Abstract
Background
Previous studies have shown that minority populations have low rates of documented advance directives and express preferences for more life-prolonging interventions at the end of life. We sought to determine the impact of Latino ethnicity on patients' self-report of having an advance directive discussion and having a completed advance directive in the medical record at an index hospitalization for serious medical illness.
Methods
This was a prospective observational cohort study of 458 adults admitted to the general medical services of a safety net hospital, an academic medical center, and a Veterans' Affairs (VA) hospital. Patients were asked if they had discussed advance directives, and we reviewed medical records for documented advance directives.
Results
Overall, 45% of patients reported having had a discussion about advance directives (29% of Latinos compared with 54% of Caucasians, p=0.0002) and 24% of patients had a completed advance directive in their medical record (25% Latinos and 26% of Caucasians, p=not significant [ns]). Using logistic regression modeling and adjusting for socioeconomic status (SES), education level, and language spoken, Latinos (odds ratio [OR] 0.42, confidence interval [CI] 0.24–0.75) were less likely to report having advance directive discussions compared with Caucasians (referent). However, modeling of a completed advance directive in the medical record showed no significant difference between Latinos (OR 1.44, CI 0.73–2.85) and Caucasians (referent).
Conclusions
The unexpected discrepancy we found highlights the need for more effective communication in advance care planning that includes education that is culturally sensitive and accessible to persons with low health literacy.
Introduction
Following passage of the Patient Self Determination Act (PSDA) in 1990,1 advance directives (ADs) became part of the hospital admission process. In the intervening 20 years since the passage of the PSDA, completion rates of ADs remain low at 18 to 36% of adults.2,3 Less than half of adults with a serious chronic or life-limiting illness have completed an AD and many physicians are unaware their patients have completed an AD.4,5
Advance care planning protects patient autonomy and can communicate patient preferences for care at the end of life. Recent research has demonstrated that ADs do not decrease survival and can benefit patients at the end of life.8,9 In Silveira and colleagues' recent nationwide study of decedent adults, they found that for those who completed an AD, care at the end of life was significantly more likely to be consistent with previously stated preferences.9 Furthermore, in patients with advanced cancer, simply engaging in discussions about wishes at the end of life with their physician increased the likelihood that care was consistent with preferences.10
In addition, cross-cultural research suggests one model for end-of-life care does not fit all. Indeed, there are multiple studies demonstrating that care preferences among ethnic minorities at the end of life differ from those of Caucasians.11–13 In several studies, when compared with Caucasians, African Americans and Latinos expressed a wish for aggressive therapies and more life-prolonging interventions over comfort care, even if life could be extended by only days.11 Ethnic minorities also tend to express a greater preference for death in a hospital rather than at home11,12 and appear less likely to complete ADs.11,14 Multiple barriers to AD completion have been identified including language, lack of knowledge, poor communication, and a perception that having family involved obviated the need for an AD.15–17 In a recent study of patients with advanced cancer, the presumed influences, such as religiousness, treatment preferences, and acknowledgement of terminal diagnosis, were not associated with the ethnic differences in advance care planning.11 The authors of the study postulated that communication and physician bias were possible mediators to be explored in future research.
We sought to explore the relationship between Latino ethnicity and two separate but related outcomes—whether patients reported having discussed ADs and whether they had a documented AD in the medical record. Looking at both of these outcomes allows us to not only examine ethnic differences in completion of AD, but also to examine an important barrier to completing an AD—whether patients recall if a discussion about AD even took place.
Methods
This was a multisite cross sectional observational study of adult patients admitted to the hospital for medical illness. The Colorado Multi-Institutional Review Board approved this study.
