Abstract
Objective:
To compare the psychopathology between depressed patients with low religiosity and those with high religiosity and to correlate the level of religiosity with the psychopathology in the psychiatric clinic of a general hospital in Chandigarh, North India.
Materials and Methods:
Thirty depressed patients with low religiosity and 30 patients with high religiosity were assessed on the Religiosity Scale, Beck Depression Inventory, Hamilton Depression Rating Scale, Beck Hopelessness Scale and Suicidal Intent Questionnaire.
Results:
In the patients with depression, hopelessness and suicidal intent correlated negatively with the level of religiosity.
Conclusion:
In depressed patients, hopelessness and suicidal intent are inversely related to the level of religiosity.
Keywords: Depression, hopelessness, religiosity, suicidal intent
INTRODUCTION
Major depressive disorder is reported to be the most common mood disorder.[1] The psychopathology of depression is characterized by mood disturbances, anhedonia and loss of interest, psychomotor retardation and depressive cognitions. The depressive cognitions include negative evaluations of the self, of the world and of the future along with recurrent thoughts of death and suicide. Depression also has vegetative symptoms in the form of anorexia, sleep disturbances and decreased libido. Similar rates of depression across cultures may obscure the diversity of the experience of depression in different cultures and in different patients.[2] So, it is important to elucidate not only biological or cognitive understandings of depression but also its social and cultural contexts.
A satisfactory definition of religion has eluded scholars to this day. Capps[3] argued that the definitions of religion offered by many eminent scholars reflected the personal biographies of those scholars, and Yinger[4] said that any theoretical definition of religion was likely to be satisfactory only to its author. According to Shafranske and Maloney,[5] the term “religion” refers to “adherence to and beliefs and practices of an organised church or religious institution”. Any research on religious experience and behavior requires an operational definition of denomination and frequency of religious observance. A person can be religious to varying degrees and so these constructs are typically quantitative. Religion can thus be viewed in a one-dimensional or multidimensional perspective. Glock and Stark[6] suggested that religion has five dimensions, and Koenig in his book “Handbook of religion and mental health” has given a list of 12 dimensions of religiousness out of which a particular set may require measurement for a particular study.[7]
Earlier surveys had reported that as compared to 90% of the general public, only 40–70% of psychiatrists and psychologists professed a belief in God.[8] Several years ago, Kroll and Sheehan[9] and Larson et al.[10] had also noted that religious and spiritual variables were relatively neglected in the study of mental health. In recent times, however, a number of authors have underscored the importance of mental health professionals, taking into account the religious and spiritual lives during the psychiatry consultation.[11–13] Studies have found religiosity to affect the occurrence and psychopathology of substance abuse, psychosis, obsessive compulsive disorder and other anxiety disorder.[14–17] A study by Kendler et al.[18] identified dimensions of religiosity and correlated them with externalizing and internalizing psychiatric disorders. It was seen that the dimensions of general religiosity, forgiveness, God as judge and involved God were associated with lesser prevalence of externalizing disorders including nicotine, alcohol and other substance dependence and adult anti-social behavior. Social religiosity and thankfulness were associated with lower prevalence of externalizing as well as internalizing disorders (major depression, phobias, panic disorder, generalized anxiety disorder and bulimia nervosa). The various aspects of depression that have been studied to see if they are affected by religion are its incidence, severity, type of psychopathology, speed of remission, use of religious coping and the use of religious psychotherapies.[19,20] Both religious affiliation and religious practices have been shown to affect the incidence of depression.[21–24] Religious parameters also affect the incidence of depression in the medically ill population as shown in women who had suffered hip fractures and in a group of functionally impaired elderly adults.[25,26] Studies have also shown that more religious depressed persons have lesser depressive cognitions but the same level of somatic symptoms.[27,28] Suicidal attempts in depressed in-patients were seen to be higher in religiously unaffiliated subjects and greater moral objection to suicide was one of the protective factors against suicide.[29] Bainbridge and Stark reported a strong negative correlation between church membership and suicide rates for 78 large metropolitan areas in the United States.[30] Longitudinal studies have also shown that higher religiosity was also associated with faster remission of depression.[31,32]
Previous studies have examined religion as a coping mechanism in physical and mental illnesses but few studies have investigated the relationship between the patient's religiosity and depressive psychopathology. If many patients cognitively and emotionally deal with mental and physical illness by relying on religious faith, then mental health professionals need to be aware of the effects of religion on mental illness. Hence, we conducted a study with the objectives of comparing the depressive psychopathology between depressed patients with low religiosity and high religiosity and of correlating the level of religiosity with depressive psychopathology.
