Abstract
To describe endoscopic power assisted adenoidectomy and review the experience with the procedure demonstrating its safety and efficacy. Prospective study of 44 patients aged between 7 to 15 years undergoing power assisted adenoidectomy between Jan 2004 and July 2006. Tertiary care private teaching hospital. Forty four consecutive children with adenoid hypertrophy undergoing power assisted adenoidectomy. Therapeutic endoscopic adenoidectomy using microdebrider. Operative time, blood loss, complications, completeness and depth of removal, surgeon’s satisfaction and recovery period. The average operative time was 12 min (range: 8–16 min) and average blood loss was 30 ml (range: 24–42 ml). Complete resection was possible under vision with few complications. The surgeon satisfaction was high and post-operative recovery good. Power assisted adenoidectomy is quick, precise and safe. There is good visualization during resection thus improving precision and ensuring complete removal of adenoid tissue.
Keywords: Adenoidectomy, Endoscopic, Microdebrider, Power-assisted
Introduction
Adenoid, a nasopharyngeal lymphoid tissue forming a part of the Waldeyer ring, was initially described in 1868 by Meyer [1]. Adenoidectomy is one of the most common procedures performed in children today, either alone or in conjunction with tonsillectomy or insertion of ventilating tubes. The widely used conventional curette adenoidectomy was first described in 1885 [1]. Complications such as bleeding, inadequate removal, eustachian tube stenosis and nasopharyngeal stenosis though uncommon are best prevented by precise resection of adenoid tissue with preservation of integrity of nasopharyngeal structures. Dissatisfaction with conventional technique in, adequately and safely removing the adenoid tissue has, led to the development of alternative methods, including endoscope guided power-shaver adenoidectomy [2]. These have been made possible by developments in fiber optics and endoscopic instrumentation [3, 4]. We have in our study described the use of microdebrider for adenoidectomy guided by the rigid nasal endoscope highlighting its advantages and disadvantages.
Materials and Methods
Prospective study of 44 children who underwent endoscopic power assisted adenoidectomy from January 2004 to July 2006 was conducted. The children were aged between 7 to 15 years (median age: 9 years), 27 being males (61.36%) and 17 females (38.64%). These patients had symptoms of nasal obstruction, mouth breathing, snoring, deafness and recurrent sinusitis. Twenty eight patients (63.64%) had undergone tonsillectomy in past. Adenoid hypertrophy was confirmed by radiograph of nasopharynx and nasal endoscopy with 0° sinuscope. The procedure of complete endoscopic power assisted adenoidectomy was performed by the senior author in a tertiary care teaching hospital.
Technique
Patients were given general anaesthesia with orotracheal intubation. The theatre set up and positioning was as for a standard functional endoscopic sinus surgery. The nasal cavities were decongested by using pledgets soaked in 4% lignocaine with 1:10,000 adrenaline. Mouth gag was applied. Using a 0° 2.7 mm rigid telescope (4 mm for older children), the posterior choanae and nasopharynx were assessed. Microdebrider with irrigating blades of different angles 0, 15, 45 and 60° or special adenoid blade was used (Fig. 1). The special adenoid blade is longer, and has a window on convex side for use transorally to adapt to the roof of nasopharynx. Sinuscope and debrider were passed through the same nostril or, the sinuscope through one nostril and debrider through the other (Fig. 2). In some cases sinuscope was passed through nose and debrider through the oral cavity with angled blade (Fig. 3). In smaller children transoral approach was performed with 45° scope and angled microdebrider blades or adenoid blades (Fig. 4). Under endoscopic vision the shaver cannula was passed into nose with suction switched off to avoid trauma to turbinates or the septum. The suction was then turned on which draws the adenoid tissue in and the rotating blade shaves it under constant endoscopic vision. The adenoidectomy was started high in the nasopharynx from upper limit of adenoid tissue, which often cannot be reached by conventional curette. Resection was continued in side to side fashion on an even level until the inferior edge of adenoid pad was reached. The cutting and aspirating action of the shaver and simultaneous irrigation removes both adenoid tissue and the blood, thus providing a clear view. Better control of the depth of removal of adenoid is achieved thus avoiding damage to underlying structures. Haemostasis was obtained by applying pledgets soaked in hydrogen peroxide or by suction diathermy in few cases. A nasopharyngeal pack was kept for few minutes and then removed. Mouth gag was removed. Post operative care was given and patient discharged the same day. All patients were followed up after a week and then monthly over 6 months to 1 year. At follow up, endoscopic nasopharyngeal examination was done to assess healing and completeness of removal.
