Abstract
Purpose
To evaluate the safety and efficacy of higher fluence cornea collagen cross linking (CXL).
Methods
Twenty-one patients with bilateral keratoconus had randomized CXL in one eye (group A) with 7 mw/cm2 for 15 minutes; the other eye (group B) had the standard 3 mw/cm2 for 30 minutes; 50 um PTK with the Eye-Q 400 Hz Excimer laser (Wavelight, Erlagen, Germany) was used for epithelial removal. The patients were evaluated postoperatively at the following intervals: day 1, day 4, month 1, month 3, and then every 6 months.
Results
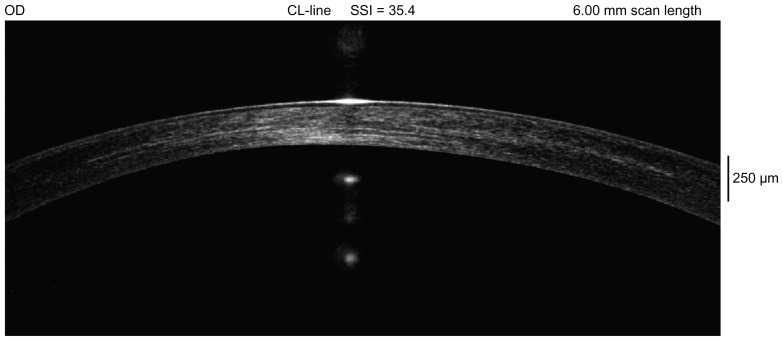
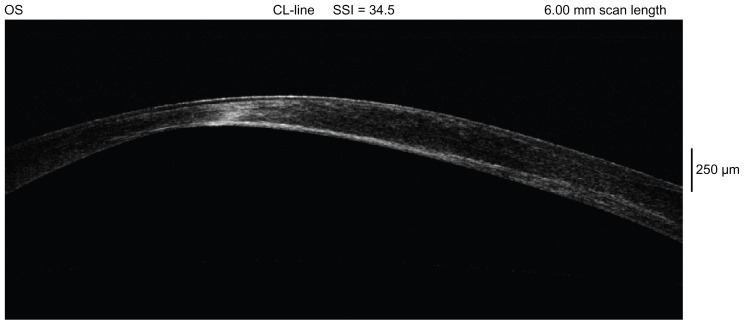
For groups A and B respectively, in mean values: uncorrected distance visual acuity (UDVA) improved from 20/60 to 20/38, and 20/62 to 20/40; best corrected visual acuity (BCVA) from 20/30 to 20/25 in both groups; mean sphere was reduced by 2.5 and 2.1 diopters; mean cylinder was reduced by 2.9 and 2.5 diopters on average; Steepest K was reduced from 49.5 to 46.1, and from 48.7 to 45.8 diopters. There was no ectasia progression in any of the cases during the follow-up time studied. There was no change in the endothelial cell count. All patients returned to full activities postoperatively within a month. Four cases from group A and five cases from group B had delayed epithelial healing (completed by postoperative day 9). No other adverse effects were noted in any of the cases studied. Mean follow-up was 46 months (18–56). Corneal optical coherence tomography (OCT) revealed diffused light scattered in anterior two-thirds of the cornea stroma, which was more intense and much broader in diameter in group A than in group B.
Conclusion
This novel technique offers similar clinical results in ectasia stabilization without any adverse effects noted.
Keywords: cornea collagen cross linking (CXL), ectasia management, keratoconus management, higher fluence ultraviolet light
Introduction
The management of keratoconus (KCN) with collagen cross linking (CXL), utilizing UV irradiation and simultaneous topical riboflavin administration, has been studied at length. This has taken place both in laboratory work as well as clinical work,1–14 and received the CE mark of approval, in December 2006, for clinical use in countries in the European Union. The standard technique described by Wollensak et al involves partial or complete central epithelial removal, followed by topical administration of riboflavin 0.1% solution in order to achieve intra-stromal penetration.1
We theorized that by increasing the UV light fluence we targeted the following: (1) a faster procedure, as the fluence time is shortened, and (2) shorter keratocyte exposure time and potentially less fibrocyte cornea damage caused.
Methods
Twenty-one patients with bilateral progressive keratoconus were studied. The study is a prospective randomized comparative case series. These patients were selected with the following criteria:
Topographic and tomographic evidence of keratoconus (K > 45 and/or inferior steepening greater than 1 diopter to the superior half of the cornea, and 1 diopter of tomographic cylinder progression over 1 year.)
