Abstract
Context:
Central venous catheter-related bloodstream infection (CRBSI) is associated with high rates of morbidity and mortality in critically ill patients.
Aims:
This study was conducted to determine the incidence of central venous catheter-related infections (CRIs) and to identify the factors influencing it. So far, there are very few studies that have been conducted on CRBSI in the intensive care unit in India.
Settings and Design:
This was a prospective, observational study carried out in the medical intensive care unit (MICU) over a period of 1 year from January to December 2004.
Materials and Methods:
A total of 54 patients with indwelling central venous catheters of age group between 20 and 75 years were included. The catheters were cultured using the standard semiquantitative culture (SQC) method. Statistical analysis used SPSS-10 version statistical software.
Results:
A total of 54 CVC catheters with 319 catheter days were included in this study. Of 54 patients with CVCs studied for bacteriology, 39 (72.22%) catheters showed negative SQCs and also negative blood cultures. A total of 15 (27.77%) catheters were positive on SQC, of which 10 (18.52%) were with catheter-associated infection and four (7.41%) were with catheter-associated bacteremia; the remaining one was a probable catheter-associated bacteremia. CRIs were high among catheters that were kept in situ for more than 3 days and emergency procedures where two or more attempts were required for catheterization (P < 0.05). In multivariate analysis of covariance duration of catheter in situ for >3 days, inexperienced venupucturist, more number of attempts and emergency CVC were associated with more incidence of CVCBSIs, with P <0.02. The duration of catheter in situ was negatively correlated (-0.53) and number of attempts required to put CVC was positively correlated (+0.39) with incidence of CVCBSIs. Sixty-five percent of the isolates belonged to the CONS group (13/20). Staphylococcus epidermidis showed maximum susceptibility to amikacin, doxycycline and amoxycillin with clavulanic acid and was susceptible to vancomycin (100%). Klebsiella pneumoniae was 100% susceptible to amikacin and ciprofloxacin. Escherichia coli was susceptible to amikacin and cefotaxime.
Conclusions:
The overall incidence of CRI was 27.77% (15/54). Catheter-associated BSIs were 47.31 per 1000 catheter-days. CRI was low in the catheters inserted by the experienced venipuncturists, elective procedure and CVC kept in situ for ≤3 days. S. epidermidis was the most common isolate.
Keywords: Catheter-related infection, catheter-associated infection, semiquantitative culture
Introduction
The problem of central line-associated bloodstream infections has gained increasing attention in recent years. They cause a great deal of morbidity and deaths, and increase health care costs. Central venous catheters (CVCs) are increasingly used in hospitals to manage critically ill patients. Catheter-related bloodstream infections (CRBSIs) occurring in the intensive care unit (ICU) are common, costly and potentially lethal. They provide secure access to the central circulation for infusion therapy, nutritional support, hemodynamic monitoring, plasmapheresis, apheresis and hemodialysis. CVCs have a higher infection risk than other indwelling vascular access lines. This causes significant morbidity and mortality to the critically ill patient.[1,2] CRBSIs are considered among the first and most “preventable” classes of nosocomial infections.[3] Patients with CVCs are at risk of developing local as well as systemic infectious complications like local insertion-site infection, CRBSI, septic thrombophlebitis, endocarditis and other metastatic infections. The most serious complications are bacteremia, sepsis and death.[4] The definitive diagnosis of catheter infection can be made by using a combination of clinical signs and symptoms together with the quantitative culture techniques.[5] CVC catheterisation is often associated with serious infectious complications, mostly CRBSI, resulting in significant morbidity, increased duration of hospitalization and additional medical costs. The majority of CRBSIs are associated with CVCs, and the relative risk for CRBSI is significantly greater with CVCs than with peripheral venous catheters. So far, there are very few studies that have been conducted on CRBSI in India. This study was undertaken to determine the incidence of CVC-related infections in the ICU and to identify the factors influencing it, which would help to institute better prophylactic measures.