MATERIALS AND METHODS
The study design was cross-sectional and all assessments were completed in a single session. Patients with first onset, non-psychotic depressive episode were recruited from the out-patient service of the Department of Psychiatry at Post-Graduate Institute of Medical Education and Research (PGIMER) in Chandigarh, North India. Chandigarh is the capital of the states of Punjab and Haryana in North India. The institute serves as the major health care center for patients from urban as well as rural areas of four surrounding states. The sampling was conducted in a purposive manner. The sample consisted of 30 patients with high religiosity and 30 patients with low religiosity.
Inclusion and exclusion criteria
Patients of either gender, between 20 and 45 years of age, belonging to any religion, with a mild, moderate or severe depressive episode without psychotic symptoms as diagnosed using the ICD-10 criteria for research, i.e. DCR-10,[33] were included in the study. Patients who had psychiatric co-morbidity in the form of substance abuse disorders, psychotic disorders, anxiety disorders or mental retardation, chronic physical illness and subjects who did not consent to take part in the study were excluded.
Instruments
Sociodemographic profile sheet
The sociodemographic profile sheet developed at the Department of Psychiatry, PGIMER, Chandigarh, India, was administered to record demographic variables including the age, sex, marital status, education, religion, occupation and type of family.
Clinical profile sheet
This contains information regarding the age of onset of illness, total duration of illness, family history of psychiatric disorder and details of treatment taken.
Beck depression inventory
It is a 21-item scale on which the individuals are asked to rate each item on a 0–3 spectrum with a total score range of 0–63. The items assess the various symptoms of depression including sadness, anhedonia, depressive cognitions of guilt, punishment and suicide and various somatic symptoms. It has been found to be psychometrically sound for both depressed and normal adults.[34]
Religiosity scale
The Religiosity Scale designed in India by Deka and Broota[35] consists of 44 items which measure the level of religious faith and belief in the local language. For example, the first item is “heaven and hell do not exist, these are only imaginations of the mind” and the second item is “A good person is only one who has full faith in God”. For each item, the subject has to specify if he or she strongly agrees, agrees, does not know, disagrees or strongly disagrees with statement. Each response is accordingly scored from 1 to 5. The final scale consists of 44 items out of which 25 are positive and 19 negative. The total score ranges from 44 to 220. The division of subjects into those with high religiosity and those with low religiosity is done on the basis of a central score of 140. An advantage with the scale is that its items are not specific to any religion and hence can be used for all religious groups. The reliability and validity of the final scale has been established. The reliability co-efficient of 0.96 indicated that the scale has a high reliability. The scale has been cross-validated on a sample of college students belonging to four different religious groups: Muslims, Christians, Jains and Hindus.[36]
Hamilton depression rating scale
It is an observer rated scale having 21 items. Each item (except 2 two-part items) is rated on a 0–4 spectrum. The total score ranges from 0 to 84. It has items on all symptoms of depression including the rarer symptoms of paranoid ideation, depersonalization and derealization and obsessions. It evaluates somatic symptoms including difficulties with sleep and appetite, weight loss, psychic and somatic anxiety in greater detail than the BDI. It has good validation, research base and ease of administration and is widely used in research studies on depression. The inter-rater reliability is 0.87–0.95.[37]
Beck's hopelessness scale
