Abstract
Background:
Does cognitive screening rule out impairment of different cognitive functions of older adults in India? This study is an attempt to explore these issues.
Materials and Methods:
Study sample consisted of 89 Mixed version of Mini Mental State Examination and Hindi Mental State Examination (Mixed MMSE) negative older adults aged ≥60 years. Subjects giving informed consent for the study were recruited using inclusion/exclusion criteria from a randomly selected ward of urban Lucknow as consecutive series. Semi-structured proforma of sociodemographic details and Mixed MMSE were administered. Subjects scoring above 23 on Mixed MMSE and not having any significant physical illness in past one year which affects the activity of daily living were considered as normally aging older adults. These normally aging older adults (89) were further assessed on Brief Cognitive Rating Scale to identify level of cognitive functioning on different domains. Appropriate statistical test was used for data analyses using Statistical Package for Social Sciences (SPSS) 12.0 version.
Results:
Maximum normally aging older adults (51.7%) has mild level of objective dysfunction in “orientation” followed by “concentration” (22.5%). Significantly (P<0.05) higher number of normally aging males had objective dysfunction in “orientation” and in “functioning/self-care” in comparison with females. Similarly, significantly (P<0.05) higher number of subjects aged 70 years or more had subjective dysfunction on “recent and past memory” in comparison with those in 60 to 69 years of age.
Conclusion:
Normally ageing subjects had objective cognitive dysfunction in the areas of “orientation” and “concentration” and “functioning/self care.” It was found in more older adults with increasing age.
Keywords: Brief cognitive rating scale, cognitive dysfunction, memory, mixed mini mental state examination, normal ageing
INTRODUCTION
Cognitive function declines with advancing age particularly in older adults aged 60 years and above. Hence, concepts like normal ageing, age-related cognitive decline, mild cognitive impairment (MCI)/dysfunction, cognitive impairment/dysfunction, and cognitive disorders are used to denote cognitive status of an older adult. Different cut-off scores of the cognitive screening/assessment tools are in practice to differentiate between normal cognitive functioning and cognitive dysfunction/impairment as well as areas of cognitive dysfunction. But, most of these tools are not free from culture and education bias.[1–3] Chandra et al.[4] have hypothesized that in a low demanding society, cognitive impairment may go unnoticed by the subject and proxies. It is almost intuitive that in modern societies of the developed world, where new devices that rely on memory (and also on executive functions) are constantly introduced into daily life, the elderly are confronted with more challenging conditions and may complain and become more aware of memory impairments. If we take into account this, suggested cut-off scores of different tests and areas of cognitive dysfunction may differ across the globe.
A study[5] reported that normal aging should have a greater effect on performance in subtests that rely heavily on self-initiated processing (for example, free recall test) and those that involve associative information (for example, paired associate tests), but smaller effect on performance in tests that rely on generic ideas (for example, recall of story's gist) and those that involve a higher level of environmental support (for example, recognition tests). The types of memory that decline most with age are working memory and episodic memory. Episodic memory is responsible for remembering events and experiences that have happened to us personally, and shows the greatest age-related difference. Studies have reported that subjective memory impairment (SMI) may be the first manifestation of future dementia in elderly subjects.[6,7] A high prevalence of SMI (70%)[8] was found in a study, which was more frequent in women; however, age and education did not impact on prevalence.
Categorization of cognitive status of an older adult in India is mostly based upon standard criteria on western population except few.[9–12] Indian adaptations[13–16] of some tests developed in western countries have been done, but there are no normative data available for Indian population. There is dearth of Indian studies to focus upon this issue. Therefore, in the present study, it was explored which of the cognitive functions are mostly affected in normally ageing older adults, using a stringent methodology. The paper is based on an ongoing Ph.D. work entitled, “A clinical psychological study of cognitive functioning as a determinant of quality of life amongst urban elderlies” of author under the guidance of coauthor.
Aim
To study the status of cognitive functioning of normally aging older adults aged 60 years and above in urban Lucknow.
MATERIALS AND METHODS
Sample
Sample consisted of 89 older adults aged 60 years and above. Subjects giving informed consent to participate in the study were recruited using inclusion/exclusion criteria from a randomly selected Musahabganj ward of urban Lucknow as a consecutive series.
Inclusion criteria
-
Older adults (males and females) aged 60 years and above;
-
Confirmation of the age was done by following using one or more criteria:
- An authentic document/certificate
- Retirement year (if retired)
- Year of marriage+gap period of his/her eldest child birth+Age of eldest son/daughter = Age of the subject
- Date of birth before independence year (1947) of India respect to freedom of India
- Self and family assessment of the subject
-
Cooperative persons.