Materials and Methods
This study was carried out at Padmabhushan Vasantdada Patil General Hospital Sangli and Government Medical College Hospital, Miraj. This study was carried out over a period of 1 year, from January 2004 to December 2004. The study was approved by the ethical committee of Govt. Medical College, Miraj. This was a prospective, observational study.
Aims and objectives
To study the incidence of infections associated with CVC.
To study the various factors influencing the CVC infection.
To differentiate between contaminated and infected CVCs using semiquantitative culture (SQC) and blood culture methods.
To identify the organisms involved in the causation of catheter-related infections (CRIs).
To study the antibiotic susceptibility patterns of the isolated organisms.
A total of 137 patients underwent central venous catheterization in the medical intensive care unit (MICU) for various indications. A total of 54 (39.41%) patients with age group between 20 and 75 years of both genders with indwelling CVCs were included and the remaining (n = 83) were excluded according to the exclusion criteria in the current study admitted under the MICU.
Exclusion criteria
Patients with obvious source of infection were excluded (fever, pneumonia, urinary tract infection, cellulitis, septicemia) by history, clinical examination, blood culture, chest X-ray, urine examination, etc. and relevant investigations pertaining to the suspected infection.
Patients having infective endocarditis, retroviral disease and immunosuppressive drugs.
Patients whose catheter was put outside our hospital.
Type of catheter material used was Cavafix® Certo®14 Gauge/35 cm length. A presterlized polyurethane insertion set was used for various central venous cannulations.
Central venous catheterization
During catheter insertion, hand disinfection using an antiseptic rub was preferred. The use of clean gloves after hand hygiene was recommended. The maximal sterile barrier precautions in the form of use of cap, mask, sterile gloves, full-sleeved sterile gown and large sterile drapes were used. For the insertion of CVCs, full scrub (up to the elbows) with an antiseptic solution was used. To prepare clean skin, alcoholic chlorhexidine (2%) was preferred. Sterile gauze or sterile transparent dressing was performed at the catheter site. The use of topical antibiotic ointments or creams at the insertion site was avoided. Hand hygiene procedures were strictly followed (even when gloves were worn) before and after injection, blood sampling, dressing or any contact with the CVC or insertion site. The gauze dressings were changed every 2 days, the site was inspected for purulence and erythema and palpated for tenderness and induration (local signs of CVC infection). The CVC was placed according to the indication of its insertion and was held in situ by a single suture. All lines were placed percutaneously using the Seldinger technique (Committee for the Development of Guidelines for the Prevention of Vascular Catheter Associated Infection; Indian Society of Critical Care Medicine.. Acknowledgements. Indian J Crit Care Med 2003;7:16-16).
Experienced venupucturist
Greater than or equal to 25 independent central catheterization procedures within 3 months was considered as experienced venupucturist.
Less-experienced venipuncturists
Less than 25 independent central catheterization procedures within 3 or more months was considered as less experienced venupucturist.
Clinical data
Detailed clinical history of the patients was recorded for indication for catheterization, site of insertion of catheter, type of placement: emergency/elective, number of attempts required to place the CVC, length of catheter inside the patient (<20 cm/>20 cm), duration of placement (<72 h/>72 h), indication for removal, infection at catheter-insertion site, systemic antibiotic therapy and experience of the venipuncturist (<25/≥ 25 venipunctures).
Indications of central venous catheters
In the present study, we enrolled patients without obvious source of infection at the time of admission to avoid false-positive results of catheter tip by SQC method and to keep results more specific for CVC BSIs. We have chosen the indications for CVC where it is required for parenteral fluid supplementation, for inotropic support, CVP monitoring and to monitor patients with cardiorespiratory failure. (Organophosphorus poisoning, cerebrovascular accident, congestive cardiac failure, dilated cardiomyopathy, liver cirrhosis, GB syndrome, hypokalemic periodic paralysis, chronic cor-pulmonale, acute pulmonary embolism, myxodema coma with pericardial effusion, neuroparlalytic snake bite, status epilepsy and acute myocardial infarction with cardiogenic shock.)