Study sites and participant recruitment
Participants were recruited from three hospitals affiliated with the University of Colorado Denver School of Medicine Internal Medicine Residency program: the Denver Veterans' Administration Center (DVAMC), a large urban Veterans' Affairs (VA) hospital; Denver Health Medical Center (DHMC), the safety net hospital for the Denver area; and University of Colorado Hospital (UCH), an academic tertiary, specialty care, and referral center. Participants, who were screened for study eligibility on the first day following admission to the adult general medical service, were recruited during 96 postadmission days between February 2004 and June 2006 (exclusion criteria: death or discharge <24 hours, pregnant, jailed, or lacking decisional capacity as determined by the treating physician). All potentially eligible patients were approached and invited to participate in a brief verbal survey that focused on ADs and preferences relating to care at the end of life.
Subject interview and measures
After informed consent was obtained, participants completed a bedside interview that included self-identified ethnicity through the Multigroup Ethnic Identity Measure (MEIM),18 a scale measuring dimensions of ethnic identity, including self-identification, affirmation/belonging, identity achievement, and ethnic behaviors and practices. In addition, participants reported socioeconomic measures (e.g., income, employment, home ownership, car ownership), measures of social support (marital status, friends and relatives with whom they are in contact, faith group, memberships in other formal organizations), if they had a primary care provider (PCP), and questions related to advance care planning as detailed below.
Interviewer: Do you know what an advance directive is?
Patient responds.
Interviewer: [Either affirms or redirects and then offers this standard explanation to all participants] An advance directive is a document or paper that tells your doctors about the kind of medical treatment you would want if you were very sick and could not make those decisions for yourself. This may include a living will, a medical decision maker or medical durable power of attorney, or a CPR directive.
Has anyone ever talked to you about advance directives?
Chart review data collection
For each participant, we performed a detailed chart review for medical history including admitting diagnoses and the CARING criteria, a set of simple criteria developed by our group to score the need for palliative care, which has been shown to predict death at one year.19 The CARING criteria is an acronym for Cancer as an admitting diagnosis, Admitted to the hospital ≥2 times in the past year for a chronic illness, Resident in a nursing home, ICU (intensive care unit) admission in multiorgan failure, and meeting ≥2 Noncancer hospice Guidelines. Each criterion and patient age are weighted so that patients may be categorized as low, medium, or high risk of death at one year. We also recorded insurance coverage, and the presence of ADs in the medical record. We defined ADs broadly, including a living will, a durable power of attorney (POA) for health care, or a comprehensive advance care planning document (e.g., Five Wishes),44 and cardiopulmonary resuscitation (CPR) directive. All responses and data were directly entered into an electronic Access© database (Microsoft Corporation, Redmond, WA).
Analysis
The statistical software SAS version 9.1 (SAS Institute Inc., Cary, NC) was used for all analyses. Simple frequencies and means statistics were used to determine rates of descriptive characteristics of the sample as well as rates of the measured outcomes, reporting an AD discussion and presence/absence of an AD in the medical record. Chi-square tests were performed for all categorical variables to determine a significant association with outcome variables. Continuous variables including summary score for the MEIM were selected for the model by performing t tests. Variables were selected for logistic regression modeling if the p value of univariable analysis was ≤0.25.20 We had 80% power to detect a 12 percentage point difference in rates of AD completion.
Logistic regression modeling
Logistic regression models were fitted to examine adjusted associations between variables selected in the univariable analysis and the outcome variables—whether the subject reported a discussion about ADs and whether there was an AD in the medical record.
Results
Study population
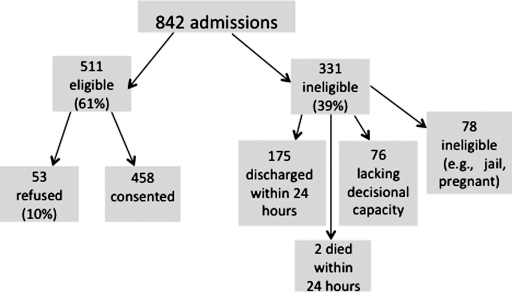
Subjects were recruited on 96 postadmission days totaling 842 admissions. Details of enrollment, eligibility, and refusal rates are presented in Figure 1. Characteristics of the 458 study participants are depicted in Table 1. Spanish was the preferred language for 31 participants (7%), whereas the rest of the patients spoke English.