Exclusion criteria
Uncooperative persons;
Having been diagnosed as suffering from any major psychiatric disorder as a main or comorbid condition other than MCI and Dementia;
Having any problem suggesting significant organic pathology like head injury, seizure, mental retardation, substance abuse, etc., or having physical health problems which affects functioning of daily living of the individual during past one year;
Having problems with speech, hearing, and vision, which can impede the interview.
Tools
Semi-structured sociodemographic and personal history data sheet
Mixed Mini Mental State Examination (mixed version of Mini Mental State Examination[17] and Hindi Mental State Examination (HMSE)[9] was used to control the education and language bias)
Brief Cognitive Rating Scale (BCRS):[18] BCRS is divided into five axes: Concentration, recent memory, past memory, orientation, and functioning/self-care. It is a seven-point rating scale with increasing severity. Rating 1 denotes- No objective or subjective impairment in cognitive function, 2- subjective impairment /dysfunction and 3-7 – objective impairment/dysfunction.
Study procedure
A house-to-house survey was conducted to screen households where older adults aged 60 years and above were living to recruit study subjects as a consecutive series. After taking written informed consent, the subjects were included in the study according to inclusion and exclusion criteria. Sociodemographic and personal history data sheet and Mixed Mini Mental State Examination (Mixed version of MMSE[17] and HMSE[9]) were administered. Subjects scoring above 23 on Mixed MMSE and not having any significant physical illness in past one year which affects the activity of daily living were considered as normally aging older adults. Of the recruited 104 subjects, 89 subjects were found to be normally aging older adults. These 89 subjects were studied for their cognitive dysfunctioning using BCRS.[13]
Data were analyzed using SPSS 12.0 version. Statistical calculations were done, i.e., percentages, mean, SD, and χ2 with Yate's correction wherever applicable.
RESULTS
Of the total 104 included subjects, 89 (85.58%) elderlies were found to be Mixed MMSE negative (scored above 23) and 15 (14.42) elderlies were positive (scored below 24). Of 89 Mixed MMSE negative elderlies, 47 (52.8%) were males and 42 (47.2%) were females. Mean score of Mixed MMSE-negative subjects was found to be 26.2±2.7 and on BCRS it was 7±2. The mean age of the studied elderlies was 67.25±5.1 years. Most of the subjects (68.5%) studied up to below primary level and were married (75.2%). The mean years of schooling of the subjects was found to be 5±3 years.
Table 1 shows that maximum normally aging older adults (51.7%) had objective cognitive dysfunction in the area of “orientation” followed by “concentration” (22.5%), “functioning/self care” (19.1%), and very less number of older adults in “recent memory” (3.4%). Objective dysfunction in “past memory” was not found in normally aging older adults. It is also evident from Table 1 that significant difference was found on the domain of “recent memory” between no dysfunction and objective dysfunction (P<0.05). Significantly higher number of normally aging male subjects had objective dysfunction on “recent memory” than females. Gender-wise difference was found statistically significant (P<0.05) on the domain of “orientation” between no dysfunction vs objective dysfunction (P<0.05) and on the domain of “functioning/self-care” between subjective dysfunction and objective dysfunction. Significantly higher number of males had subjective dysfunction in “orientation” and objective dysfunction in “functioning/self-care” in comparison with females.
Table 1.
Sex-wise comparison of cognitive dysfunctions on BCRS of normally ageing subjects
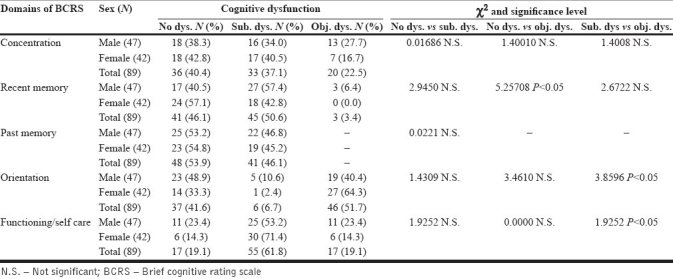
Subjective dysfunction on the domain of “functioning/self care” was found to be in 61.8% older adults followed by in “recent memory” (50.6%), “past memory” (46.1%), and “concentration” (37.1%). Very less older adults reported subjective dysfunction on the domain of “orientation” (6.7%).