Sample collection
The distal 5 cm of the CVC was collected aseptically in a sterile test tube and transported immediately to the laboratory for culture. Immediately subsequent to catheter removal, 5 ml of blood was collected aseptically from the peripheral vein in trypticase soya broth for blood culture. The catheters were cultured using the standard SQC method described by Maki et al. After SQC, the segment was immersed in trypticase soya broth. The plate was incubated at 37°C and colony count was recorded after 48 h.[6] For qualitative culture, trypticase soya broth containing catheter segment was incubated as 37°C and then subcultured on Blood agar and MacConkey's agar plates after 24, 48 and 72 h. The plates were incubated for 24 h at 37°C. Blood collected from the peripheral vein in trypticase soya broth for qualitative culture was incubated at 37°C. Subcultures were made on Blood agar and MacConkey's agar plates after 24, 48 and 72 h.[7] The plates were incubated for 24 h at 37°C. All the colonies grown were examined for the morphology followed by Gram staining and were identified by standard methods of Koneman.[8]
Antibiotic susceptibility testing was performed for all isolates on Muller-Hinton agar. The susceptibility test was carried out by the standard Kirby Bauer disc diffusion method. The selection of antibiotic for sensitivity was based on the National Committee for Clinical Laboratory Standards (NCCLS) guidelines and suggestions of clinicians.[9,10]
The results of the catheter tip and blood cultures were interpreted according to Widmer et al. before labeling a particular episode as catheter-related sepsis.[11]
Negative semiquantitative culture technique
A negative SQC result was defined as an SQC yielding less than 15 colony forming units (cfu) in the absence of positive blood culture.
Catheter-associated infection
An SQC yielding 15 cfu or more in the absence of a positive blood culture was considered to indicate CAI, and was reported as the number of cfu of the cultured microorganism [Figure 1].
Figure 1.
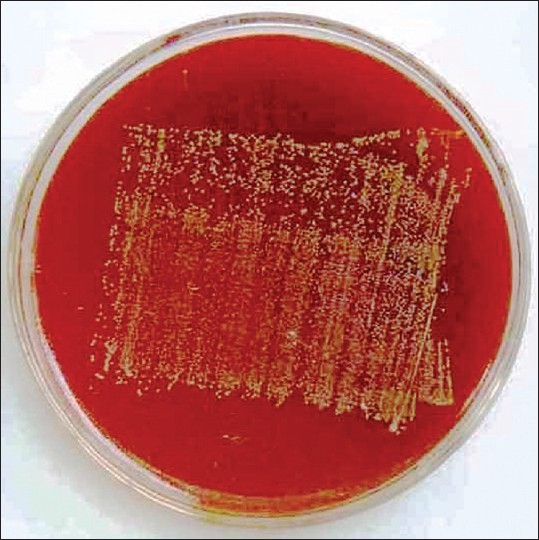
Semiquantitative culture of catheter tip on blood agar showing >15 cfu
Probable catheter-associated bacteremia
Probable catheter-associated bacteremia (CAB) was defined as a positive blood culture with no obvious catheter site infection and a negative SQC or an SQC yielding a microorganism different from that isolated from the blood.
Definite CAB
Definite CAB was defined as a positive blood culture and a positive tip culture yielding the same species of microorganism with the same antimicrobial susceptibility pattern.
Statistical analysis for mean, percent, standard deviation and chi-square test was performed by SPSS-10 version statistical software.
Results
A total of 137 patients underwent central venous catheterization in the MICU for various indications. A total of 54 (39.41%) patients in the age group between 20 and 75 years of both genders with indwelling CVCs were included. Of 54 patients, 32 (59.25%) were males and 22 (40.74%) were females. Sixteen (29.62%) of them were above the age of 60 years, followed by 14 (25.92%) patients who were between 41 and 50 years. A total of 24 (44.44%) patients were between 20 and 40 years of age. The mean age for males was 50.15 (±11.89) years and that for females was 53.95 (±16.65) years. The minimum age was 20 years and the maximum age was 75 years, with an overall mean age of 51.7 (±14) years. The mean for the duration of CVC in situ was 7 (±5) days. A total 13 patients were of organophosphorus poisoning, 11 were with cerebrovascular accident, seven were with congestive cardiac failure, two were with dilated cardiomyopathy, five were with liver cirrhosis with portal hypertension with hepatic encephalopathy, one was with GB syndrome, one with hypokalemic periodic paralysis, two with chronic cor-pulmonale, one with acute pulmonary embolism, one myxodema coma with pericardial effusion, two with neuroparlalytic snake bite, two with status epilepsy and five with acute myocardial infarction with cardiogenic shock.