Minimum cornea thickness at or over 450 microns.
Age at or over 18 years.
Refer to Table 1 for pre-op and post-op: refraction, corrected distance visual acuity (CDVA), UDVA, IOP, corneal endothelial cell count, and the figures for ultrasound cornea pachymetry (UCP), cornea tomography (Oculyzer; Wavelight, Erlangen, Germany), and OCT cornea imaging (Optovue Inc, Fremont, CA), with a minimum of 28 months follow-up.
Table 1.
Summary of perioperative data
| Variable | 7 mW/cm2 – group A | 3 mW/cm2 – group B |
|---|---|---|
| UDVA pre-op | 20/60 | 20/62 |
| UDVA post-op | 20/38 | 20/40 |
| CDVA pre-op | 20/30 | 20/30 |
| CDVA post-op | 20/25 | 20/25 |
| Spherical equivalent change | −2.5D (1.4–3.1) | −2.3D (1.3–2.9) |
| Refractive cylinder change | −2.9D (1.5–3.4) | −2.8D (1.6–3.3) |
| Topometric cylinder change (steepest K) | −3.4D (1.6–4.1) | −2.9D (1.7–3.8) |
| Endothelial cell change | −100 | −250 |
| Delayed epithelial healing | 4 | 5 |
| Complications | 0 | 0 |
Abbreviations: UDVA, uncorrected distance visual acuity; CDVA, corrected distance visual acuity; D, diopter.
Surgical technique
Phototherapeutic keratectomy (PTK) epithelial removal: under topical 1% proparacaine anesthesia (Alcaine, Alcon, Fort Worth, Texas), the Wavelight 400 Hz Excimer laser was used for PTK with the parameters of 6.5 mm optical zone, 50 um depth of tissue removal. This mode was used instead of manual epithelial removal for several reasons: (1) to avoid ethanol-related cornea toxicity, and (2) to use the epithelium as a masking agent in epithelial removal, anticipating that this mode would perhaps remove Bowman’s membrane and possibly some stroma over the area of the cone, as the epithelium there is usually significantly thinner.
Collagen cross-linking: 0.1 ml of 0.1% of riboflavin solution was administered every 30 seconds for 5 minutes (10 drops) until the de-epithelialized cornea was a bright yellow color, due to the presence and stromal infiltration of the riboflavin solution. The preceding removal of Bowman’s membrane at the cone area facilitated rapid riboflavin solution diffusion within the stroma within 5 minutes. The cornea was then exposed to UV light: group A with 7 mW/cm2 for 15 minutes and group B for the standard 3 mW/cm2 for 30 minutes.
A UV irradiation source of an average 370 nm wavelength (365–375 nm) was used to irradiate the corneal surface. The effective fluence at the corneal surface was calibrated at 7 mW/cm2 and lasted 15 minutes. The total amount of UV irradiation delivered at an 8 mm-diameter corneal plane was calculated to be 6.3 joules (in comparison to 5.4 joules for group B).
Post-op medicines included topical ofloxacin four times daily for 1 week, and a combination of chlorampenicol and 1% prednisolone acetate (Dispersadron C, Alcon) four times daily for a month and twice daily for another month. Vitamin C – 1000 mg per day – was administered orally for 2 months, and patients were encouraged to avoid direct sunlight. The patients were evaluated at postoperative day 1, day 4, month 1, month 3, and then every 6 months.
Results
Table 1 documents the pre- and post-UDVA, CDVA, Steepest K, Min K, endothelial cell count (ECC), Pentacam thickness, OCT thickness and hyper-reflectivity. The results for groups A and B in mean values respectively are: UDVA improved from 20/60 to 20/40, BSCVA from 20/30 to 20/25, mean sphere was reduced by 2.4 diopters, mean cylinder was reduced by 2.9 diopters on average, Steepest K was reduced from 49.5 to 46.1 diopters. There was no ectasia progression in any of the cases during the follow-up time studied and there was no change in the endothelial cell count.
There was an initial reduction of cornea pachymetry at 1 month, at about 20% of the preoperative pachymetry measurement. The mean thinnest cornea pachymetry appeared to increase at 18 months follow-up by 25%, on average, when compared to postoperatives in the first month, and by 5% when compared to the preoperative pachymetry measurement. All patients returned to full activities postoperatively within a month. Four cases from group A and five cases from group B had delayed epithelial healing (completed in day nine). No other adverse effects were noted in any of the cases studied. Mean follow-up was 46 months (18–56).