Fig. 1.
Study Recruitment and enrollment.
Table 1.
Sample Characteristics (n=458; Percent [n] Unless Otherwise Noted)
| Mean MEIMa score (±SD) | 2.75 (±0.32) |
| Mean age in years (±SD) | 57.7 (±15) |
| Ethnicity | |
| African American | 19% (88) |
| Caucasian | 52% (239) |
| Latino | 22% (102) |
| Other | 6% (29) |
| Spanish language only | 6% (31) |
| Female gender | 35% (159) |
| Admitted to DVAMC | 41% (188) |
| Admitted to DHMC | 38% (174) |
| Admitted to UCH | 21% (96) |
| CARING criteria | |
| Cancer diagnosis | 11% (51) |
| Admitted to hospital ≥2 times in the past year for chronic illness | 40% (181) |
| Resident in a nursing home | 2% (9) |
| Noncancer Hospice Guidelines (meeting ≥2) | 13% (59) |
| Income less than $30,000/year | 82% (377) |
| No greater than high school education | 54% (248) |
| Home owner | 27% (125) |
| Rents home | 39% (177) |
| Unstable living situationb | 34% (156) |
| Low social supportc | 37% (169) |
| Uninsured | 18% (81) |
| Regular primary care provider | 73% (332) |
MEIM=Multi-Ethnic Identity Measure, a continuous numeric scale of ethnic identity. Scores range from 1 to 4.
Unstable living situation defined as homeless, living in shelters, or with friends.
Low social support defined as Identifying fewer than two forms of social support (spouse/significant other, relatives, friends, church or other group) present in their life.
DHMC, Denver Health Medical Center; Denver Veterans' Administration Center, DVAMC; UCH, University of Colorado Hospital.
Effect of ethnicity on reporting advance directives discussions and presence of advance directives in the medical record
Overall, 206 study patients (45%) reported having had a discussion about ADs. However, medical record review revealed that only 110 patients (24%) had a form of documented AD in their chart. Among these, 28 patients (25%) had a living will, 43 (39%) had a durable POA, 30 (27%) had a broader AD document (e.g., Five Wishes),44 and 59 (54%) had a CPR directive. Table 2 shows the unadjusted results of our two related research questions—are there ethnic differences in reporting AD discussions and are there ethnic differences in documentation of AD in the medical record? We found Latinos were significantly less likely to have discussed AD compared with all other ethnicities. We did not find any significant differences between ethnic groups for having a documented AD in the medical record. Most importantly, for patients who reported an AD discussion, Latinos were slightly more likely than all other ethnic groups to have a documented AD in the medical record, although this difference was not statistically significant (Table 2).
Table 2.
Advance Directive Discussions and Documentation by Ethnicity
| Total | African American | Caucasian | Latino | Other | P value | |
|---|---|---|---|---|---|---|
| Reported AD discussion | 45% (n=206) | 41% (n=36) | 54% (n=128) | 29% (n=29) | 45% (n=13) | 0.0002 |
| Reported AD discussion (n=206) and had documented AD | 29% (n=59) | 22% (n=8) | 29% (n=37) | 34% (n=10) | 31% (n=4) | 0.7 |
| Had documented AD | 24% (n=110) | 19% (n=17) | 26% (n=62) | 25% (n=62) | 21% (n=6) | 0.6 |
AD, advance directive.
Variables for logistic regression modeling
In the univariable analysis, variables related to ethnicity including ethnic group and mean MEIM score were associated with the outcomes of interest with a p value ≤ 0.25, and were included in the multivariable models. Socioeconomic variables, including education level, income, and home ownership as well as social support, having a primary care provider, more severe disease (i.e., meeting CARING criteria), gender, and hospital site were all associated (p≤0.2) with having an AD discussions and documentation of an AD in the chart.