It has 20 true/false items that endorse or deny pessimistic or optimistic statements. Each item has a score of 0 or 1 depending upon the response of the patient. The total score ranges from 0 to 20. The higher the score, the greater is the hopelessness. It demonstrates high internal consistency, with KR-20 coefficient generally of 0.9 or more, test–retest reliability of 0.6 and concurrent validity with clinician's rating of hopelessness of 0.7.[38]
Suicidal intent questionnaire
It consists of 10 questions in the local language relating only to suicidal ideation. Each of the questions has three responses–often, sometimes and never. Each of these responses is scored as 0, 1 or 2. Thus, the subject's total score may range from 0 to 20. Based on the score, the subject is grouped under one of three categories–non-communicators (suicidal intent absent), partial communicators and definite communicators (suicidal preoccupation definitely present). The clinical validity of the scale has been assessed in 40 indoor patients and was found to be high.[39]
Procedure
All outpatients fulfilling the selection criteria were approached, explained the purpose of the study, and written informed consent was obtained from them. Clinical and sociodemographic details were obtained from the patients, relatives and treatment records. ICD-10 DCR criteria were used to confirm and record the diagnosis at the time of inclusion into the study. Following this, the instruments BDI, Religiosity scale, BHS, SIQ and HDRS were applied. A total of 69 patients were approached. Out of these, three refused to take part in the study and four left the assessment incomplete. Based on the score on the religiosity scale, each patient was grouped as having high or low religiosity. The sample size of 30 patients for high religiosity was completed after assessing 51 patients, and thereafter, the complete assessment was done only when a patient had a score of below 140 (the cut-off) on the religiosity scale.
All statistical tests were done using SPSS version 11.0. Descriptive statistics were used for the demographic and clinical profile of the sample. Chi-square test and one way analysis of variance (ANOVA) were used to test for differences in sociodemographic and clinical profiles between groups. Student's “t” test was used to test for differences in ratings on the scales between the groups with high and low religiosity. Mann–Whitney “U” test was used for one variable (suicidal intent) whose distribution was non-normal. For correlations between religiosity and psychopathology, Pearson's correlation was used for the variables with normal distribution and Spearman's rho was used for the variables with non-normal distribution.
RESULTS
Sociodemographic profile
The average age of the high religiosity group was 34.43 years (SD=8.48). The gender distribution was equal. Most of the subjects of this group were at least matriculate with only eight subjects with an educational level of middle school or below. Paradoxically, a larger proportion, i.e. 17 subjects, was unemployed. Twenty-three of these subjects were married and staying with their spouses and seven were single or separated. A large majority had low income (less than ‘2500). Twenty-two of them belonged to the Hindu religion, with eight patients belonging to Sikhism (six patients) or Islam (two patients). 66% belonged to nuclear families and 80% came from an urban background. 40% of this group came from Chandigarh.
In the low religiosity group, the average age was 31.53 years which was lower than the high religiosity group. This group had a slightly larger proportion (60%) of males. 40% of this group were educated up to the graduate level or higher, 43.67% were matriculates or held diplomas, whereas 16.33% had education below the middle school level. As with the high religiosity group, this group too had more number of married subjects, i.e. 20. Twelve subjects had a low income (less than ‘2500) and there were nine each in the middle and higher income groups. Majority of these subjects belonged to joint or extended type of families. Twenty-two of these patients were either Sikhs or Muslims and eight were Hindus. More than half of the patients belonged to an urban background and there were more patients from Haryana and Punjab as compared to Chandigarh.