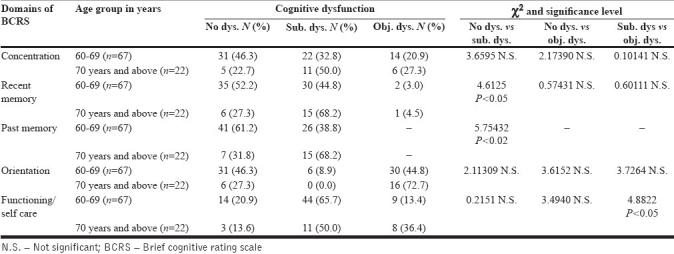
Table 2 shows that significant differences were found on no dysfunction vs objective dysfunction in the areas of “recent memory” (P<0.05) and “past memory” (P<0.02) and between subjective dysfunction vs objective dysfunction on “functioning/self care” (P<0.05) on the domains of BCRS between age group of 60-69 years and 70 or more than 70 years group. Significantly higher (68.2%) number of subjects aged 70 or more than 70 years had subjective dysfunction on “recent memory” in comparison with those of 60 to 69 years of age (44.8%). Findings were same for “past memory” also. Significantly higher number of elderly had subjective dysfunction in “functioning/self-care” in comparison with objective dysfunction. Older adults aged 60 years and above had subjective dysfunction (65.7%) and objective dysfunction was found in 36.4% urban older adults aged 70 years and above.
Table 2.
Age-wise comparison of cognitive dysfunctions on BCRS of normally ageing subjects
DISCUSSION
The study was conducted to assess status of the cognitive functioning of normally aged older adults aged 60 years and above and found that maximum older adults (51.7%) had objective cognitive dysfunction in the area of “orientation” followed by “concentration” (22.5%), “functioning/self care” (19.1%), and a very less number of older adults had cognitive dysfunction in “recent memory” (3.4%). There was no impairment in “past memory” and a very less number of older adults (males only) had objective dysfunction on “recent memory.” Objective dysfunction among normally aging older adults aged more than 70 years was found to be more in comparison with 60 to 69 years on all the areas of BCRS.
Gender differences in cognitive dysfunction have been found among normally ageing older adults. Males were found to have significantly more cognitive dysfunction than females on “recent memory,” ”orientation,” and “functioning/self-care.” Contradictory result was found in a study,[16] but it was for severity of the symptoms, not for percentages of females. Increasing age is related to poorer performance on tasks of memory (recent and past), and functioning/self-care. The result is similar to two studies[16,19] which have been explained as a result of aging brain in patients.
Objective cognitive dysfunction in normally aging subject was found maximum in the area of “orientation” followed by “concentration.” Most of the older adults are not well worse with some items of orientation, i.e., date, year, name of the block, district or the Nation even after controlling the education bias. It was also found in the study that the ability of “functioning/self care” and “concentration” diminish with advancing age. Least affected cognitive function was “recent memory” and objective dysfunctioning was not found in “past memory” among normally aging older adults. It suggests that “memory” was the least affected and “orientation” was the most affected cognitive functions in normally aging older adults.
Subjective dysfunction in “memory” has been reported by most of the normal older adults aged more than 70 years of age. However, objective dysfunction was found more on “orientation” and on “functioning/self-care” in the normally aging older adults aged 70 years and above. These objective dysfunctions in the areas of “orientation” and “functioning/self-care” may be taken into account while diagnosing the older adults in India. The observations are based on a small sample and it indicates that study may be conducted on large sample across India. There is a need, thus, to develop culture-free cut-off scores for cognitive screening and assessment tools for older adults in India.
ACKNOWLEDGMENT
The study was carried out along with an ICMR, New Delhi-sponsored research project, “An epidemiological study of prevalence of neuropsychiatric disorders with special reference to cognitive disorders amongst urban elderly.”