Reporting advance directive discussions—logistic regression modeling
The results of the model of reporting an AD discussion are presented in Table 3. No variables, including age, gender, disease severity, social support, or the ability to identify a PCP, were associated with recalling a discussion about AD. However, Latino ethnicity was a significant negative predictor of reporting an AD discussion. That is, after adjusting for socioeconomic status (SES), age, gender, disease severity, insurance, hospital, and PCP, Latinos were far less likely to report having discussed AD compared with Caucasians (referent group) and other ethnic groups (African American, Asian, Native American).
Table 3.
Predictors of Reporting an Advance Directive Discussion
| Predictive variables | Estimate | P value | Odds ratio | 95% Wald confidence limits | |
|---|---|---|---|---|---|
| MEIM* score | 0.11 | 0.74 | 1.12 | 0.57 | 2.19 |
| Latino ethnicity | −0.87 | 0.003 | 0.42 | 0.24 | 0.75 |
| African American ethnicity | −0.39 | 0.18 | 0.68 | 0.38 | 1.20 |
| Other minority ethnicity | −0.04 | 0.92 | 0.96 | 0.41 | 2.23 |
| Age by quintile | −0.03 | 0.73 | 0.97 | 0.81 | 1.16 |
| Female gender | −0.13 | 0.61 | 0.88 | 0.53 | 1.45 |
MEIM=Multigroup Ethic Identity Measure, a continuous numeric scale of ethnic identity. Scores range from 1 to 4.
Adjusted for socioeconomic status (income, education level, housing), presence of a primary care provider, social support, insurance, disease severity (CARING criteria), Spanish as primary language, and hospital.
Advance directives documented in the medical record—logistic regression modeling
The results of the model of having an AD documented in the medical record are presented in Table 4. Latino ethnicity was not a significant predictor for having an actual AD on the chart. Latino participants were just as likely as Caucasians and other ethnic groups (African American, Asian, and Native American) to have an AD documented in the medical record. Older age and more severe disease were the only significant predictors of having an AD documented in the medical record. There were no detectable interactions between age and ethnicity.
Table 4.
Predictors of Having an Advance Directive in the Medical Record
| Predictive variables | Estimate | P value | Odds ratio | 95% Wald confidence limits | |
|---|---|---|---|---|---|
| MEIM^ Score | −0.17 | 0.68 | 0.85 | 0.38 | 1.87 |
| Latino ethnicity | 0.36 | 0.30 | 1.44 | 0.73 | 2.85 |
| African American ethnicity | −0.08 | 0.82 | 0.92 | 0.46 | 1.86 |
| Other minority ethnicity | 0.38 | 0.49 | 1.46 | 0.50 | 4.26 |
| Age by quintile | 0.29 | 0.008 | 1.34 | 1.08 | 1.66 |
| Meeting CARING criteria | 0.70 | 0.004 | 2.01 | 1.25 | 3.24 |
| Female gender | −0.27 | 0.42 | 0.77 | 0.40 | 1.48 |
| Reported having an advance directive discussion | 0.20 | 0.41 | 1.23 | 0.76 | 2.0 |
^ *MEIM=Multi-Ethnic Identity Measure, a continuous numeric scale of ethnic identity. Scores range from 1 to 4.
Adjusted for socioeconomic status (income, education level, housing), presence of a primary care provider, social support, insurance, and hospital.
To minimize the effect of a language barrier, we repeated the analysis after removing the 31 patients who were monolingual Spanish, for whom language barriers would have been a potential impediment. Yet excluding them from the analysis had no appreciable effect on the results.
We also recognize that CPR directives may or may not be representative of ADs. The patients may be directing care for themselves, or relatives, proxies, or MD POAs may be making the decision for patients. Therefore, we completed additional analysis excluding CPR directives and our findings were unchanged.