Clinical profile of the sample
It was seen that more than 50% of the patients in both the groups had a depressive episode of moderate severity with somatic syndrome as diagnosed by the ICD-10 DCR. The two groups differed significantly in the duration of depressive episode with which they had presented. In the patients with low religiosity, 11 patients presented with an illness duration of 1–2 years, 15 patients with a duration of 6–12 months and 4 patients with a duration of 2 weeks to 5 months. In patients with high religiosity, 14 patients had an illness duration of 1–2 years, 6 patients had a duration of 6–12 months and 10 patients had a duration of 2 weeks to 5 months. Thus, almost 50% of the patients with low religiosity had a depressive episode that had lasted between 6 and 12 months, whereas among the patients with high religiosity, the duration was anywhere between 1 and 2 years in almost 50%. More than 80% patients in both the groups did not have a family history of any psychiatric disorder. The pharmacological treatment most commonly used was selective serotonin reuptake inhibitors with 20 patients of high and 21 patients of the low religiosity group having a prescription of these drugs. The other drugs used were imipramine, venlafaxine, mirtazapine and reboxetine.
Comparison between depressive psychopathology in depressed patients with high religiosity and low religiosity
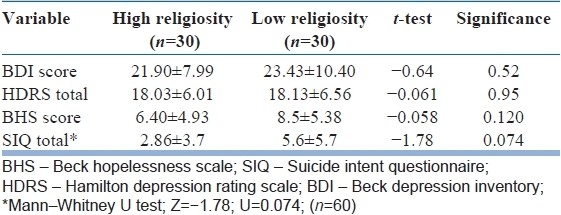
Table 1 shows the various measures of psychopathology and their comparison in groups with high religiosity and with low religiosity. The average BDI score in the low religiosity group was 23.43 (SD=10.4) and in the high religiosity group it was 21.9 (SD=7.99). The average total score on the HDRS in the low religiosity group was 18.13 (SD=6.56) and in the high religiosity group it was 18.03 (SD=6.01). The severity of depression on both the scales did not differ significantly between the two groups. On the BHS, high religiosity patients had a total score of 6.40 (SD=4.93) and low religiosity patients had a score of 8.5 (SD=5.38). The difference was not statistically significant. Suicidal intent was higher in patients with low religiosity (high religiosity group=2.86±3.7; low religiosity group=5.6±5.7), but the difference did not reach statistical significance (Mann–Whitney U test).
Table 1.
Comparison between depressive psychopathology in depressed patients with high religiosity and those with low religiosity
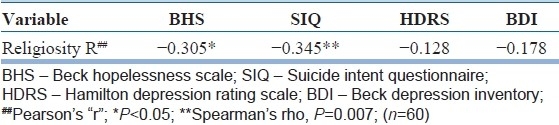
Correlation between religiosity and BHS and SIQ scores
We correlated the religiosity with the measures of psychopathology including total BDI, HDRS, BHS and SIQ scores in all 60 depressed patients. Table 2 shows the correlation between the religiosity score and the scores on the BHS, SIQ, HDRS and BDI. There was a significant negative correlation between the levels of religiosity and the total score on the BHS (r=–0.305; P<0.05). There was a highly significant negative correlation between the levels of religiosity and the total score on the SIQ (rho=–0.345; P=0.007).
Table 2.
Correlation between religiosity and BHS, SIQ, HDRS and BDI scores
DISCUSSION
The current study included 30 patients with low religiosity and 30 patients with low religiosity and examined the depressive symptoms that they manifested. As a part of the selection criteria, patients with psychotic depression or recurrent depressive disorder were excluded. Diagnosis was made using standard ICD-10 diagnostic criteria for research. Assessment of severity of depression was done using two standard scales, one being patient rated and the other being clinician rated. Depressive cognitions were assessed using standard scales, i.e. the BHS and SIQ, the second having been standardized in the Indian population. Religiosity was measured using a scale that has been standardized in Indians and was not specific for persons of any particular religious affiliation. The religiosity scale we used mainly measured one dimension of religiosity, namely, religious beliefs.
