Abstract
Aim of the Study:
Subureteral endoscopic injection of a bulking agent is an attractive alternative to open surgery or antibiotic prophylaxis for vesico ureteral reflux (VUR). Little information is available about long-term risk of recurrence after an initially successful treatment. Aim of this paper was to review short- and long-term success rate of endoscopic treatment in a single Center series after risk stratification of individual patients.
Materials and Methods:
The records of 126 patients who underwent Deflux injection for primary VUR were examined. Indications to treatment were an unvaried high grade VUR (IV-V) at 1 year from diagnosis and/or and recurrent urinary tract infection (UTI) on antibiotic prophylaxis even in the presence of mild grade VUR (III grade). Gender, age and mode of diagnosis, infections (UTI), voiding dysfunctions, VUR grade and side, renal function, number of treatments were correlated to outcome. Long-term evaluation was planned at a minimum of 1 year from the last negative post-injection cystogram (MCUG). A new MCUG and DMSA scan were also offered to those complaining new UTI episodes. Late recurrences were correlated to history and grade of reflux. Data were analyzed with Graph Pad Instat software; the Chi-square test was used for univariate comparisons, the Fisher's exact test for categorical variables.and multiple regression tests for factors influencing outcome.
Results:
M/F ratio was 62 to 64; median age at diagnosis was 28 months. VUR affected 198 renal units. Preinjection VUR grade was I in 1, II in 27, III in 107, IV in 59, and V in 4 units. Reduced DMSA uptake was evidenced in 51 units and scarring in 24. Median age at treatment was 34.5 months, for persistent high grade VUR (IV–V) in 55 patients and recurrent IVU in 92. Two hundred sixty seven injections were performed on 198 ureters. Complete resolution was documented by MCUG at 3-5 months in 68%, low grading < II in 20%, persistence or unsignificant reduction in 11%. Preoperative recurrent UTI, higher grade VUR, and bilaterality were correlated to a poorer surgical outcome. Among 80 successfully treated cases, 12 complained of persistent UTI. Recurrence of VUR was demonstrated in 31% of them. Deteriorated uptake or additional scarring in 25% was independent from VUR recurrence. Preoperative recurrent UTI and voiding dysfunction correlated significantly to late outcome.
Conclusions:
Preoperative recurrent IVU, together with high-grade reflux, seem to correlate to lower success rate of Deflux injection for primary VUR. Even after successful endoscopic treatment, long-term surveillance may be needed among these cases, mainly if voiding dysfunction is also recorded. Late recurring VUR must be actively excluded in case of new IVU episodes.
Keywords: Endoscopic treatment, urinary tract infection, vesico ureteral reflux
INTRODUCTION
Vesico ureteral reflux (VUR) affects approximately 1% of all children, with a range of incidence between 20% and 35% in children with urinary tract infection (UTI).[1,2] It has been reported that VUR is diagnosed in 60% of children after an episode of UTI in the first year of life and in 30% beyond 2 years of age.[3] Low grade VUR (according to International Reflux Grading System) usually resolves spontaneously within the first years of life. A still inconclusive debate is pending about the value of different approaches to manage children with higher grade VUR, especially when urinary tract infections require continuous antibiotic prophylaxis.[4] Comparative analyses include conservative versus different surgical treatments, evaluating possible development of late complications. The research of a favored approach may underscore the need for a better risk-stratification of patients with VUR to offer the best treatment for each case. Relationship between reflux and pyelonephritis remains unclear. Children without documented VUR get pyelonephritis and scarring;[5] recurrent infections reflect a complex interaction between bacteria and host where reflux plays the role of an additional risk factor whose relevance is magnified by the possibility of effective surgical correction. The role of other nonsurgical options beyond antibiotic therapy, such as proper management of constipation and voiding disorders is too frequently under considered. Surgical treatment takes the risk to disregard other important factors which continue to influence clinical course and prognosis of individual cases despite the initial radiological “success”.[6–8] Evidences do not seem in favor of surgery over medical treatment, as far as long-term results are concerned.[9] Most of these studies reflect experiences based on the “gold standard” of traditional open anti reflux surgery.[10–11] Widespread diffusion of endoscopic treatment of VUR as an alternative to long-term antibiotic prophylaxis or open surgery meets families’ expectations for a “quick fix” solution to the problem, with a high success rate and few complications whenever medical approach appears inconclusive.[4,12,13] This solution despite its increasing popularity sill raises questions about long-term issues and durability.[6,12,14,15] The aim of the present study was
To review factors influencing the success among a single center series of primary VUR cases treated by single or repeated endoscopic Deflux®injection
To analyze long-term outcome (recurrent UTI, VUR recurrence, incidence of new renal scarring or further renal function damage) after an initially successful endoscopic treatment.