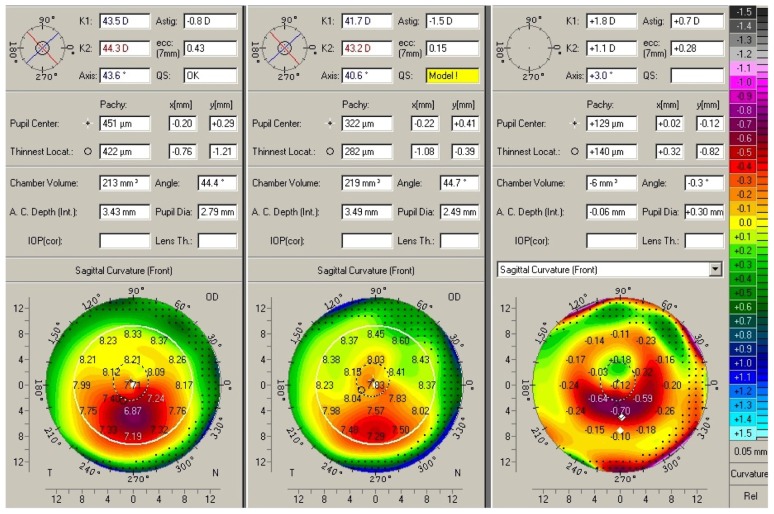
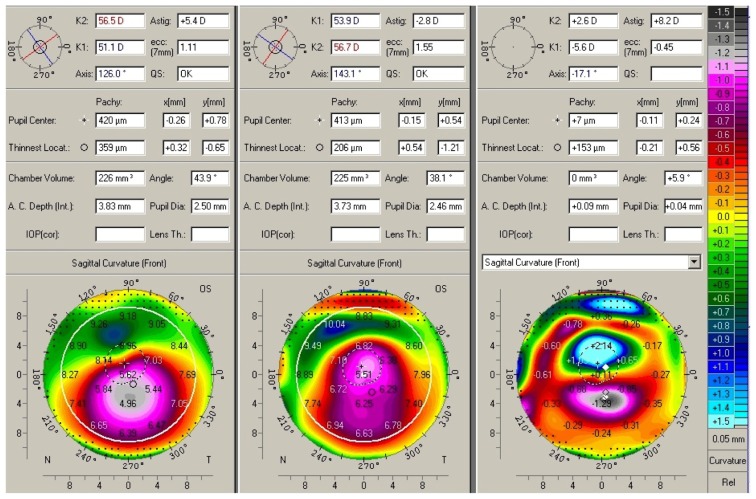
Representative pre- and postoperative tomographies for two eyes from group A, along with their topographic difference, are displayed in Figures 1 and 2. Slit lamp biomicroscopy revealed no long term epithelial defects, and diffuse light scattering in anterior 2/3 of the cornea stroma, consistent with our clinical findings from the standard CXL technique, was more intense and much broader in diameter in group A (Figures 3 and 4).
Figure 1.
Pre (left), post (center), and difference (right) topography maps from an indicative case of Group A.
Figure 2.
Pre (left), post (center), and difference (right) topography maps and keratometric data of an additional indicative case of Group A.
Figure 3.
A 1 year postoperative cornea OCT from a case from Group A (also studied in Figure 1). There is very wide and deep stromal hyper-reflectivity representing effective large stromal volume cross-linking.
Figure 4.
This is an 18 month postoperative cornea OCT of a case from Group A (same case shown in Figure 2). The extreme cornea thinning is evident, along with deep stroma hyper-reflectivity representing effective large stromal volume cross-linking.
Discussion
We have clinically applied CXL, utilizing ultraviolet A irradiation and riboflavin solution in cornea ectasia, keratoconus and bullous keratopathy over the last 6 years.12–16,18–24 We have previously presented and reported the employment of higher fluence CXL with riboflavin solution administration via a femtosecond created intracorneal pocket.22
CXL was shown to have a documented benefit to corneal ectatic disorders. One of the shortcomings with the standard Dresden protocol are lengthy exposure duration (30 minutes). Post-operative pain, delayed epithelial healing, and delayed visual rehabilitation for 1 to 2 weeks postoperatively are some of the other shortcomings.