Both the groups consisted of an approximately equal number of male and female patients. The entire group consisted of men and women in their mid-thirties, which is known to be the age group in which depression occurs most commonly. Most patients were well-educated but unemployed and with no income. This could be accounted for by the large proportion of educated albeit unemployed housewives in the sample. The subjects were mainly Hindus and Sikhs as is majority of the population in the service area of the hospital. A major part of the sample came from nuclear families of urban background which is typical of the population attending the psychiatric out-patient facility at this hospital.[40]
Most patients had a clinical diagnosis of moderate depression with somatic syndrome and there were no patients without a diagnosis of the somatic syndrome as a qualifier of the depressive episode. Most patients with high religiosity presented with an illness that was at least a year long, whereas those with low religiosity presented with a shorter duration of illness. This could be because patients of depression with high religiosity have lower severity of depression and suicidal intent which may cause a delay in approaching a psychiatric facility. Further, patients with high religiosity could be utilizing religion as a mechanism for coping with their depressive symptoms which may again cause a delay in approaching a psychiatric facility. In medical settings, cross-sectional research has shown that religious coping as measured by an index of religious coping (RCI) correlated inversely with both self-rated and clinician-rated measures of depression.[41,42] Majority of patients had been prescribed selective serotonin reuptake inhibitors.
Several studies have demonstrated that more religious persons have a lower incidence and prevalence of depression. The studies which have correlated the incidence and prevalence of depression to the various dimensions of religiosity are mainly large-scale community-based studies. In a study among medically ill men, it was seen that after controlling for demographics, medical status and religious coping, men who indicated that they had no religious affiliation had higher scores on the HDRS.[41] Multi-item measures of religious involvement are consistently negatively correlated with measures of depressive symptoms and affect,[43–45,25] but the association weakens after controlling for demography, religious salience and comfort from religion.[45,46] Persons who believe in God showed fewer depressive symptoms as per one study[46] but some studies showed no association between the two.[47,48] Compared to the large number of studies on the association between incidence and prevalence of depression or depressive symptoms and religiosity, studies evaluating the relationship between religiosity and psychopathology in patients who are already depressed are very few. It is especially important to identify the effect of religiosity on suicidal intent and hopelessness in depressed patients both in psychiatric and general medical settings. Hence, we compared psychopathology in depressed patients with different levels of religiosity in a psychiatric clinic-based study.
We found that there was no significant difference between the high and low religiosity groups when psychopathology was compared [Table 1]. Three other studies, however, have demonstrated the opposite. A study comparing psychopathology in religious and non-religious depressed adults demonstrated that religious persons with depression differed from non-religious persons with depression in that the former had less depressive cognitions but the same number of somatic symptoms.[42] In another study, it was seen that depressed persons belonging to a specific religious denomination called the Calvinists had more vegetative symptoms and more guilt than depressed Roman Catholics and non-church members.[28] It has also been seen that the inverse relationship between religious coping and depressive symptoms holds true especially for the cognitive symptoms of depression.[42] This can be due to various reasons. First of all, the dimension of religiosity that we have examined (religious belief) is different from the other three studies (religious affiliation, religious coping, religious involvement). The other difference is that ours was a clinic-based study with a relatively small sample size, whereas the others were large community-based studies.
Religiosity is a protective factor against suicidality as shown by several studies.[49] The current study also shows that, as expected, there is a negative correlation between religiosity and both hopelessness and suicidal intent. Stack proposed that the protective effect is due to various reasons like religious injunctions against suicide, provision of religious coping mechanisms, belief in help from God and social support.[50] The factors affecting the maintenance of hope and optimism have been studied extensively in palliative care medicine, especially in illnesses like malignancies and HIV infection. Religion was found to be one of the factors maintaining hope in patients diagnosed with AIDS.[51] Hope and optimism were the factors mediating the relationship between better psychological adjustment and higher levels of religiosity.[52] Even in the context of depression, it may be surmised that patients with higher religiosity believe in a supernatural power that has a positive influence on their lives and offers help when the patient himself or herself is depleted of all inner resources.
Future directions
Other dimensions of religiosity like religious practices, orientation, attitudes, religious commitment and well-being need to be studied and the measurements need to be done repeatedly over time. Further studies should be performed keeping a bidirectional relationship between depression and religiosity in mind. The replication of the study with a larger sample size and a community based-sample may make the results generalizable.