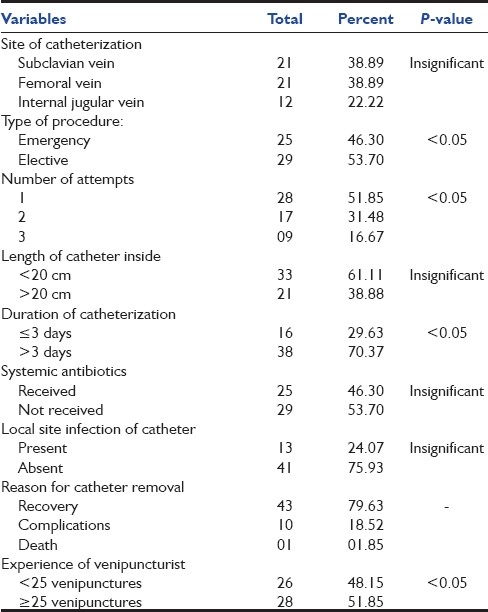
Subclavian route was used in 21 (39.89%) patients, femoral route in 21 (39.89%) and internal jugular route in 12 (22.22%) patients. Twenty-five (46.30%) procedures were done as emergency procedures and 29 (53.70%) as elective procedures. Twenty (51.85%) catheters were placed in the first attempt, 17 (31.48%) in two attempts and nine (16.67%) in three attempts. A total of 16 (29.63%) catheters were placed in situ for less than 3 days and 38 (70.37%) were placed for more than 3 days. In 33 (61.11%) patients, the length of catheter inside the vein was less than 20 cm and in 21 (38.89%) patients, the length of catheter inside the vein was more than 20 cm. A total of 25 (46.30%) of the patients had received antibiotics, whereas 29 (53.70%) did not receive any antibiotics. Local catheter site infection was present in 13 (24.07%) and absent in 41 (75.93%) of the patients. A total of 28 (51.85%) catheters were placed by experienced venipuncturists and 26 (48.15%) by less experienced venipuncturists. A total of 43 (79.63%) catheters were removed due to recovery of the patients, 10 (18.52%) due to complications and one (1.85%) due to death of the patient [Table 1].
Table 1.
Prevalence of central catheter-related factors
Of the 54 patients with CVCs studied, 39 (72.22%) catheters showed negative SQCs and, also, negative blood cultures. A total of 15 catheters were positive on SQC, of which 10 (18.52%) were with CAI and four (7.41%) were with CAB; the remaining one was probable CAB [Table 2 and Figure 2]. In one patient, blood culture showed Escherichia coli, but the SQC of catheter tip showed Staphylococcus haemolyticus. This patient was found to have urinary tract infection. The urine culture yielded E. coli with antibiogram identical with blood isolate. We studied 54 patients with CVCs inserted in the MICU over a period of 12 months with 319 catheter-days, and 15 (27.77%) BSIs. The rate of BSI associated with CVCs placed in the MICU was 47.31 per 1000 catheter-days (95% confidence interval 13.9–59.7). The mean duration of catheterization was 4.5 days (median 4; range 1–17 days). Among infected CVCs, the mean duration of catheterization was 8.6 days (median 7; range 2–18 days).
Table 2.
Incidence of catheter-related infections

Figure 2.