Fig. 1.
Microdebrider with irrigating blades of different angles and the special adenoid blade. Inset shows tip of adenoid blade with window on convex side
Fig. 2.
Transnasal approach with 0° sinuscope and 15° debrider blade
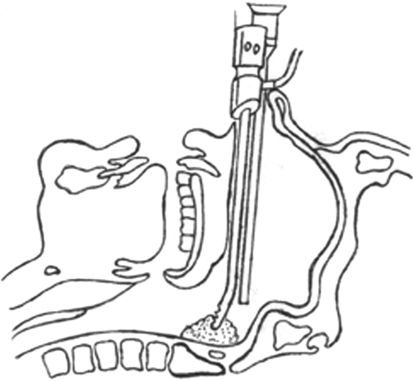
Fig. 3.
0° Sinuscope through nose and debrider with adenoid blade transorally
Fig. 4.
Transoral approach with 45° angled sinuscope and adenoid blade
Intra operative parameters recorded were adenoid size, operative time, blood loss, completeness and depth of removal, surgeon satisfaction and complications. Adenoid size was recorded based on degree of nasopharyngeal obstruction noted on nasal endoscopy, as small to moderate (<50% obstruction), large (50–75% obstruction) or very large (>75% obstruction). Operative time in minutes and seconds was recorded on a stop watch, beginning from fixing of the mouth gag till when the mouth gag was removed.
Precise blood loss was calculated from the difference in amount of irrigating fluid used and the collected fluid in the vacuum flask. During adenoidectomy, in-line irrigation system of the microdebrider was used. So the exact amount of irrigating fluid from saline bottle was noted. At end of procedure the material collected from suction canister was filtered to remove tissue and the remaining fluid comprising of blood and sucked irrigating fluid measured. The blood loss in milliliters was calculated as the difference between this amount and the earlier amount of saline used for irrigation. The blood soiling the nasopharyngeal pack after surgery was not measured. The completeness of the adenoid resection was recorded as fair, good or excellent. It was noted as excellent when adenoid tissue was completely resected superiorly up to roof of nasopharynx, posterolaterally till the eustachian tube orifices and anteriorly from the choanae. Resection was rated as good when only a few adenoid tags were left behind inadvertently and fair when substantial adenoid remnants were found post operatively. The depth of resection was recorded as shallow, adequate or excessive depending on the plane of tissue dissection reached. Intra operative complications such as injury to surrounding structures could be assessed in the theatre itself. The surgeon performing the procedure noted his level of satisfaction.
On follow up after a week the patients were assessed for pain, neck stiffness, speech changes and swallowing problems. Endoscopic nasopharyngeal examination was done and the adequacy of adenoid removal assessed. Patient’s recovery in terms of time required to return to his normal diet and activities was noted. Ten patients were lost to follow-up at end of 1 year. Thirty four patients were further examined endoscopically at end of 1 year to rule out nasopharyngeal stenosis. Data was compiled and analyzed.
Results
Patient demographics, indications for adenoidectomy and sizes of adenoid are listed in Table 1. Nasal obstruction in 35 patients (79.55%) and breathing by mouth in 34 patients (77.27%) were the most common indications for the surgery. Other indications were snoring (31.82%), otitis media (27.27%) and recurrent sinusitis (20.45%). Every patient had one or more of these complaints. Most of our patients had moderate to large sized adenoids as assessed by sinuscope.
Table 1.