CONCLUSIONS
Religiosity has a significant effect on the psychopathology of the depressed patient, especially on hopelessness and suicidal intent. This implies that the incorporation of religious elements in the treatment of the depressed is likely to have a useful positive impact.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Sadock BJ, Sadock VA. Comprehensive textbook of psychiatry. 8th ed. Philadelphia: Williams and Wilkins; 2004. [Google Scholar]
- 2.Raguram R, Weiss MG, Keval H, Channabasavanna SM. Cultural dimensions of clinical depression in Bangalore, India. Anthropol Med. 2001;1:31–46. [Google Scholar]
- 3.Capps W.H. Psychology of religion. [Last accessed on 2011 Feb 28]. Available from: URL http://www.oneworldpublications.com .
- 4.Yinger JM. The scientific study of religion. New York: Macmillan; 1970. [Google Scholar]
- 5.Shafranske E, Malony HM. Clinical psychologists’ religious and spiritual orientations and their practice of psychotherapy. Psychotherapy. 1990;27:72–8. [Google Scholar]
- 6.Glock CY. On the study of religious commitment. Relig Educ and Res Suppl. 1962;57:s98–110. [Google Scholar]
- 7.Koenig HG. Handbook of religion and mental health. San Diego: Academic press; 1988. [Google Scholar]
- 8.American psychiatric association task force report 10: Psychiatrists’ viewpoints on religion and their services to religious institutions and the ministry. Washington D C: APA; 1975. [Google Scholar]
- 9.Kroll J, Sheehan W. Religious beliefs and practices among 52 psychiatric inpatients in Minnesota. Am J Psychiatry. 1989;146:67–72. doi: 10.1176/ajp.146.1.67. [DOI] [PubMed] [Google Scholar]
- 10.Larson DB, Pattison M, Blazer DG, Omran AR, Kaplan BH. Systematic analysis of research on religious variables in four major psychiatric journals 1978-1982. Am J Psychiatry. 1986;143:329–35. doi: 10.1176/ajp.143.3.329. [DOI] [PubMed] [Google Scholar]
- 11.King M, Dein S. The spiritual variable in Psychiatry. Psychol Med. 1999;28:1259–62. doi: 10.1017/s003329179800703x. [DOI] [PubMed] [Google Scholar]
- 12.Crossley D. Religious experience within mental illness: Opening the door on research. Br J Psychiatry. 1995;166:284–6. doi: 10.1192/bjp.166.3.284. [DOI] [PubMed] [Google Scholar]
- 13.Sims A. ‘Psyche’ – spirit as well as mind? Br J Psychiatry. 1994;165:441–6. doi: 10.1192/bjp.165.4.441. [DOI] [PubMed] [Google Scholar]
- 14.Piko BF, Fitzpatrick KM. Substance use, religiosity, and other protective factors among Hungarian adolescents. Addict Behav. 2004;29:1095–107. doi: 10.1016/j.addbeh.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 15.Podvoll E. Mania and the risk of power. J Contemplative Psychother. 1987;4:95–122. [Google Scholar]
- 16.Lewis CA. ‘Cleanliness is next to godliness’: Religiosity and obsessiveness. J Relig Health. 1998;37:49–61. [Google Scholar]
- 17.Trenholm P, Trent J, Compton WC. Negative religious conflict as a predictor of panic disorder. J Clin Psychol. 1998;54:59–65. doi: 10.1002/(sici)1097-4679(199801)54:1<59::aid-jclp7>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 18.Kendler KS, Liu XQ, Gardner CO, McCullough ME, Larson D, Prescott CA. Dimensions of religiosity and their relationship to lifetime psychiatric and substance use disorders. Am J Psychiatry. 2003;160:496–503. doi: 10.1176/appi.ajp.160.3.496. [DOI] [PubMed] [Google Scholar]