Incidence of central venous catheter-related infection
Sixty-five percent of the isolates belonged to the CONS group (13/20). In these 13 CONS, nine were S. epidemidis (45%), three were S. haemolyticus and one was S. saprophyticus. One isolate each of S. epidemidis and S. haemolyticus from the catheter tip culture was reciprocated from blood culture, showing identical colony morphology and antibiogram. A similar phenomenon was observed in one case of S. aureus infection and one case of Klebsiella pneumoniae infection. E. coli was isolated from the blood culture of one patient. Candida albicans was recovered from a catheter tip [Table 3 and Figure 3].
Table 3.
Organisms causing central venous catheter-related infection

Figure 3.
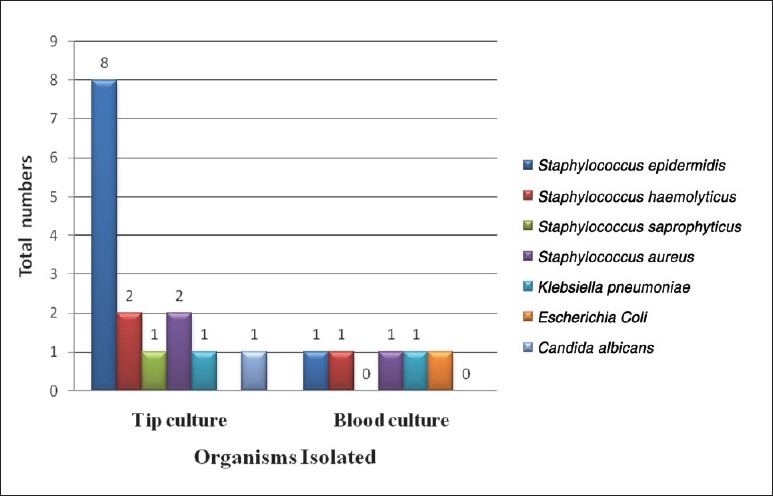
Organisms causing central venous catheter-related infection
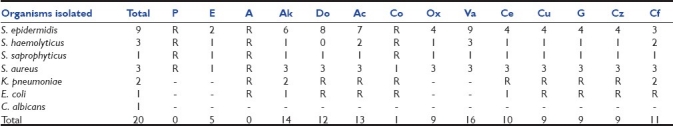
Antimicrobial susceptibility testing of all the isolates was performed by the Kirby Bauer disc diffusion method. All staphylococcal isolates showed 100% resistance to penicillin and ampicillin. S. epidermidis showed maximum susceptibility to amikacin, doxycycline and amoxycillin/clavulanic acid. Of nine isolates of S. epidermidis, four (44.4%) were susceptible to oxacillin and all isolates (100%) were susceptible to vancomycin. S. haemolyticus showed maximum susceptibility to amoxycillin/clavulanic acid and ciprofloxacin. Of three isolates, one isolate was susceptible to oxacillin whereas all three isolates were susceptible to vancomycin. S. saprophyticus, which was isolated from a single catheter, was resistant to penicillin, ampicillin and cotrimoxazole and susceptible to the rest of the antibiotics. S. aureus showed 100% resistance to penicillin and ampicillin and were least susceptible to erythromycin and cotrimoxazole. S. aureus showed maximum susceptibility to other antibiotics. K. pneumoniae (2/2) was 100% susceptible to amikacin and ciprofloxacin and resistant to other antibiotics. E. coli was susceptible to amikacin and cefotaxime and resistant to other antibiotics [Table 4].
Table 4.
Organsisms isolated and their antibiotic susceptibility pattern
Of 22 subclavian venous catheters, seven (33.33%) were infected. CRIs with femoral and internal jugular venous catheters were five (23.81%) and three (25%), respectively. There was no significant difference in the incidence of CRI of subclavian, femoral and internal jugular venous catheters.