Discussion
We found that Latinos were less likely to report having discussed ADs compared with Caucasians. Conversely, Latinos may be as likely (or even more likely although not significantly) to have an AD in the medical record as Caucasians. We did not detect any other ethnic differences in AD discussions or documentation. Our results suggest that when Latinos recalled discussing ADs, they were just as likely to have an AD documented in the medical record as Caucasians. Thus the communication discrepancy we found is a result of lower rates of reported discussions. The ultimate question is are rates of reported discussions lower among Latinos because they did not take place (physician bias) or did the discussions take place and Latinos were less likely to have understood those conversations (cultural factors, communication, and health literacy)?
Low rates overall of reported advance directive discussions and documentation
Perhaps the most important finding of our study was that less than half of our sample reported to have discussed ADs and roughly a quarter of our population had some form of AD documented in their medical record. This is particularly disconcerting given that all subjects had been admitted to the hospital within the past 24 to 48 hours, and according to the 1995 PSDA, all persons admitted to the hospital must be asked about ADs and should receive information about them.1 Our data certainly provide further evidence that this federal mandate has been largely ineffective and that information about ADs is not read or understood by a significant proportion of hospitalized adults.21
The effects of ethnicity on advance care planning
Previous studies examining ethnic differences in advance care planning have focused on preferences, with multiple studies showing a preference for more invasive, aggressive care at the end of life11–14 and lower rates of hospice utilization among African Americans and Latinos.22,23 Qualitative research suggests that health inequality and poor access to care has fostered a mistrust in the health care system and explains in part the preference for higher use of technologic interventions at the end of life.24 The literature has also demonstrated lower rates of documented ADs among ethnic minorities, although these differences may be explained in part by differences in access to care.11,13,25
Our results are unique and unexpected—we found no difference in rates of documented ADs but a startling communication discrepancy. Our study hospitals included DVAMC, which provides equal access to care for all qualifying veterans and has been previously shown to have no ethnic differences in rates of ADs in the medical record. DHMC was another of our study hospitals and is a safety-net health care system and nationally recognized for providing high-quality care without disparities.26 It may have been that the quality and equality of care at these two hospitals resulted in similar rates of documented ADs between ethnic groups. However, if the inclusion of these two model health care systems explains why rates of documented ADs did not differ, it leaves the more troubling question of why were rates of reported AD discussions so much lower among Latinos unanswered.
Possible explanatory factors may include physician bias, cultural preferences, health literacy, or poor quality of communication between patients and providers. Further studies are needed to help understand these differences as we work to improve advance care planning for all patients.
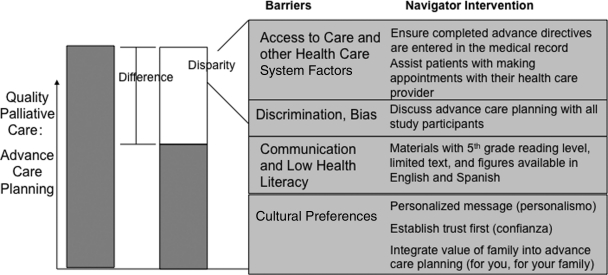
Improving advance care planning communication for Latinos
Based on our study findings, we have developed an intervention to increase knowledge and understanding and rates of completion of ADs.43 The model for this intervention (Fig. 2) addresses cultural factors by utilizing a bicultural and bilingual patient navigator to deliver a personalized message to patients and their families about advance care planning. As a layperson from the community, a patient navigator eliminates the hierarchal power relationship. The navigator will employ teach–teach-back methods to ensure understanding of the information. Our intervention addresses limited health literacy by providing English and Spanish language materials that are targeted for a low literacy population by using simple language, bulleted points, and pictures/cartoons to illustrate information.42
Fig. 2.
Model of patient navigator intervention to improve advance care planning.
Limitations
Our study has several limitations. First, we were approaching patients who were recently hospitalized and experiencing acute medical illness. It is possible that their recollection of AD discussions did not accurately reflect whether or not the discussions had actually occurred. We also relied solely on the medical record for proof of existence of Ads, and the rates we report did not include patients who had completed an AD in another setting (e.g., during estate planning process) that had not been incorporated into the medical record. However, the hospital is the setting where ADs are likely to be necessary and therefore, access to these documents in the medical record is imperative.