MATERIALS AND METHODS
One hundred twenty six patients were extracted from 214 children who underwent endoscopic treatment for VUR between January 2000 and December 2009, at the Pediatric Surgery and Pediatric Urology Unit of the San Camillo-Forlanini Hospital (Rome, Italy). We excluded patients with VUR associated to duplicated system, neurogenic bladder, posterior urethral valves, and contralateral obstructive uropathies. Patients’ records were revised to extract demographic and clinical data (gender, age, and mode of diagnosis, UTI, voiding dysfunctions, VUR grade and side, renal separate function and scars, age at first treatment, number of endoscopic treatments, final result). Reflux was diagnosed by Ultrasonography (US) and Micturating Cystouretrogram (MCUG); a Tc99-dimercaptosuccinic acid (DMSA) renal scan was always performed. VUR was scored according to the International Reflux Study grading system.[16] Indications of endoscopic treatment were an unvaried high grade VUR (IV–V) at 1 year from diagnosis and/or and recurrent UTI on antibiotic prophylaxis even in presence of mild grade VUR (III grade). Mild refluxes (I–II grade) were treated only if associated to contralateral higher grade VUR. Endoscopic treatment was always performed under general anesthesia by two senior pediatric urologists. Dextranomer/Hyaluronic Acid (Deflux®) was used as bulking agent in all cases. The needle was introduced submucosally under the ureteral orifice at the 6′o clock position and 1.0 ml of Deflux was injected (range 0, 5–2, 0 ml). The procedure was repeated twice or three times in cases of persistent VUR at a mean interval of 6 months (range 3 months–1 year). Open surgery was advised in cases of repeated failures. US was performed a week after the procedure to exclude secondary ureteral obstruction and MCUG after 3–5 months, to check VUR persistence. Treatment was recorded as successful after reflux disappearance or low grading < II. Antibiotic prophylaxis (ABP) was continued for almost 1 month after endoscopic correction. Long-term results were evaluated for patients who received endoscopic treatment only. A telephone interview was made at a minimum of 1 year from the last negative MCUG. Grade of parental satisfaction was scored using the Likert scale. Recurrent UTI episodes after successful VUR treatment were recorded. A new MCUG and DMSA scan were proposed for these patients. Results and time elapsed from last treatment were added to a database where age and symptoms at diagnosis (recurrent UTI, voiding dysfunctions independent from infectious episodes), initial grade and side of VUR, initial renal state, age at first treatment and number of treatments were reported. Data were analyzed with Graph Pad Instat software, version 3.10. The Chi-square test was used for univariate comparisons. The Fisher's exact test was used for categorical variables. Multiple regression tests were used for factors influencing successful endoscopic treatment of VUR and affecting long-term outcome. A value of P < 0.001 was considered significant.
