Abstract
Background:
Elective caesarean section rates have risen over the last decade worldwide. The increase in this rate is not associated with clear benefit for the baby or mother but proportionally associated with increased morbidity for both. Neonatal adverse outcomes in infants born before 39 weeks of gestation are increased and increase progressively as gestational age at birth declines
Aim:
To compare neonatal outcomes of elective caesarean section performed at or beyond completed 37 weeks of gestation with ≥ 38 weeks of gestation.
Material and Method:
This is a prospective observational study. During the period from July 2010 through April 2011 a total 134 neonates delivered by elective Cesareans at term and were divided into two groups, those who were born (early term) before 38 weeks of gestation (37+0 – 37+6) and those who were born (late term) at or greater than 38 weeks of gestation. We analyzed the following variables sex, number of maternal parities, mode of anesthesia, Apgar score at first and fifth minute, respiratory complications, hypothermia, hypoglycemia, feeding difficulties and admission to neonatal intensive care unit.
Results:
During the period of the study 890 live births whether delivered by Cesarean section or normal vaginal delivery. Of these only 134 neonates fulfilling the inclusion criteria were included. About 50% of them were delivered before 38 weeks of gestation. We performed our analysis on those 134 neonates and we found a significant risk in the early Cesareans group in comparison to later group for development of respiratory complications (P=0.0001), hypothermia (P=0.0001) and feeding difficulty (P=0.0001).
Conclusion:
Significant reduction in the neonatal morbidities if the time of elective Cesareans is at completed 38 weeks or beyond 38 weeks of gestation. Further larger studies are needed to analyze the factors responsible for our new date regarding the hypothermia and feeding difficulty in neonates born electively by Cesareans before 38 completed weeks of gestation.
Keywords: Elective caesarean section, neonatal morbidities, neonatal outcome
Introduction
Elective caesarean section rates have risen over the last decade worldwide because of obstetrical recommendations and maternal request have the potential for a significant impact on public health and health care costs because of the morbidity associated with this subgroup. The increase in this rate is not associated with clear benefit for the baby or mother but proportionally associated with increased morbidity for both[1,3,4].
Moreover, these increases in cesarean delivery rates which may not always be explained by clinical indications have led to efforts to reduce the number of cesarean deliveries[2]. Neonatal adverse outcomes in infants born before 39 weeks of gestation are increased and increase progressively as gestational age at birth declines[5,6]. Infants born by cesarean section in comparison with those born vaginally are at increased risk for adverse respiratory outcomes, especially when delivery occurs before the onset of labor, even in infant who are delivered at or beyond 37 completed weeks of gestation, so it is very important to choose the correct timing for elective caesarean section to prevent unnecessary morbidities[5,6]. Tita et al noticed those elective repeat cesareans before 39 weeks of gestation are common and are associated with respiratory and other adverse neonatal outcomes[5].
The aim of our study is to evaluate the timing of planned elective cesarean delivery and morbidities of the newborns.
Materials and Methods
Makassed General Hospital (MGH) is a tertiary hospital in the center of the great Beirut which is affiliated with American university in Beirut medical center AUB-MC. During the period from July 2010 – March 2011 there were 890 live births, of these live births 134 neonates were delivered by Elective Cesarean Section (ECS) and included in our study.
The data for the study were collected prospectively using a questionnaire that was approved by institutional review board in our institution. The data from these questionnaires were analyzed for postnatal complications after Elective Cesarean Section (ECS).
Inclusion and Exclusion Criteria
In our study we included those who are singleton pregnancies planned for delivery by elective cesarean section at or greater than completed 37 weeks of gestation, with no prenatal complication or any maternal morbidity. Those who were delivered by urgent cesarean section or had any prenatal complications, any congenital anomalies, maternal medical or obstetrical morbidities that could affect the risk of neonatal morbidities, multiple pregnancies, elective cesarean sections after spontaneous rupture of membranes or signs of labor were excluded. Indications for ECS included maternal request, breech presentation or repeat cesarean section (Figure 1).
