L. Electromyographic activity of selected leg musculature in subjects with normal and chronically sprained ankles performing on a BAPS board. Phys Ther. 1991;71(7):514–522. doi: 10.1093/ptj/71.7.514. [DOI] [PubMed] [Google Scholar]
- 74.Edwards P.H., Jr, Wright M.L., Hartman J.F. A practical approach for the differential diagnosis of chronic leg pain in the athlete. Am J Sports Med. 2005;33:1241. doi: 10.1177/0363546505278305. [DOI] [PubMed] [Google Scholar]
- 75.Kortebein P.M., Kaufman K.R., Basford J.R., Stuart M.J. Medial tibial stress syndrome. Med Sci Sports. 2000;32(2):S27–S33. doi: 10.1097/00005768-200003001-00005. [DOI] [PubMed] [Google Scholar]
- 76.Mattacola C.G., Dwyer M.K. Rehabilitation of the ankle after acute sprain or chronic instability. J Athl Train. 2002;37(4):413–429. [PMC free article] [PubMed] [Google Scholar]
- 77.Preston W.J., Nigg B.M. The effect of an ankle orthosis on ankle range of motion and performance. J Orthop Sports Phys Ther. 1996;23(6):362–369. doi: 10.2519/jospt.1996.23.6.362. [DOI] [PubMed] [Google Scholar]
- 78.Handoll H.H.G., Rowe B.H., Quinn K.M., De Bie R. Interventions for preventing ankle ligament injuries. Cochrane Library. 2008;Volume 4 doi: 10.1002/14651858.CD000018. [DOI] [PubMed] [Google Scholar]
- 79.Sankey R.A., Brooks J.H.M., Kemp S.P.T., Haddad F.S. The epidemiology of ankle injuries in professional rugby union players. Am J Sports Med. 2008;10(10):1–10. doi: 10.1177/0363546508322889. [DOI] [PubMed] [Google Scholar]
- 80.Gross M.T., Clemence L.M., Cox B.D., McMillan H.P., Meadows A.F., Piland C.S. Effect of ankle orthoses on functional performance for individuals with recurrent lateral ankle sprains. J Orthop Sports Phys Ther. 1997;25(4):245–252. doi: 10.2519/jospt.1997.25.4.245. [DOI] [PubMed] [Google Scholar]
- 81.Sastinopoulos D. Comparison of three preventive methods in order to reduce the incidence of ankle inversion sprains among female volleyball players. Br J Sports Med. 2004;38:182–185. doi: 10.1136/bjsm.2002.003947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Refshauge K.M., Raymond J., Kilbreath S.L., Pengel L., Heijnen I. The effect of ankle taping on detection of inversion-eversion movements in participants with recurrent ankle sprain. Am J Sports Med. 2009;37(2):371–375. doi: 10.1177/0363546508324309. [DOI] [PubMed] [Google Scholar]
- 83.McHugh M.P., Tyler T.F., Mirabella M.R., Mullaney M.J., Nicholas S.J. The effectiveness of a balance training intervention in reducing the incidence of noncontact ankle sprains in high school football players. Am J Sports Med. 2007;35:1289–1294. doi: 10.1177/0363546507300059. [DOI] [PubMed] [Google Scholar]
- 84.Hupperts M.D., Verhagen E.A., van Mechelen W. Effect of unsupervised home based proprioceptive training on recurrences of ankle sprain: randomised controlled trial. BMJ. 2009;339:1–6. doi: 10.1136/bmj.b2684. [DOI] [PMC free article] [PubMed] [Google Scholar]