RESULTS
Male female ratio was 62 to 64; median age at diagnosis was 28 months (range 1 month–14 years). Forty five patients (36%) had a prenatal diagnosis of hydronephrosis, whereas in 72 (57%) VUR was detected after single or recurrent episodes of UTI. In nine patients (7%) MCUG resulted positive after occasional discovery of pyelo-ureteral dilatation at an US performed for extra urinary reasons (vomiting, abdominal pain, or trauma). Dysfunctional voiding was recorded in 20 cases (5 males, 15 females); enuresis was always investigated as a possible spy of dysfunction. VUR was unilateral in 56 patients and bilateral VUR in 69 and affected 198 renal units. Preinjection VUR grade was I in 1, II in 27, III in 107, IV in 59, and V in 4 renal units. Whenever median age at diagnosis was considered it was 1.5 months for Grade V, 7 months for Grade IV, and 26 months for Grade III. Reduced renal uptake at DMSA scan was evidenced in 51 renal units and scarring in 24. Median age at the first endoscopic treatment was 34.5 months (range 5 months–14 years); indications were persistent high grade VUR (IV–V) in 55 patients (44%) and recurrent IVU under ABP in 92 (73%). We performed 267 Deflux injections on 198 ureters (mean 1.3 per ureter) with a maximum of two procedures for 62 patients (49%) and three for 4 (3%). Final results are illustrated on [Figure 1]. A complete reflux resolution was achieved in 79 patients (68%), low grading <2 in 21 (20%) while persistence or not significant reduction was recorded in 15 (11%), who underwent ureteric reimplantation for persistence of severe VUR, associated with recurrent UTI in 8. Four patients were lost at follow up and postoperative MCUG were not available. Multiple regression analysis was performed on the remaining 122 patients to calculate the impact of different prognostic factors on final outcome after endoscopic Deflux injection on single ureters. Results are reported in [Table 1].
Figure 1.
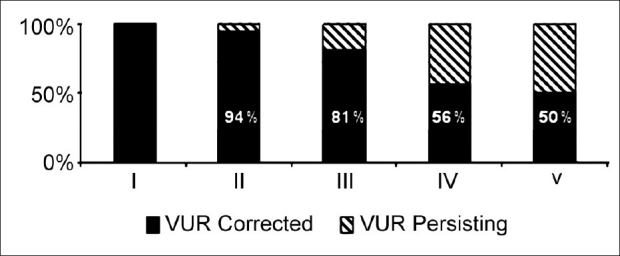
Final results of endoscopic treatment at 3–5 months vs grade of VUR (198 renal units in 126 patients)
Table 1.
Multiple regression analysis of outcome among 191 renal refluxing units in 122 patients treated by endoscopic deflux injection
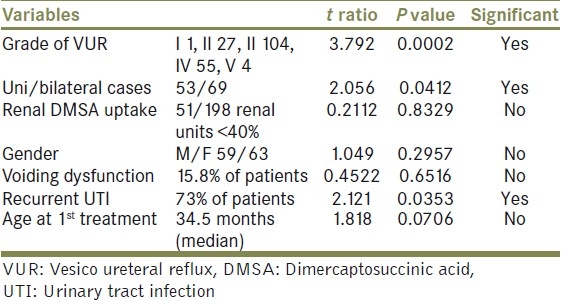
We found a significant negative correlation between grade, bilaterality, history of recurrent UTI, and resolution of reflux at 3 months from last Deflux injection. A telephone interview was made in those cases who
had a negative post injection MCUG done at least one year before the interview;
had not been submitted to open surgery after unsuccessful endoscopic treatment.
Eighty patients were selected (M/F ratio 39/41); mean age at control was 8.3 years (range 2–12). Time since last endoscopic treatment ranged from 13 to 148 months (mean 63). Parental satisfaction was tested. An excellent grade of satisfaction was reported in 85% of cases; the remaining 15% (12 patients) complained of persistent UTI and/or minor voiding disturbances, despite successful endoscopic treatment. All patients had a new MCUG and DMSA scan performed. Recurrence of VUR ≥ grade 2 was found in 5 out of 16 renal units (31%) and interested four out of 12 patients. New renal scars or further reduced renal uptake were found in 4 out 16 units (25%) and were associated to a recurrent VUR only in one case. Late recurrence of VUR in patients with a previous successful endoscopic treatment was correlated to clinical history of each patient. Gender, preinjection voiding dysfunction, recurrent UTI, VUR grade, uni/bilaterality, and renal uptake at diagnosis were taken into consideration. Multiple regression analysis results are reported in [Table 2].
Table 2.