Fig. 1.
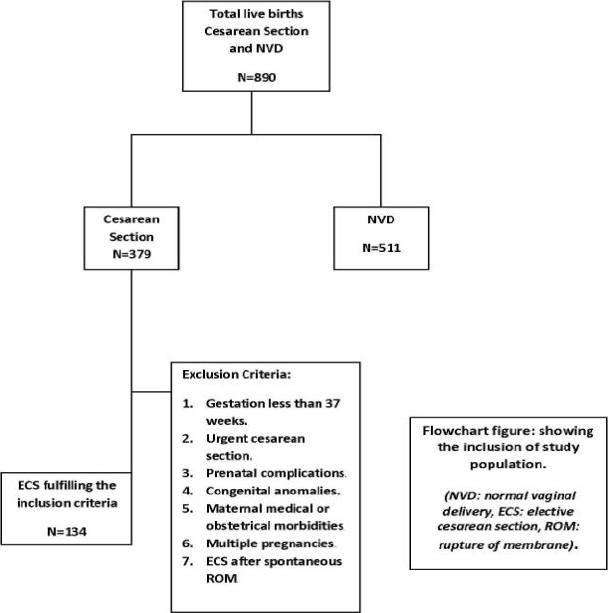
Flowchart figure for the inclusion of study population
Neonatal Follow-Up
In our institution, the neonates were accompanied since birth by a pediatrician and transferred to the regular nursery unit within a maximum of 15 minutes by the mean of an incubator preheated at set temperature (38C) to ensure a balanced thermal ambient.
At regular nursery unit newborns were kept under radiant warmer for about 1 hour during which they will be examined, glucose level and body temperature checked and bathing was delayed till body temperature was stable at ≥ 36.5C. The follow up of neonates stopped at discharge from the hospital, but if he/she transferred to NICU follow up was continued.
Neonatal Outcomes and Analysis
Our outcomes included respiratory complications (transient tachypnea of the newborn or respiratory distress syndrome), hypothermia (rectal temperature < 36C within 1 hour of life), hypoglycemia (< 40 mg/dl within 1 hour of life), feeding difficulties (lack of interest to feed or nausea) and admission to neonatal intensive care unit (admission to NICU for more than 3 days).
The data were analyzed with the use of SPSS (version 17) and the Chi-Square test was used to check the statistical difference between the two groups. P-value of less than 0.05 was considered to indicate the statistical significance. To achieve the objective of the study, we divided our study population into two groups those who were born at 37+0 -37+6 (early term) and those who were born at or greater than 38 weeks of gestation (late term).
A sample size equal to 68 patients in each group was found to be adequate to detect a decrease of 54% in the total respiratory complications in those patients who were born at ≥ 38 weeks of gestation with α= 5% and power of the study = 80%.The study was approved by the institutional review board of MGH and parental approval was obtained for the patients.
Results
During the study period July 2010 through April 2011, there were 890 deliveries. Of these, 379 neonates were delivered by cesarean section, 134 elective and 254 intrapartum. After exclusion, we included 134 neonates in our analysis.
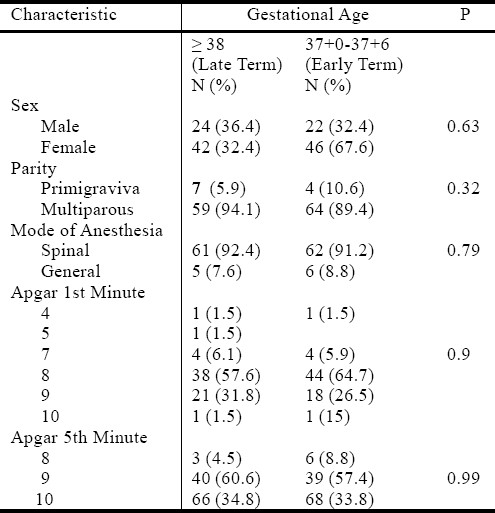
Among the women who underwent ECS, 123 (91.8%) were repeat ECS, 68 (50.8%) underwent the procedure at (early term) 37+0-37+6 weeks of gestation. If we compared the neonates in the two groups (Table 1) the mean maternal age was (29.9, 29.58 years) respectively [-1.72 to 2.36], and there were no significant differences between the two groups (i.e. Both groups were similar) regarding the mode of anesthesia (P=0.8) whether spinal or general, number of parity (P= 0.32) or neonatal gender (P=0.6) or birth weight of the newborns [-234.05 to 93.19].