The contributing elements in the CXL photo-oxidative and biochemical reactions are riboflavin, UVA light, oxygen, and stromal collagen. There is a potential limit of oxygen availability and absorption by riboflavin within the stroma during the length of standard cross-linking procedure. If the riboflavin was already present in the cornea stroma, a larger portion of UVA light may pass through the cornea epithelium and produce the photochemical reaction in the cornea stroma instead of the eye’s surface, therefore facilitating more efficient intra-stromal cross-linking and potentially less collateral toxicity to the cornea surface.
In the standard technique, the riboflavin-soaked cornea stroma absorbs the UVA light and, with oxygen, produces a photo-oxidative reaction (type 2). The product is a free radical oxygen molecule, which facilitates a biochemical reaction within stromal collagen. We speculate that it generates fiber to fiber bonds, or bonds between proteoglycans and collagen fibrils,25 leading to higher stromal rigidity.
The novel method described herein, where higher fluence UV light is used with shorter exposure, appears to be safe and effective in stabilizing keratoconus.
This technique appears to be similar but more comfortable for the patients. It requires half UV exposure time, has similar first night discomfort, and all patients returned to pre-op visual function with no epithelial defect by week one (on average).
Would there be a reduced stromal keratocyte loss, compared to that reported with the standard technique,17 because there is a shorter duration of UV exposure with higher fluence? Most human cells are believed to be more resistant to short or pulsed exposure to UV light, rather than longer and continuous exposure. Does this procedure pose less risk for postoperative infectious keratitis, again due to the shorter duration and the higher fluence providing a “dis- infective effect”?
In our early clinical experience, this new technique has been very rewarding in regard to the cross-linking effect.
This technique may become an alternative CXL technique for the prevention and stabilization of cornea ectasia. In our opinion, it may become an effective application as an adjunct prophylactic treatment in routine ‘Laser Assisted In-Situ Keratomileusis’ (LASIK) cases, when cornea ectasia may be a possible concern. Further studies and longer follow-up are needed to validate these data.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–627. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 2.Wollensak G. Crosslinking treatment of progressive keratoconus: new hope. Curr Opin Ophthalmol. 2006;17:356–360. doi: 10.1097/01.icu.0000233954.86723.25. [DOI] [PubMed] [Google Scholar]
- 3.Mazzotta C, Balestrazzi A, Traversi C, et al. Treatment of progressive keratoconus by riboflavin-UVA-induced cross-linking of corneal collagen. Cornea. 2007;26:390–397. doi: 10.1097/ICO.0b013e318030df5a. [DOI] [PubMed] [Google Scholar]
- 4.Kanellopoulos AJ. Post LASIK ectasia. Letter to the editor. J Ophthalmol. 2007;114(6):1230. doi: 10.1016/j.ophtha.2007.03.041. [DOI] [PubMed] [Google Scholar]
- 5.Kanellopoulos A, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK. A temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26:891–895. doi: 10.1097/ICO.0b013e318074e424. [DOI] [PubMed] [Google Scholar]
- 6.Spoerl E, Mrochen M, Sliney D, et al. Safety of UVA riboflavin crosslinking of the cornea. Cornea. 2007;26:385–389. doi: 10.1097/ICO.0b013e3180334f78. [DOI] [PubMed] [Google Scholar]
- 7.Seiler T, Hafezi F. Corneal cross-linking-induced stromal demarcation line. Cornea. 2006;25:1057–1059. doi: 10.1097/01.ico.0000225720.38748.58. [DOI] [PubMed] [Google Scholar]
- 8.Wollensak G, Spoerl E, Seiler T. Stress-strain measurement of human and porcine corneas after riboflavin-ultraviolet-A-induced cross-linking. J Cat Refr Surg. 2003;29:1780–1785. doi: 10.1016/s0886-3350(03)00407-3. [DOI] [PubMed] [Google Scholar]