Influence of different clinical variables on late recurrence of VUR outcome among 118 renal units in 80 patients successfully treated by endoscopic Deflux injection
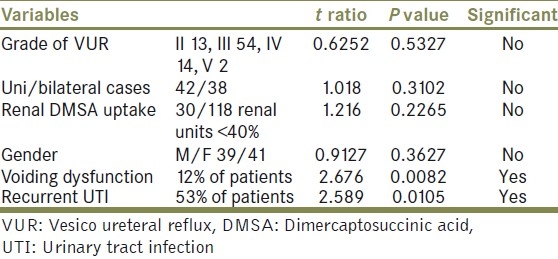
Twelve of our patients among those who could be included in the long-term follow up reported recurrent episodes of UTI despite successful endoscopic reflux correction. Recurrence of VUR was demonstrated in 31% of already treated ureteral units. Deteriorated renal function in terms of decreased uptake or additional scarring was documented in 25% independently from the presence of a new reflux. Symptomatic UTI and a history of voiding dysfunction were significantly associated to a higher rate of VUR recurrence even after a previously negative post injection MCUG. Further deterioration of renal uptake or new renal scars appeared to be dependent upon different clinical variables and not necessarily associated to a recurrent VUR.
DISCUSSION
Optimal management of VUR is still a controversial matter.[17] Even after several studies[18,19] we lack conclusive evidences in favor or against any reasonable treatment. Prenatally diagnosed VUR associated with congenital renal damage is a rather different entity than later observed symptomatic VUR associated with focal renal scarring and dysfunctional elimination syndrome (DES). Furthermore Gordon et al.,[20] showed that the presence of VUR is a weak predictor of the presence of renal damage in hospitalized children with UTI. The potential of spontaneous reduction of VUR during the follow-up has been quoted between 20% and 50% in 5-year follow-up.[21] The risk of UTI was estimated 57.6% among 735 patients during conservative management.[22] Grain et al.,[23] suggested the use of antibiotic prophylaxis in patients with primitive VUR associated with UTI to prevent renal parenchymal damage. The main advantage of antibiotic prophylaxis is avoiding invasive procedures; whereas the major disadvantage is persistence of reflux despite long-term treatment, with a low success rate after 1 year (33% in grade II-IV reflux).[24] International Reflux Study reported no difference between the medical treatment and surgical approach in children with III and IV grade VUR to prevent renal damage.[25] An individualized approach to children with VUR is therefore recommended considering individual risk factors like congenital upper tract anomalies associated with reflux and voiding habits; constipation and family compliance to conservative treatment; evaluation and management of a febrile illness or lower urinary tract symptoms. Endoscopic treatment for VUR was first introduced in 1981 by Matouschek[26] and was popularized by O’Donnell and Puri.[27] Injection of a bulking agent under ureteric meatal mucosa creates a solid support and elongates intramural ureter.[28] Many studies reported endoscopic treatment to be effective and safe as a first-line therapy for VUR; however, the ideal agent has not yet been identified.[29,30] Nowadays, Deflux and Macroplastique are the most frequently used bulking agents with a reported success rate between 68% and 90%.[31,32]
Endoscopic approach allows VUR correction with less hospital stay and morbidity.[33] Open surgery remains the gold standard of treatment in terms of long-term success rate and reduction of episodes of pyelonephritis; no differences, compared to medical treatment, of new asymptomatic UTI or renal damage have been reported.[34] Ureteral reimplant is currently reserved for cases of high grade persistent primary VUR following repeated unsuccessful endoscopic treatment.