Patient demographics, indications for adenoidectomy and sizes of adenoid in 44 patients (n = 44)
| Age | Range: 7–15 years; median: 9 years |
| Male | 27 (61.36%) |
| Female | 17 (38.64%) |
| Indication for adenoidectomy | |
| Nasal obstruction | 35 (79.55%) |
| Mouth breathing | 34 (77.27%) |
| Snoring | 14 (31.82%) |
| Otitis media | 12 (27.27%) |
| Recurrent sinusitis | 9 (20.45%) |
| Size of adenoids | |
| Small to moderate (<50% obstruction) | 6 (13.64%) |
| Large (50–75% obstruction) | 26 (59.09%) |
| Very large (>75% obstruction) | 12 (27.27%) |
Results are shown in Table 2. The mean operative time was 12 min 30 s (range, 8–16 min). The average blood loss was 30 ml (range, 24–42 ml). Completeness of resection was excellent in all cases and depth of removal, adequate. There were no intraoperative complications in any of the patients. Amongst the initial patients in our series three (6.82%), complained of post operative neck pain and stiffness which was relieved with analgesics. Six patients (13.64%) had transient hypernasality lasting for a week. All patients were on normal diet within 3 days after surgery and returned to normal activities within a week. Complete airway patency and no remnant of adenoids were seen in all patients assessed by endoscopic evaluation at follow up. At 1 year follow up, endoscopic examination showed no Eustachian tube stenosis or nasopharyngeal stenosis in any of the 34 patients. Others were lost to follow up. Surgeon satisfaction with the microdebrider was high and has continued to perform power assisted adenoidectomy.
Table 2.
Result of main outcome measures in 44 patients who underwent endoscopic power assisted adenoidectomy
| Parameter | Result |
|---|---|
| Operative time | 12 min 30 s (range, 8–16 min) |
| Blood loss | 30 ml (range, 24–42 ml) |
| Completeness of resection | Excellent |
| Depth of removal | Adequate |
| Intra-operative complications | Nil |
| Post-operative complications | Neck pain (6.82%) |
| Hypernasality (13.64%) | |
| Surgeon satisfaction | High |
Discussion
Adenoidectomy is one of the most frequently performed operations in children. Though not considered a risky surgery, some complications do occur, the most important being bleeding (0.5–8% incidence) [5]. The surgical technique used can have considerable influence on the intra operative bleeding, post operative pain and the recovery time. This is important in day care surgeries like adenoidectomy. Also complications like nasopharyngeal stenosis and eustachian tube stenosis though rare are difficult to handle if they occur [6].
Traditionally adenoidectomy is done with a curette. The main disadvantage of this method is that it is relatively a blind technique that may lacerate the choanae and torus tubaris, the nasopharyngeal mucosa or may leave behind obstructing tissue, particularly at the eustachian tube orifices, high in the nasopharynx and at intranasal protrusions [7].
In an attempt to overcome the short comings of curettage method various techniques of adenoidectomy have been devised. Suction diathermy ablation of adenoid has been a popular alternative, reported to be is safe with minimal blood loss [8, 9], however it may not address intranasal adenoid tissue, is slow and has the risk of cicatrisation and burns to surrounding tissue as does the use of CO2 laser which in addition requires its special precautions [10]. Nasopharyngeal stenosis has been reported following adenoidectomy using a KTP laser [11]. Other methods described are radiofrequency adenoidectomy [12] and use of electronic molecular resonance tool [5].
Power assisted adenoidectomy using a microdebrider is a recently described procedure. We prospectively studied patients in whom we performed endoscopic guided power assisted adenoidectomy and reviewed its merits and demerits.
The microdebrider has been used extensively for tissue debridement during endoscopic sinus surgery, where precision is required to avoid orbital or intracranial entry [13]. Adenoidectomy with microdebrider using a transnasal endoscopic approach has been described [4, 10]. Others have used a mirror for visualization in the place of endoscope [6, 14].