Table 1.
The study population characteristics.
Regarding the other outcomes (Table 2, Figure 2), there were a very significant associating between (early term) group and the respiratory complication (P=0.0001, 5.81 [2.19-15.38]), hypothermia (P=0.0001, 45.5[5.96-347.54]) and feeding difficulty (P=0.0001). We could not calculate the odds ratio for feeding difficulty because there were no patients in the (late term) group. We did not find any association with hypoglycemia (P= 0.28, 1.86[0.59-5.88]) or admission to the NICU (P= 0.08).
Table 2.
The Outcome measures.
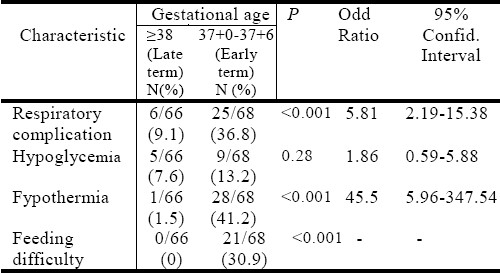
Fig. 2.
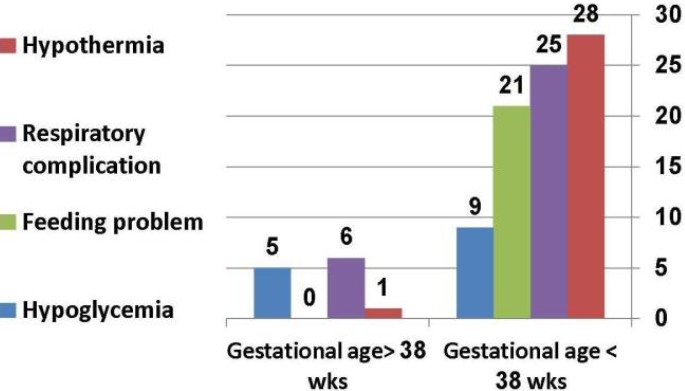
Comparison between the neonatal outcomes for both early and late term groups.
Discussion
In this study we analyzed 134 neonates who were born electively at term, 50% of them were delivered by ECS at early term. We divided the study population into two groups as we mentioned to achieve the objective of our study. Previous studies have stressed on neonatal outcomes like respiratory complications, hypoglycemia, neonatal sepsis and indirect hyperbilirubinemia[5–7,9] but to our knowledge none looked at the other outcomes like hypothermia or feeding difficulty.
We found that there were significantly higher risks in the early Cesareans group of various neonatal outcomes including respiratory complications, hypothermia and feeding difficulty. In the early Cesareans group the risk for respiratory complications is 5.8 times higher (P=0.0001) manifested most often as transient tachypnea of the newborn and this risk decreased as advancing the gestational age that is in line with those found by Tita et al, Signore et al and Wilmink et al[5–7,10,11].
Hansen and colleagues found that infants delivered by ECS at 37 weeks of gestation had a 10% incidence of respiratory complications[8,10, and 11], so our finding was comparable to what is already published in the literature.
On other hand, there were 45.5 times (P=0.0001) increase in the risk of development of hypothermia and a very significant development of feeding difficulty in early Cesarean group which were a surprising findings as it was not reported in the previous studies. We could not calculate the odds ratio for feeding difficulty because the late term group includes no patient.
We tried to look for explanations for these outcomes led us to review the transport flow of the neonates, nursery unit thermal ambient, radiant warmer and all the medications used in anesthesia, hopefully to detect a judicious clue about the causes for such morbidities, but we could not find any relation that could explain our new outcome.