- 19.Berry D. Does religious psychotherapy improve anxiety and depression in religious adults? A review of randomized controlled studies. Int J Psychiatr Nurs Res. 2002;8:875–90. [PubMed] [Google Scholar]
- 20.Razali SM, Hasanah CI, Aminah K, Subramaniam M. Religious--sociocultural psychotherapy in patients with anxiety and depression. Aust N Z J Psychiatry. 1998;32:867–72. doi: 10.3109/00048679809073877. [DOI] [PubMed] [Google Scholar]
- 21.Meador KG, Koenig HG, Hughes DC, Blazer DG, George LK, Turnbull J. Religious affiliation and major depression. Hosp Community Psychiatry. 1992;43:1204–8. doi: 10.1176/ps.43.12.1204. [DOI] [PubMed] [Google Scholar]
- 22.Jones-Webb RJ, Snowden LR. Symptoms of depression among blacks and whites. Am J Public Health. 1993;83:240–4. doi: 10.2105/ajph.83.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braam AW, Beekman AT, van Tilburg TG, Deeg DJ, van Tilburg W. Religious involvement and depression in older Dutch citizens. Soc Psychiatry Psychiatr Epidemiol. 1997;32:284–91. doi: 10.1007/BF00789041. [DOI] [PubMed] [Google Scholar]
- 24.Hahn CY, Yang MS, Yang MJ, Shih CH, Lo HY. Religious attendance and depressive symptoms among community dwelling elderly in Taiwan. Int J Geriatr Psychiatry. 2004;19:1148–54. doi: 10.1002/gps.1204. [DOI] [PubMed] [Google Scholar]
- 25.Pressman P, Lyons JS, Larson DB, Strain JS. Religious belief, depression and ambulation status in elderly women with broken hips. Am J Psychiatry. 1990;147:758–60. doi: 10.1176/ajp.147.6.758. [DOI] [PubMed] [Google Scholar]
- 26.Cummings SM, Neff JA, Husaini BA. Functional impairment as a predictor of depressive symptomatology: The role of race, religiosity, and social support. Health Social Work. 2003;28:23–32. doi: 10.1093/hsw/28.1.23. [DOI] [PubMed] [Google Scholar]
- 27.Koenig HG, Cohen HJ, Blazer DG, Kudler HS, Krishnan KR, Sibert TE. Religious coping and cognitive symptoms of depression in elderly medical patients. Psychosomatics. 1995;36:369–75. doi: 10.1016/s0033-3182(95)71646-2. [DOI] [PubMed] [Google Scholar]
- 28.Baetz M, Griffin R, Bowen R, Koenig HG, Marcoux E. The association between spiritual and religious involvement and depressive symptoms in a Canadian population. J Nerv Ment Dis. 2004;192:818–22. doi: 10.1097/01.nmd.0000146735.73827.85. [DOI] [PubMed] [Google Scholar]
- 29.Dervic K, Oquendo MA, Grunebaum MF, Ellis S, Burke AK, Mann JJ. Religious affiliation and suicide attempt. Am J Psychiatry. 2004;161:2303–8. doi: 10.1176/appi.ajp.161.12.2303. [DOI] [PubMed] [Google Scholar]
- 30.Bainbridge W, Stark R. Suicide, homicide and religion. Annu Rev Social Sci Relig. 1981;5:33–56. [Google Scholar]
- 31.Koenig HG, George LK, Peterson BL. Religiosity and remission of depression in medically ill older patients. Am J Psychiatry. 1998;155:536–42. doi: 10.1176/ajp.155.4.536. [DOI] [PubMed] [Google Scholar]
- 32.Braam AW, Beekman AT, Deeg DJ, Smit JH, Van Tilberg W. Religiosity as a protective or prognostic factor of depression in later life; Results from a community survey in the Netherlands. Acta Psychiatr Scand. 1997;96:199–205. doi: 10.1111/j.1600-0447.1997.tb10152.x. [DOI] [PubMed] [Google Scholar]
- 33.The ICD-10 classification of mental and behavioural disorders. Geneva: Diagnostic criteria for research; 2004. World Health Organization. [Google Scholar]