A total of 21 catheters were placed for ≤3 days, of which two (9.52%) were associated with infection. Of the 33 catheters placed for more than 3 days, 13 (39.39%) were infected. The CRI increased with the duration of catheterization. CRI was statistically significant among patients with catheter for >3 days duration, with a P-value of <0.05. Of 21 CVCs that were inserted as an emergency procedure, nine (42.86%) showed CRI. A total of 33 catheter insertions were done as elective procedures, of which six (18.18%) were infected. CRI was higher in the emergency procedure than in elective procedures, with a P-value of <0.05. Of 28 central venous catheterizations done in a single attempt, one (3.57%) showed CRI. A total of six (35.29%) catheters out of 17 catheters inserted in two attempts and eight (88.89%) out of nine catheters inserted in three attempts were infected. CRI was highest among the catheters that were inserted in three attempts, and lowest in catheters placed in the first attempt, with a P-value of <0.05. Of 54 patients, 25 patients received antibiotics and 29 did not receive any antibiotics. Of these, eight (32%) patients who received antibiotics developed infectious complications. Among the patients who did not receive any antibiotics, seven (24.14%) developed infectious complications. There was no statistical significant correlation of CRI and use of systemic antibiotics. In the present study, catheter culture positivity was 33.3% in catheters having a length of <20 cm and 23.8% in catheters having a length of >20 cm inside. There was no significant correlation of CRI with length of catheter inside. Of 24 catheters inserted by less experienced venipuncturists, i.e. those who have done <25 catheterizations, 10 (41.67%) were associated with infection. Five (16.67%) out of 30 catheters inserted by experienced venipuncturists (≥25) were infected. CRI was higher in the catheters inserted by less experienced venipuncturists, with a P-value of <0.05. A total of 13 (24.07%) patients showed local infections at the site of catheterization. However only three (5.5%) of them had catheter infection. The remaining 10 (76.92%) patients did not show catheter infection in spite of local site infection. There was no correlation between the local catheter insertion-site infection and CRI. In multivariate analysis of covariance, duration of catheter in situ for >3 days, inexperienced venupucturist, more number of attempts and emergency CVC was associated with more incidence of CVCBSIs, with P <0.02. The duration of catheter in situ was negatively correlated (-0.53) and number of attempts required to put CVC was positively correlated (+0.39) with incidence of CVCBSIs.
Discussion
Vascular catheters are the most frequently used indwelling medical devices and have become necessary tools for the successful treatment of patients with chronic or critical illness. Placement of these catheters however has an associated risk of morbidity and mortality. In most cases, this is outweighed by the benefit gained, especially when long-term access to the central venous system is needed. Extensive experience with this technique has lead to the recognition of infectious complications that may result from its use and factors affecting infection rate. Thus, the definitive diagnosis of CRI can be made only by using a combination of clinical signs and symptoms together with the culture of the catheter. A prominent problem in detecting infection of intravascular catheters is the difficulty in distinguishing infection from contamination. This distinction has become easy with the SQC technique.
A total of 54 patients with CVCs with 319 catheter-days were included in the present study. Patients with any obvious source of infection were not included in the study. The rate of bloodstream infection associated with CVCs placed in the MICU was 47.31 per 1000 catheter-days. An attempt was made to study the incidence, bacteriology and risk factors associated with CRIs. In the present study, out of 54 patients with CVCs, 15 were infected, with incidence of CRI being 27.77%. Incidence of CAI was 18.52% and definite CAB was 7.41%. Over the years, various workers have reported an incidence of CRI raging from 2.7% to 60%. Catheter infection rate was 11.8% in a study done by Haslett.[12] In a multicentric study, Richet et al. reported an incidence rate of central CAB of 5%.[5] Groeger et al. reported that the incidence of CRI was ranging from 2.7% to 60%.[13] The incidence rate of catheter sepsis in standard catheters was 7.5% in a study done by Pemberton et al.[14] Safdar et al. reported an incidence of 2.7% (5.9 per 1000 CVC days).