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Tiwari SC, Tripathi RK, Kumar A. Applicability of the Mini Mental State Examination (MMSE) and the Hindi Mental State Examination (HMSE) to the urban elderly in India: A pilot study. Int Psychogeratr. 2009;1:123–8. doi: 10.1017/S1041610208007916. [DOI] [PubMed] [Google Scholar]
- 2.Jones RN, Gallo JJ. Education bias in the Mini-Mental State examination. Int Psychogeriatr. 2001;13:299–310. doi: 10.1017/s1041610201007694. [DOI] [PubMed] [Google Scholar]
- 3.Jorm AF, Scott R, Henderson AS, Kay DW. Educational level differences on the Mini-Mental State: The role of test bias. Psychol Med. 1998;18:727–31. doi: 10.1017/s0033291700008424. [DOI] [PubMed] [Google Scholar]
- 4.Chandra V, Pandav R, Dodge HH, Johnston JM, Belle SH, DeKosky ST, et al. Incidence of Alzheimer's disease in a rural community in India: The Indo- U.S. study. Neurology. 2001;57:985–9. doi: 10.1212/wnl.57.6.985. [DOI] [PubMed] [Google Scholar]
- 5.Luo L, Craik F. Aging and memory: A cognitive approach. Canadian J Psychiatry. 2008;53:346–53. doi: 10.1177/070674370805300603. [DOI] [PubMed] [Google Scholar]
- 6.Gauthier S, Reisberg B, Zaudig M, Petersen RC, Ritchie K, Broich K. International Psychogeriatric Association Expert conference on mild cognitive impairment.Mild Cognitive Impairment. Lancet. 2006;367:1262–70. doi: 10.1016/S0140-6736(06)68542-5. [DOI] [PubMed] [Google Scholar]
- 7.Jessen F, Wiese B, Cvetanovska G, Fuchs A, Kaduszkiewicz H, Kolsch H, et al. Patterns of subjective memory impairment in the elderly: Association with memory performance. Psychol Med. 2007;37:1753–62. doi: 10.1017/S0033291707001122. [DOI] [PubMed] [Google Scholar]
- 8.Brucki SMD, Nitrini R. Subjective memory impairment in a rural population with low education in the Amazon rainforest: An exploratory study. Int Psychogeriatr. 2009;21:164–71. doi: 10.1017/S1041610208008065. [DOI] [PubMed] [Google Scholar]
- 9.Ganguli M, Ratcliff G, Chandra V, Sharma S, Gilby J, Pandav R, et al. A Hindi version of the MMSE: The development of a cognitive screening instrument for a largely illiterate rural elderly population in India. Int J Geriatr Psychiatry. 1995;10:367–7. [Google Scholar]
- 10.Pershad D, Verma SK. Agra, India: National Psychological Corporation; 1990. Handbook of PGI Battery of Brain Dysfunction (PGIBBD) [Google Scholar]
- 11.Mathuranath PS, Cherian JP, Mathew R, George A, Alexander A, Sarma SP. Mini mental state examination and the Addenbrooke's cognitive examination: Effect of education and norms for a multicultural population. Neurol India. 2007;55:106–10. doi: 10.4103/0028-3886.32779. [DOI] [PubMed] [Google Scholar]
- 12.Gupta S, Khandelwal SK, Tandon PN, Maheshwari MC, Mehta VS, Sundaram KR, et al. The development and standardization of a comprehensive neuropsychological battery in Hindi (adult form) J Pers Clin Stud. 2000;16:75–109. [Google Scholar]
- 13.Gupta A, Kumar KK. Indian adaptation of Cognistat: Psychometric properties of a cognitive screening tool for patients of traumatic brain injury. Indian J Neurotrauma. 2009;6:123–32. [Google Scholar]
- 14.Srinivasan S. The concise cognitive test for dementia screening: Reliability and effects of demographic variables as compared to the mini mental state examination. Neurol India. 2010;58:702–7. doi: 10.4103/0028-3886.72167. [DOI] [PubMed] [Google Scholar]
- 15.Mathuranath PS, Hodges HR, Mathew R, Cherian JP, George A, Bak TH. Adaptation of the ACE for a Malayalam speaking population in southern India. Int J Geriatr Psychiatry. 2004;19:1188–94. doi: 10.1002/gps.1239. [DOI] [PubMed] [Google Scholar]
- 16.Das SK, Banerjee TK, Mukherjee CS, Bose P, Biswas A, Hazra A, et al. An urban community-based study cognitive function among non-demented elderly population in India. Neurol Asia. 2006;11:37–48. [Google Scholar]
- 17.Folstein MF, Folstein SE, Me Hugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:789–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 18.Reisberg B, Ferrish SH. Brief Cognitive Rating Scale (BCRS) Psychopharmacol Bull. 1988;24:629–6. [PubMed] [Google Scholar]
- 19.Srinivasan L, Thara R, Tirupati SN. Cognitive dysfunction and associated factors in patients with chronic schizophrenia. Indian J Psychiatry. 2005;47:139–43. doi: 10.4103/0019-5545.55936. [DOI] [PMC free article] [PubMed] [Google Scholar]