Conclusion
We found low rates overall of AD discussions and documentation but an important discrepancy between Latinos and non-Latinos regarding self-report of an AD discussion and documentation of AD in the medical record. The communication breakdown in the Latino population seen in our study raises serious concerns that these conversations are either truly less likely to take place with Latino patients or the health care provider is not effectively communicating. Language barriers do not explain these differences, although inadequate patient provider communication and low health literacy are likely barriers. Finally, culturally competent strategies to increase rates of advance care planning must focus not only on AD completion, but also on ensuring a complete understanding of the entire process.
Acknowledgments
Funding for this study came from the Brookdale Leadership in Aging Fellowship Program and the National Institutes of Aging K23 AG028957-02. The authors also wish to thank Dr. Lilia Cervantes for her assistance with chart reviews and data collection.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Omnibus Budget Reconciliation Act 1990. www.ssa.gov/OP_Home/comp2/F101-508.html. [Jan 29;2011 ]. www.ssa.gov/OP_Home/comp2/F101-508.html
- 2.Dartmouth Atlas Facts on Dying. Policy Relevant Data on Care at the End of Life, USA, State Statistics. www.chcr.brown.edu/dying/usastatistics.htm. [Jan 15;2011 ]. www.chcr.brown.edu/dying/usastatistics.htm
- 3.U.S. Department of Health and Human Services. Advance Directives and Advance Care Planning: Report to Congress. http://aspe.hhs.gov/daltcp/reports/2008/ADCongRpt.pdf. [Jan 29;2011 ]. http://aspe.hhs.gov/daltcp/reports/2008/ADCongRpt.pdf
- 4.AHRQ. Research in Action Issue #12. Advance Care Planning: Preferences for Care at the End of Life. www.ahrq.gov/research/endliferia/endria.htm. [Jan 15;2011 ]. www.ahrq.gov/research/endliferia/endria.htm [PubMed]
- 5.Knauft E. Nielsen EL. Engelberg RA. Patrick DL. Curtis JR. Barriers and facilitators to end-of-life care communication for patients with COPD. Chest. 2005;127:2188–2196. doi: 10.1378/chest.127.6.2188. [DOI] [PubMed] [Google Scholar]
- 6.Teno JM. Advance directives: Time to move on. Ann Intern Med. 2004;141(2):159–160. doi: 10.7326/0003-4819-141-2-200407200-00017. [DOI] [PubMed] [Google Scholar]
- 7.Travis SS. Loving G. McClanahan L. Bernard M. Hospitalization patterns and palliation in the last year of life among residents in long-term care. Gerontologist. 2001;41(2):153–160. doi: 10.1093/geront/41.2.153. [DOI] [PubMed] [Google Scholar]
- 8.Fischer SM. Min SJ. Kutner JS. Advance directive discussions do not lead to death. J Am Geriatr Soc. 2010;58:400–401. doi: 10.1111/j.1532-5415.2009.02698.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silveira MJ. Kim SY. Langa KM. Advance directives and outcomes of surrogate decision making before death. New Engl J Med. 2010;362:1211–1218. doi: 10.1056/NEJMsa0907901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mack JW. Weeks JC. Wright AA. Block SD. Prigerson HG. End-of-life discussions, goal attainment, and distress at the end of life: Predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol. 2010;28:1203–1208. doi: 10.1200/JCO.2009.25.4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith AK. McCarthy EP. Paulk E. Balboni TA. Maciejewski PK. Block SD. Prigerson HG. Racial and ethnic differences in advance care planning among patients with cancer: Impact of terminal illness acknowledgment, religiousness, and treatment preferences. J Clin Oncol. 2008;26:4131–4137. doi: 10.1200/JCO.2007.14.8452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caralis PV. Davis B. Wright K. Marcial E. The influence of ethnicity and race on attitudes toward advance directives, life-prolonging treatments, and euthanasia. J Clin Ethics. 1993;4:155–165. [PubMed] [Google Scholar]