- 9.Spoerl E, Huhle M, Seiler T. Induction of cross-links in corneal tissue. Exp Eye Res. 1998;66:97–103. doi: 10.1006/exer.1997.0410. [DOI] [PubMed] [Google Scholar]
- 10.Hafezi F, Kanellopolous J, Wiltfang R, et al. Corneal collagen cross linking with riboflavin and ultraviolet A to treat induced kerectasia after laser in situ keratomileusis. J Cat Refr Surg. 2007;33:2035–2040. doi: 10.1016/j.jcrs.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 11.Kanellopoulos AJ. Cross-linking plus topography-guided PRK for post-LASIK ectasia management. In: Ashok G, editor. Mastering Advanced Surface Ablation Techniques. Jaypee Brothers; 2007. [Google Scholar]
- 12.Kanellopoulos AJ. Video technique on sequential topography-guided partial PRK followed by collagen cross-linking in keratoconus. In: Ashok G, editor. Video Atlas of Ophthalmic Surgery. Jaypee Brothers; 2007. [Google Scholar]
- 13.Kanellopoulos AJ. Photorefrative keratectomy and Collagen cross-linking (PRK and C3-R) In: Boxer-Wachler Brian S., editor. Modern Management of Keratoconus. Jaypee Brothers; 2007. [Google Scholar]
- 14.Kanellopoulos AJ. Managing highly distorted corneas. Refractive surgery subspecialty day syllabus. Proceedings of the refractive surgery at AAO; New Orleans. Nov 2007. [Google Scholar]
- 15.Krueger R, Esteban RJ, Kanellopoulos AJ. Staged, intrastromal delivery of riboflavin with UVA cross-linking in advanced bullous keratopathy: laboratory investigation and first clinical case. J Cataract Refract Surg. 2008;24:S730–S736. doi: 10.3928/1081597X-20080901-17. [DOI] [PubMed] [Google Scholar]
- 16.Kanellopoulos AJ. Cross-linking plus topography-guided PRK for post-LASIK ectasia management. In: Ashok G, Emanuel R, editors. Instant Clinical Diagnosis in Ophthalmology Refractive Surgery. Jaypee Brothers; 2008. [Google Scholar]
- 17.Wollensak G, Spoerl E, Reber F, et al. Keratocyte cytotoxicity of riboflavin/ultraviolet-A treatment in vitro. Eye. 2004:1–5. doi: 10.1038/sj.eye.6700751. [DOI] [PubMed] [Google Scholar]
- 18.Kanellopoulos AJ. Prophylactic collagen crosslinking in high risk femtosecond assisted-LASIK: a novel technique. In: Ashok G, Jorge LA, editors. Surgical Techniques in Ophthalmology-Refractive Surgery. Jaypee-Highlights; 2009. pp. 423–426. [Google Scholar]
- 19.Kanellopoulos AJ. Simultaneous prophylactic collagen cross-linking (CXL) following high-risk topography-guided PRK (tPRK) In: Ashok G, Jorge LA, editors. Surgical Techniques in Ophthalmology-Refractive Surgery. Jaypee-Highlights; 2009. pp. 427–430. [Google Scholar]
- 20.Kanellopoulos AJ. Simultaneous collagen cross-linking (CXL) and topography-guided PRK (tPRK) for keratoconus (KCN) In: Ashok G, Jorge LA, editors. Surgical Techniques in Ophthalmology-Corneal Surgery. Jaypee-Highlights; 2009. pp. 18–21. [Google Scholar]
- 21.Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25:S812–S818. doi: 10.3928/1081597X-20090813-10. [DOI] [PubMed] [Google Scholar]
- 22.Kanellopoulos AJ. Collagen cross-linking in early keratoconus with riboflavin in a femtosecond laser-created pocket: initial clinical results. J Refract Surg. 2009;25:1034–1038. doi: 10.3928/1081597X-20090901-02. [DOI] [PubMed] [Google Scholar]
- 23.Krueger RR, Kanellopoulos AJ. Stability of simultaneous topography-guided photorefractive keratectomy and riboflavin/UVA cross-linking for progressive keratoconus: case reports. J Refract Surg. 2010;26:S827–S832. doi: 10.3928/1081597X-20100921-11. [DOI] [PubMed] [Google Scholar]
- 24.Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same–day, topography-guided partial transepithelial PRK and collagen cross-linking: the Athens protocol. J Refract Surg. 2010 doi: 10.3928/1081597X-20101105-01. online advance released. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, Conrad AH, Conrad GW. Effects of ultraviolet-A and riboflavin on the interaction of collagen and proteoglycans during corneal cross-linking. J Biol Chem. 2011;286:13011–13022. doi: 10.1074/jbc.M110.169813. [DOI] [PMC free article] [PubMed] [Google Scholar]