One retrospective review of complete adenoidectomy using microdebrider versus curettes showed that power-assisted adenoidectomy was 58% faster (11 min vs. 19 min) but the blood loss (22 ml vs. 32 ml), recovery time and complications were not significantly different [7]. A subsequent prospective randomized study showed again that operative time was much less with microdebrider (10 min 13 s vs. 12 min 14 s) and also that blood loss was less with microdebrider (17.5 ml vs. 24.0 ml, 27% less) [14].
In our study, which was a non-comparative prospective one, we found the operative time with endoscopic power assisted technique was 12 min 30 s and blood loss was 30 ml. Blood loss was lesser in cases where diathermy was used. The surgeon found that the oscillating cutting action of the shaver blade minimizes bleeding and continuous suction maintains a clear view thus enhancing safety. Due to the suction and shaving action of the microdebrider drawing the loose tissue into the window, it can remove the tissue down to a less vascular fascial plane, as opposed to the pushing and cutting action of the curette which may leave bleeding tissue behind. Irrigation while using the microdebrider also aids in quicker haemostasis.
In comparative studies of partial adenoidectomy by the two methods, the results have been similar. Partial adenoidectomy is done leaving behind lower part of adenoid tissue to avoid velopharyngeal insufficiency [6]. This requires greater control of tissue removal and the microdebrider meets the demands for precision. The adenoid curettes do not have the control needed to provide a limited resection with certainty [14].
Stanislaw et al. [14] found that the tissue dissection was more complete and to the appropriate depth with a microdebrider, as opposed to being too shallow or too deep with a curette. The surgeon satisfaction was also greater. A prospective study involving endoscopic evaluation of cases operated by curette and microdebrider has shown that, following traditional curette adenoidectomy 39% of patients had residual obstructive tissue which was completely cleared by powered shaver adenoidectomy later [10].
Our experience with the microdebrider was supported by these studies, with respect to completeness of adenoid tissue removal to adequate depth and causing no damage to surrounding structures. The surgeon satisfaction, though a subjective parameter, was definitely high. The post operative recovery was satisfactory though a small percentage (6.82%) of patients did complain of neck pain which was relieved by analgesics. These were the first few patients and the author attributes it to deeper resection in initial surgeries. This complaint was not seen in later surgeries. Some patients (13.64%) had transient hypernasality which lasted for 1 week. None of the patients who came for long term follow-up showed any symptoms or signs of Eustachian tube stenosis.
The use of rigid endoscope or sinuscope has its advantages. It allows good visualization ensuring complete removal of adenoid tissue situated even high up in nasopharynx and intranasally without damaging surrounding structures. When used transnasally there is no need to extend the neck especially in patients with instability of cervical spine [10]. The camera attachment allows for better magnified view on the monitor, facilitating recording as well as trainee teaching. The technique of endoscopic adenoidectomy has been described using rigid telescope for visualization and forceps for removal of adenoids [15].
Performing an endoscopic power assisted adenoidectomy, harvests the advantages of both the telescope as well as the microdebrider.
Use of microdebrider has a few disadvantages. It requires the use of expensive equipment including the cost of blades which require replacement. Some authors have noted the difficulty in maneuvering the microdebrider tip into the nasopharynx, especially with a telescope in same side of the nose [4]. This can be overcome by placing the two instruments in different nostrils or transorally. Koltai et al. [7] in their series bent the shaver blade as per requirement of the nasopharynx. A special adenoid blade with the window with cutting blade on its convex aspect is available to serve the purpose which we used transorally in our study. Another shortcoming is that the resected tissue is not available for histopathological examination. Moreover we found that our technique requires a good training to achieve proficiency.
Key Messages
Endoscopic power assisted adenoidectomy is a safe, precise and quick procedure with minimal blood loss. It gives a complete clearance of obstructive adenoids under vision thus providing reliable restoration of nasopharyngeal patency. In addition to providing a good magnified view the sinuscope with camera aids in recording and teaching. Controlled tissue resection by microdebrider results in minimizing complications.