- 13.Hopp FP. Duffy SA. Racial variations in end-of-life care. J Am Geriatr Soc. 2000;48:658–663. doi: 10.1111/j.1532-5415.2000.tb04724.x. [DOI] [PubMed] [Google Scholar]
- 14.Phipps E. True G. Harris D. Chong U. Tester W. Chavin SI. Braitman LE. Approaching the end of life: Attitudes, preferences, and behaviors of African-American and white patients and their family caregivers. J Clin Oncol. 2003;2:549–554. doi: 10.1200/JCO.2003.12.080. [DOI] [PubMed] [Google Scholar]
- 15.Morrison RS. Morrison EW. Glickman DF. Physician reluctance to discuss advance directives. An empiric investigation of potential barriers. Arch Intern Med. 1994;154:2311–2318. [PubMed] [Google Scholar]
- 16.Perkins HS. Geppert CM. Gonzales A. Cortez JD. Hazuda HP. Cross-cultural similarities and differences in attitudes about advance care planning. J Gen Intern Med. 2002;17:48–57. doi: 10.1046/j.1525-1497.2002.01032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gutheil IA. Heyman JC: “They don't want to hear us”: Hispanic elders and adult children speak about end-of-life planning. J Soc Work End-Of-Life Palliat Care. 2006;2:55–70. doi: 10.1300/J457v02n01_05. [DOI] [PubMed] [Google Scholar]
- 18.Phinney JS. The Multigroup Ethnic Identity Measure: A new scale for use with adolescents and young adults from diverse groups. J Adolesc Res. 1992:7156–7176. [Google Scholar]
- 19.Fischer SM. Gozansky W. Sauaia A. Min SJ. Kutner JS. Kramer A. A practical tool to identify patients who may benefit from a palliative approach: The CARING criteria. J Pain Symptom Manage. 2005;31:285–292. doi: 10.1016/j.jpainsymman.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 20.Hosmer DW. Lemeshow S. Applied Logistic Regression. New York: A Wiley-Interscience Publication; 1989. [Google Scholar]
- 21.Teno JM. Licks S. Lynn J. Wenger N. Connors AF., Jr Phillips RS. O'Connor MA. Murphy DP. Fulkerson WJ. Desbiens N. Knaus WA. Do advance directives provide instructions that direct care? SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatment. J Am Geriatr Soc. 1997;45:508–512. doi: 10.1111/j.1532-5415.1997.tb05179.x. [DOI] [PubMed] [Google Scholar]
- 22.Colon M. Lyke J. Comparison of hospice use and demographics among European Americans, African Americans, and Latinos. Am J Hospice Palliat Care. 2003:182–190. doi: 10.1177/104990910302000306. [DOI] [PubMed] [Google Scholar]
- 23.Johnson KS. Kuchibhatala M. Sloane RJ. Tanis D. Galanos AN. Tulsky JA. Ethnic differences in the place of death of elderly hospice enrollees. J Am Geriatr Soc. 2005;53:2209–2215. doi: 10.1111/j.1532-5415.2005.00502.x. [DOI] [PubMed] [Google Scholar]
- 24.Waters CM. Understanding and supporting African Americans' perspectives of end-of-life care planning and decision making. Qualit Health Res. 2001;11:385–398. doi: 10.1177/104973201129119172. [DOI] [PubMed] [Google Scholar]
- 25.Fischer SM. Kutner JS. Sauaia A. Kramer A. Lack of ethnic differences in end-of-life care in the Veterans Health Administration. Am J Hospice Palliat Med. 2007;24:277–283. doi: 10.1177/1049909107302295. [DOI] [PubMed] [Google Scholar]