Straightforward operative approach to VUR has become more attractive after endoscopic anti reflux procedures have been available and parental preferences are often claimed to support indications to early treatment even in mild grade VUR.[4] There is a risk of under evaluating individual risk factors which affect persistence of VUR and possible reflux-related renal damage and of confusing natural history of the disease. There are no evidences about long-term outcome of endoscopically treated patients after initial success documented by MCUG. Durability and prevention of long-term complications are still under discussion.[7,12,14,15]
The general rate of success after endoscopic treatment (70%) depends on different factors, such as, sex, grade of reflux and the number of pre-operative UTI.[7,12] This was confirmed in our series. Patients with ≥2 predictive factors, including febrile UTI, voiding dysfunction, and/or renal parenchymal defects on DMSA scan, may not be optimal candidates for endoscopic treatment for high risk of breakthrough infections and persistent reflux. Whenever endoscopic treatment is elected, these high-risk patients require a more vigilant follow-up, including MCUG, beyond 3 months. Children with > 3 episodes of recurrent preinjection UTI were 8.5 times more likely than those with only 1 pretreatment UTI to have an infection after Deflux injection. Recurrence of VUR among this group of patients ranges from 13% to 27%[7,8,12] and reached 31% in our series. Whenever initial severe renal scarring was detected further renal damage at DMSA scan was reported in 2,5% after successful reflux correction and in 6,1% after VUR recurrence.[35] Among our cases deteriorated uptake was detected at long-term follow up in 25% irrespectively from VUR recurrence.
CONCLUSIONS
Based on our experience, we conclude that aside from high reflux grade, recurrent UTI are significantly related to a lower success rate of endoscopic treatment of primary VUR. A preoperative history of recurrent UTI and voiding symptoms seems to be a significant risk factor for late recurrence of VUR and must be kept in consideration during long term follow up of this group of patients even after an initially favorable post injection MCUG. Further renal deterioration, independent from VUR persistence, supports the open debate on the largely unexplained relationship between reflux and parenchymal damage. On these bases current intervals of 3–5 months between this procedure and a negative control MCUG might not be enough to interrupt follow up. Especially if a voiding dysfunction history has been previously recorded on patients note, long-term surveillance is recommended and a new Cystogram may be required after symptomatic episodes of UTI. Nevertheless, progression of scars, independent from VUR persistence, casts further doubt on relationships between reflux and renal damage.
Footnotes
Source of Support: Nil,
Conflict of Interest: None.
REFERENCES
- 1.Decter RM. Vescicoureteral reflux. Pediatr Rev. 2001;22:205–10. doi: 10.1542/pir.22-6-205. [DOI] [PubMed] [Google Scholar]
- 2.Hellerstein S. Recurrent urinary tract infections in children. Pediatr Infect Dis. 1982;1:271–81. doi: 10.1097/00006454-198207000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Layton KL. Diagnosis and management of pediatric urinary tract infections. Clin Fam Pract. 2003;165:23–8. [Google Scholar]
- 4.Capozza N, Lais A, Matarazzo E, Nappo S, Patricolo M, Caione P. Treatment of vesico-ureteric reflux: A new algorithm based on parental preference. BJU Int. 2003;92:285–8. doi: 10.1046/j.1464-410x.2003.04325.x. [DOI] [PubMed] [Google Scholar]
- 5.Rushton HG, Majd M, Jantausch B, Wiedermann BL, Belman AB. Renal scarring following reflux and nonreflux pyelonephritis in children: Evaluation with 99mtechnetium-dimercaptosuccinic acid scintigraphy. J Urol. 1992;147:1327–32. doi: 10.1016/s0022-5347(17)37555-9. [DOI] [PubMed] [Google Scholar]