- 34.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1967;4:561–72. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 35.Deka N, Broota KD. Moral Judgement and Religiosity: A comparative study of the majority and minority religious groups in India. University of Delhi, India: Unpublished Doctoral dissertation; 1985. [Google Scholar]
- 36.Deka J, Broota KD. Relation between level of religiosity and principled moral judgement among four religious communities in India. J Pers Clin Stud. 1988;4:151–6. [Google Scholar]
- 37.Hamilton M A. Rating scale for depression. J Neurol, Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: The hopelessness scale. J Consult Clin Psychol. 1974;42:861–5. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 39.Gupta SC, Anand R, Trivedi JK. Development of a suicidal intent questionnaire. Indian J Psychiatry. 1983;25:57–62. [PMC free article] [PubMed] [Google Scholar]
- 40.Gupta S, Kulhara P, Verma SK. Quality of life in schizophrenia and dysthymia. Acta Psychiatr Scand. 1998;97:290–6. doi: 10.1111/j.1600-0447.1998.tb10002.x. [DOI] [PubMed] [Google Scholar]
- 41.Koenig HG, Cohen HJ, Blazer DG, Pieper C, Meador KG, Shelp F, et al. Religious coping and depression in elderly hospitalized medically ill men. Am J Psychiatry. 1992;149:1693–700. doi: 10.1176/ajp.149.12.1693. [DOI] [PubMed] [Google Scholar]
- 42.Koenig HG, Cohen HJ, Blazer DG, Kudler HS, Krishnan KR, Sibert TE. Cognitive symptoms of depression and religious coping in elderly medical patients. Psychosomatics. 1995;36:369–75. doi: 10.1016/s0033-3182(95)71646-2. [DOI] [PubMed] [Google Scholar]
- 43.Brown DR, Gary LE. Religious involvement and health status among African-American males. J Natl Med Assoc. 1994;86:825–31. [PMC free article] [PubMed] [Google Scholar]
- 44.Ferraro KF. Firm believers? Religion, body weight and well-being. Rev Relig Res. 1998;39:224–44. [Google Scholar]
- 45.Fehring RJ, Brennan PF, Keller ML. Psychological and spiritual well-being in college students. Res Nurs Health. 1987;10:391–8. doi: 10.1002/nur.4770100607. [DOI] [PubMed] [Google Scholar]
- 46.Hallstrom T, Persson G. The relationship of social setting to major depression. Acta Psychiatr Scand. 1984;70:327–36. doi: 10.1111/j.1600-0447.1984.tb01217.x. [DOI] [PubMed] [Google Scholar]
- 47.Mosher JP, Handal PJ. The relationship between religion and psychological distress in adolescents. J Psychol Theol. 1997;25:449–57. [Google Scholar]
- 48.Schafer WE. Religiosity, spirituality and personal distress among college students. J Coll Stud Dev. 1997;38:633–44. [Google Scholar]
- 49.Stack S. Suicide: A 15-year review of the sociological literature.Part I: cultural and economic factors. Suicide Life Threat Behav. 2000;30:145–62. [PubMed] [Google Scholar]
- 50.Stack S. The effect of religious commitment on suicide: A cross-national analysis. J Health Soc Behav. 1983;24:362–74. [PubMed] [Google Scholar]
- 51.Hall BA. Ways of maintaining hope in HIV disease. Res Nurs Health. 1994;17:283–93. doi: 10.1002/nur.4770170407. [DOI] [PubMed] [Google Scholar]
- 52.Salsman JM, Brown TL, Brechting EH, Carlson CR. The link between religion and spirituality and psychological adjustment: The mediating role of optimism and social support. Pers Soc Psychol Bull. 2005;31:522–35. doi: 10.1177/0146167204271563. [DOI] [PubMed] [Google Scholar]