In contrast to Tita et al[5], our data did not find any difference in hypoglycemia (P=0.28, [CI: 0.59-5.88]) or admission to NICU (P=0.08) between early and late cesareans. Our data add new morbidities to already known poor neonatal outcomes associated with unnecessarily early performed ECS before 38 completed weeks of gestation. These data should be taken into consideration by the obstetricians and the women counseling them to avoid whenever possible a jeopardized neonatal outcomes.
Conclusion
This study focuses the light on a new dark corner of neonatal morbidities secondary to unjustified early ECS. Conversely a significant reduction in the neonatal morbidities maybe obtained if the timing of planned elective Cesareans postponed till or beyond 38 weeks of gestation. Further larger studies are needed to analyze the factors responsible for our new date regarding the hypothermia and feeding difficulty in neonates born electively by Cesarean section before 38 completed weeks of gestation.
References
- 1.Pedersen P, Avlund OL, Pedersen BL, Pryds O. Intramuscular adrenaline does not reduce the incidence of respiratory distress and hypoglycaemia in neonates delivered by elective caesarean section at term. Arch Dis Child Fetal Neonatal Ed. 2009;94:164–167. doi: 10.1136/adc.2008.138487. [DOI] [PubMed] [Google Scholar]
- 2.Gould JB, Danielsen B, Korst LM, et al. Cesarean delivery rates and neonatal morbidity in a low-risk population. Gynecol Obstet. 2004;104(1):11–19. doi: 10.1097/01.AOG.0000127035.64602.97. [DOI] [PubMed] [Google Scholar]
- 3.Ramachandrappa A, Jain L. Elective Cesarean Section: It's Impact on Neonatal Respiratory Outcome. Clin Perinatol. 2008;35:373–393. doi: 10.1016/j.clp.2008.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Villar J, Carroli G. Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study. Brithsh Med J. 2007;335(7628):1025. doi: 10.1136/bmj.39363.706956.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tita ATN, Landon MB, Spong CY, et al. Timing of Elective Repeat Cesarean Delivery at Term and Neonatal Outcomes. N Engl J Med. 2009;360:111–120. doi: 10.1056/NEJMoa0803267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilmink FA, Hukkelhoven CWPM, Lunshof S, et al. Neonatal outcome following elective cesarean section beyond 37 weeks of gestation: a 7-year retrospective analysis of a national registry. Am J Gynecol Obstet. 2010;250:1–8. doi: 10.1016/j.ajog.2010.01.052. [DOI] [PubMed] [Google Scholar]
- 7.Signore C, Klebanoff M. Neonatal Morbidity and Mortality after Elective Cesarean Delivery. Clin Perinatol. 2008;35:361–371. doi: 10.1016/j.clp.2008.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hansen AK, Wisborg K, Uldbjerg N, Henriksen TB. Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. BMJ. 2008;336:85–87. doi: 10.1136/bmj.39405.539282.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Macdorman MF, Declercq E, Menacker F, et al. Infant and neonatal mortality for primary cesarean and vaginal births to women with “no indicated risk,” United States, 1998-2001. Birth Cohorts. Birth. 2006;33:175–182. doi: 10.1111/j.1523-536X.2006.00102.x. [DOI] [PubMed] [Google Scholar]
- 10.Levine EM, Ghai V, Barton JJ, Strom CM. Mode of delivery and risk of respiratory diseases in newborns. Obstet Gynecol. 2001;97:439–442. doi: 10.1016/s0029-7844(00)01150-9. [DOI] [PubMed] [Google Scholar]
- 11.Van den Berg A, van Elburg RM, Van Geijn HP, Fetter WP. Neonatal respiratory morbidity following elective cesarean section in term infants: a 5-year retrospective study and a review of the literature. Eur J Obstet Gynecol Reprod Biol. 2001;98:9–13. doi: 10.1016/s0301-2115(01)00292-5. [DOI] [PubMed] [Google Scholar]