- 6.Lorenzo AJ, Khoury AE. Endoscopic treatment of reflux: Management pros and cons. Curr Opin Urol. 2006;16:299–304. doi: 10.1097/01.mou.0000232054.12461.5f. [DOI] [PubMed] [Google Scholar]
- 7.Sedberry-Ross S, Rice DC, Pohl HG, Belman AB, Maid M, Rushton HG. Febrile urinary tract infections in children with an early negative voiding cystourethrogram after treatment of vesico ureteral reflux with dextranomer/hyaluronic acid. J Urol. 2008;180(Suppl 4):1605–10. doi: 10.1016/j.juro.2008.04.071. [DOI] [PubMed] [Google Scholar]
- 8.Traxel E, DeFoor W, Reddy P, Sheldon C, Minevich E. Risk factors for urinary tract infection after dextranomer/hyaluronic acid endoscopic injection. J Urol. 2009;182(Suppl 4):1708–12. doi: 10.1016/j.juro.2009.02.088. [DOI] [PubMed] [Google Scholar]
- 9.Jodal U, Smellie JM, Lax H, Hoyer PF. Ten-year results of randomized treatment of children with severe vesico ureteral reflux. Final report of the International Reflux Study in Children. Pediatr Nephrol. 2006;21:785–92. doi: 10.1007/s00467-006-0063-0. [DOI] [PubMed] [Google Scholar]
- 10.Hodson EM, Wheeler DM, Vimalchandra D, Smith GH, Craig JC. Interventions for primary vesicoureteric reflux. Cochrane Database Syst Rev. 2007;3:CD001532. doi: 10.1002/14651858.CD001532.pub3. [DOI] [PubMed] [Google Scholar]
- 11.Weiss R, Duckett J, Spitzer A. Results of a randomized clinical trial of medical versus surgical management of infants and children with grades III and IV primary vesico ureteral reflux (United States).The International Reflux Study in Children. J Urol. 1992;148:1667–73. doi: 10.1016/s0022-5347(17)36998-7. [DOI] [PubMed] [Google Scholar]
- 12.Chi A, Gupta A, Snodgrass W. Urinary tract infection following successful dextranomer/hyaluronic acid injection for vesico ureteral reflux. J Urol. 2008;179:1966–9. doi: 10.1016/j.juro.2008.01.054. [DOI] [PubMed] [Google Scholar]
- 13.Bae YD, Park MG, Oh MM, Moon du G. Endoscopic subureteral injection for the treatment of vesico ureteral reflux in children: Polydimethylsiloxane (Macroplastique(R)) versus dextranomer/hyaluronic acid copolymer (Deflux(R)) Korean J Urol. 2010;51:128–31. doi: 10.4111/kju.2010.51.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Routh JC, Inman BA, Reinberg Y. Dextranomer/hyaluronic acid for pediatric vesico ureteral reflux: Systematic review. Pediatrics. 2010;125:1010–9. doi: 10.1542/peds.2009-2225. [DOI] [PubMed] [Google Scholar]
- 15.Lee EK, Gatti JM, Demarco RT, Murphy JP. Long-term followup of dextranomer/hyaluronic acid injection for vesico ureteral reflux: Late failure warrants continued followup. J Urol. 2009;181:1869–74. doi: 10.1016/j.juro.2008.12.005. discussion 1874-1875. [DOI] [PubMed] [Google Scholar]
- 16.Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE. International system of radiographic grading of vesico ureteral reflux. International Reflux Study in Children. Pediatr Radiol. 1985;15:105–9. doi: 10.1007/BF02388714. [DOI] [PubMed] [Google Scholar]
- 17.Lorenzo AJ. Medical versus surgical management for vesico ureteral reflux: The case for medical management. Can Urol Assoc J. 2010;4:276–8. doi: 10.5489/cuaj.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mathews R, Carpenter M, Chesney R, Hoberman A, Keren R, Mattoo T, et al. Controversies in the management of vesico ureteral reflux: The rationale for the RIVUR study. J Pediatr Urol. 2009;5:336–41. doi: 10.1016/j.jpurol.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keren R, Carpenter MA, Hoberman A, Shaikh N, Matoo TK, Chesney RW, et al. Rationale and design issues of the randomized intervention for children With vesico ureteral reflux (RIVUR) study. Pediatrics. 2008;122(Suppl 5):240–50. doi: 10.1542/peds.2008-1285d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gordon I, Barkovics M, Pindoria S, Cole TJ, Wolf AS. Primary vesico ureteral reflux as a predictor of renal damage in children hospitalized with urinary tract infection: A systematic review and meta - analysis. J Am Soc Nephrol. 2003;14:739–44. doi: 10.1097/01.asn.0000053416.93518.63. [DOI] [PubMed] [Google Scholar]