- 26.Eisert SL. Mehler PS. Gabow PA. Can America's urban safety net systems be a solution to unequal treatment? J Urban Health. 2008;85:766–778. doi: 10.1007/s11524-008-9296-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Ryn M. Burgess D. Malat J. Griffin J. Physicians' perceptions of patients' social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. Am J Public Health. 2006;96:351–357. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40(1 Suppl):I140–I151. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- 29.Schulman KA. Berlin JA. Harless W. Kerner JF. Sistrunk S. Gersh BJ. Dube R. Taleghani CK. Burke JE. Williams S. Eisenberg JM. Escarce JJ. The effect of race and sex on physicians' recommendations for cardiac catheterization. New Engl J Med. 1999;340:618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 30.Sabin JA. Rivara FP. Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;46:678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- 31.Anderson KO. Richman SP. Hurley J. Palos G. Valero V. Mendoza TR. Gning I. Cleeland CS. Cancer pain management among underserved minority outpatients: Perceived needs and barriers to optimal control. Cancer. 2002;94:2295–2304. doi: 10.1002/cncr.10414. [DOI] [PubMed] [Google Scholar]
- 32.Itano JK. Cultural diversity among individuals with cancer. In: Yarbro CH, editor; Wujcik D, editor; Gobel BH, editor. Cancer Nursing Practices and Principles. 7th. Sudbury, MA: Bartlett Learning, LCC; 2010. pp. 71–92. [Google Scholar]
- 33.Krieger N. Smith K. Naishadham D. Hartman C. Barbeau EM. Experiences of discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61:1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 34.Hopwood CJ. Flato CG. Ambwani S. Garland BH. Morey LC. A comparison of Latino and Anglo socially desirable responding. J Clin Psychol. 2009;65:769–780. doi: 10.1002/jclp.20584. [DOI] [PubMed] [Google Scholar]
- 35.Morales LS. Cunningham WE. Brown JA. Liu H. Hays RD. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med. 1999;14:409–417. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.The Health Literacy of America's Adults. Results from the 2003 National Assessment of Adult Literacy. http://nces.ed.gov/pubs2006/2006483.pdf. [Jan 20;2011 ]. http://nces.ed.gov/pubs2006/2006483.pdf
- 37.Wilson E. Chen AH. Grumbach K. Wang F. Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20:800–806. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Health Communication. http://www.healthypeople.gov/document/HTML/Volume1/11HealthCom.htm. [Jan 20;2011 ]. http://www.healthypeople.gov/document/HTML/Volume1/11HealthCom.htm
- 39.National Center for Education Statistics. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy (NCES 2006-483) http://nces.ed.gov/pubs2006/2006483.pdf. [Jan 20;2011 ]. http://nces.ed.gov/pubs2006/2006483.pdf
- 40.Volandes AE. Paasche-Orlow M. Gillick MR. Cook EF. Shaykevich S. Abbo ED. Lehmann L. Health literacy not race predicts end-of-life care preferences. J Palliat Med. 2008;11:754–762. doi: 10.1089/jpm.2007.0224. [DOI] [PubMed] [Google Scholar]
- 41.Volandes AE. Ariza M. Abbo ED. Paasche-Orlow M. Overcoming educational barriers for advance care planning in Latinos with video images. J Palliat Med. 2008;11:700–706. doi: 10.1089/jpm.2007.0172. [DOI] [PubMed] [Google Scholar]
- 42.Sudore RL. Landefeld CS. Barnes DE. Lindquist K. Williams BA. Brody R. Schillinger D. An advance directive redesigned to meet the literacy level of most adults: a randomized trial. Patient Educ Counseling. 2007;69:165–195. doi: 10.1016/j.pec.2007.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fischer SM. Sauaia A. Kutner JS. Patient navigation: A culturally competent strategy to address disparities in palliative care. J Palliat Med. 2007:1023–1028. doi: 10.1089/jpm.2007.0070. [DOI] [PubMed] [Google Scholar]
- 44.Aging with Dignity. www.agingwithdignity.org/five-wishes.php. [Aug 16;2011 ]. www.agingwithdignity.org/five-wishes.php