References
- 1.Thornval A. Wilhelm Meyer and the adenoids. Arch Otolaryngol Head Neck Surg. 1969;90:383. doi: 10.1001/archotol.1969.00770030385023. [DOI] [PubMed] [Google Scholar]
- 2.Parsons DS. Rhinologic uses of powered instrumentation in children beyond sinus surgery. Otolaryngol Clin N Am. 1996;29:105–114. [PubMed] [Google Scholar]
- 3.Huang HM, Chao MC, Chen YL, Hsiao HR. A combined method of conventional and endoscopic adenoidectomy. Laryngoscope. 1998;108:1104–1106. doi: 10.1097/00005537-199807000-00028. [DOI] [PubMed] [Google Scholar]
- 4.Yanagisawa E, Weaver EM. Endoscopic adenoidectomy with the microdebrider. Ear Nose Throat J. 1997;76:72–74. [PubMed] [Google Scholar]
- 5.Tarantino V, D’Agostino R, Melagrana A, Porcu A, Stura M, Vallarino R. Safety of electronic molecular resonance adenoidectomy. Int J Pediatr Otolaryngol. 2004;68(12):1519–1523. doi: 10.1016/j.ijporl.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 6.Murray N, Fitzpatrick P, Guarisco JL. Powered partial adenoidectomy. Arch Otolaryngol Head Neck Surg. 2002;128(7):792–796. doi: 10.1001/archotol.128.7.792. [DOI] [PubMed] [Google Scholar]
- 7.Koltai PJ, Kalathia AS, Stanislaw P, Heras HA. Power-assisted adenoidectomy. Arch Otolaryngol Head Neck Surg. 1997;123:685–688. doi: 10.1001/archotol.1997.01900070023004. [DOI] [PubMed] [Google Scholar]
- 8.Owens D, Jaramillo M, Saunders M. Suction diathermy adenoid ablation. J Laryngol Otol. 2005;119(1):34–35. doi: 10.1258/0022215053222743. [DOI] [PubMed] [Google Scholar]
- 9.Wong L, Moxham JP, Ludemann JP. Electrosurgical adenoid ablation. J Otolaryngol. 2004;33(2):104–106. doi: 10.2310/7070.2004.00104. [DOI] [PubMed] [Google Scholar]
- 10.Havas T, Lowinger D. Obstructive adenoid tissue: an indication for powered-shaver adenoidectomy. Arch Otolaryngol Head Neck Surg. 2002;128(7):789–791. doi: 10.1001/archotol.128.7.789. [DOI] [PubMed] [Google Scholar]
- 11.Giannoni C, Sulek M, Friedman EM, Duncan NO. Acquired nasopharyngeal stenosis: a warning and review. Arch Otolaryngol Head Neck Surg. 1998;124:163–167. doi: 10.1001/archotol.124.2.163. [DOI] [PubMed] [Google Scholar]
- 12.Shehata EM, Ragab SM, Behiry AB, Erfan FH, Gamea AM. Telescopic-assisted radiofrequency adenoidectomy: a prospective randomized controlled trial. Laryngoscope. 2005;115(1):162–166. doi: 10.1097/01.mlg.0000150704.13204.20. [DOI] [PubMed] [Google Scholar]
- 13.Setliff RC., III The hummer: a remedy for apprehension in functional endoscopic sinus surgery. Otolaryngol Clin N Am. 1996;29:95–104. [PubMed] [Google Scholar]
- 14.Stanislaw P, Koltai PJ, Feustel PJ. Comparison of power-assisted adenoidectomy vs adenoid curette adenoidectomy. Arch Otolaryngol Head Neck Surg. 2000;126(7):845–849. doi: 10.1001/archotol.126.7.845. [DOI] [PubMed] [Google Scholar]
- 15.Cannon CR, Replogle WH, Schenk MP. Endoscopic assisted adenoidectomy. Otolaryngol Head Neck Surg. 1999;121(6):740–744. doi: 10.1053/hn.1999.v121.a98201. [DOI] [PubMed] [Google Scholar]