- 21.Birmingham Reflux Study Group. Prospective trial of operative versus non – operative treatment of severe vesicoureterak reflux in children: Five years’observation. Br Med J (Clin Res Ed) 1987;295:237–41. doi: 10.1136/bmj.295.6592.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silva JM, Santos Diniz JS, Marino VS, Lima EM, Cardoso LS, Vasconcelos MA, et al. Clinical course of 735 children and adolescents with primary vesico ureteral reflux. Pediatr Nephrol. 2006;21:981–8. doi: 10.1007/s00467-006-0151-1. [DOI] [PubMed] [Google Scholar]
- 23.Garin EH, Olavarria F, Garcia Nieto V, Valenciano B, Campos A, Young L. Clinical significante of primary vesico ureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: A multicentric, randomized, controller study. Pediatrics. 2006;117:626–32. doi: 10.1542/peds.2005-1362. [DOI] [PubMed] [Google Scholar]
- 24.Cendron M. Endoscopic treatment for vesico ureteral reflux: Let's not get carried away! Urology. 2006;68:242–3. doi: 10.1016/j.urology.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 25.Olbing H, Hirche H, Koskimies O, Lax H, Seppänen U, Smellie JM, et al. Renal growth in children with severe vesico ureteral reflux: 10-year prospective study of medical and surgical treatment: The International Reflux Study in Children (European branch) Radiology. 2000;216:731–7. doi: 10.1148/radiology.216.3.r00au35731. [DOI] [PubMed] [Google Scholar]
- 26.Matouschek E. Die Behandlung des vesikorenalen Refluxes durch transurethrale Einspritzung von Teflonplaste. Urologe. 1981;20:263–4. [PubMed] [Google Scholar]
- 27.O’Donnel B, Puri P. Treatmente of vescicoureteric reflux by endoscopic injection of Teflon. Br Med J (Clin Res Ed) 1984;289:7–9. doi: 10.1136/bmj.289.6436.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matouschek E. Treatment of vesicorenal reflux by transurethral teflon-injection (author's transl) Urologe A. 1981;20:263–4. [PubMed] [Google Scholar]
- 29.Capozza N, Caione P. Dextranomer/hyaluronic acid copolymer implantation for vesico-ureteral reflux: A randomized comparison with antibiotic prophylaxis. J Pediatr. 2002;140:230–4. doi: 10.1067/mpd.2002.121380. [DOI] [PubMed] [Google Scholar]
- 30.Elder JS, Diaz M, Caldamone AA, Cendron M, Greenfield S, Hurwitz R, et al. Endoscopic therapy for vesico ureteral reflux: A meta analysis. I. Reflux resolution and urinary tract infection. J Urol. 2006;175:716–22. doi: 10.1016/S0022-5347(05)00210-7. [DOI] [PubMed] [Google Scholar]
- 31.Ozyavuz R, Ozgur GK, Yuzuncu AK. Subureteric polydime- thylsiloxane injection in the treatment of vesico-ureteric reflux. Int Urol Nephrol. 1998;30:123–6. doi: 10.1007/BF02550564. [DOI] [PubMed] [Google Scholar]
- 32.Läkgren GA, Wahlin N, Sköldenberg E, Stenberg A. Long-term followup of children treated with dextranomer/hyaluronic acid copolymer for vesico ureteral reflux. J Urol. 2001;166:1887–92. doi: 10.1016/s0022-5347(05)65713-8. [DOI] [PubMed] [Google Scholar]
- 33.Austin JC, Cooper CS. Vesico ureteral reflux: Surgical approaches. Urol Clin North Am. 2004;31:543–57. doi: 10.1016/j.ucl.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 34.Mathews R, Carpenter M, Chesney R, Hoberman A, Keren R, Mattoo T, et al. Controversies in the management of vesico ureteral reflux: The rationale for the RIVUR study. J Pediatric Urol. 2009;5:336–41. doi: 10.1016/j.jpurol.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chertin B, Natsheh A, Fridmans A, Shenfeld OZ, Farkas A. Renal scarring and urinary tract infection after successful endoscopic correction of vesico ureteral reflux. J Urol. 2009;182(Suppl 4):1703–6. doi: 10.1016/j.juro.2009.03.011. [DOI] [PubMed] [Google Scholar]