[15] Trick et al. in their study of 106 CVCs with 682 catheter-days reported that the primary BSI rate was 4.4 per 1000 catheter-days.[16] LeMaster et al. reported the rate of BSI associated with CVCs placed in the emergency department to be 1.93 per 1000 catheter-days in one study and prevalence of 0–32.8/1000 catheter-days for central line-related BSI in another study.[17,18] Koh et al. reported the incidence per 1000 catheter days CRBSI to be 16.8 (13.3–21.3).[19] Lucet et al. in their study of 3532 catheters and 27,541 catheter-days quoted CVC infection of 11.1/1000 catheter-days.[20] According to Fortun et al., the rate of incidence of tip colonization was 2.9 per 1000 catheter-days and of bacteremia was 1.2 per 1000 catheter-days.[21] Similarly, Deshpande et al. in 2005 in their study reported that the incidence of catheter infection was 4.01/1000 catheter-days (2.29% catheter) and colonization was 5.07/1000 catheter-days (2.89% catheters), which was low.[22] The rate of BSI associated with CVCs placed in the present study was 47.31 per 1000 catheter-days, which is quite high compared with these studies. This variability of incidences in various studies could be due to various factors like techniques, site of catheterization, type of catheter used, catheter care and diagnostic criteria used for diagnosing CRIs. The high infective complication rate in the present study may have been due to the fact that our hospital is catering to the lower socioeconomic group. Therefore, the overall hygiene of the patients is poor. Secondly, the patient population consisted mainly of elderly people above the age of 60 years, and it was usually done as an emergency procedure.
Maki et al., who evaluated the SQC technique for identifying infection due to intravenous catheters, found this technique to be 100% sensitive and 100% specific in detecting the CAB.[6] In the present study, out of 54 catheters studied, 15 (27.88%) catheters were positive on SQC. Of these, 10 (18.5%) were associated with CAI, one was probable CAB and four (7.41%) were definitive CAB. Maki et al. found that 21% of the catheters studied were positive on SQC, of which 8.4% were CAB.[6] Widmer found that 7% of the catheters were positive on SQC, of which 3.8% were associated with only CAI and 5% with BSI.[11] Cobb found that 21% of the catheters studied were positive on SQC, of which 16% were associated with local CAI and 5% with bloodstream infection.[23] Charalambous et al. found that 34% of the catheters studied were positive on SQC.[24] Similarly, Juste et al. found that 33.6% of the CVCs were positive on SQC.[25] Aufwerber et al. found that 25% of the catheters were positive on SQC and 18% were CAB.[26]
In the present study, painting was done with alcoholic chlorhexidine (2%) and sterile gauze with sterile transparent dressing was done at the catheter site. The use of topical antibiotic ointments or creams at the insertion site was avoided. The catheter dressings were changed every second day. According to Mermel et al., the choice of CVC dressing may be a matter of preference and cost. However, they preferred gauze dressing if blood was oozing from the catheter insertion site.[27] Maki et al. found that chlorhexidine provided the best protection against catheter colonization, with an incidence of 2.3%, followed by 70% alcohol with 7.1% infection rate and then by 10% povidone-iodine, which was 9.3%.[28] Similarly, Mimoz et al. concluded that the rate of catheter-related sepsis was 12 per 1000 catheter-days in the 4% alcohol-based solution of 0.25% chlorhexidine gluconate-treated sites when compared with 21 to per 1000 catheter-days 0.025% benzalkonium chloride with for 10% povidone-iodine.[29]
In the present study, out of 20 isolates, 65% were coagulase-negative staphylococci. S. epidermidis was the most commonly isolated coagulase-negative staphylocci comprising of 45%, followed by S. haemolyticus 15% and then S. saprophyticus 5% of the total isolates. Out of 13 CONS, 11 isolates were from the catheter tip and two were from blood culture. Many authors have reported CONS as a major isolate from the patients suspected of CRI by catheter culture. Richet et al. found that 46.5% of the isolates were S. epidermidis from both central and peripheral venous catheters.[5] Widmer et al. found that 11 (7%) out of 157 catheters were positive by CONS, being the most common organism.[11] Moonen et al. studied 23 episodes of fever in patients with CVCs. Of these, 10 episodes were due to CONS.[30] Velasco et al. studied that the most common isolates from blood in patients with hematology disease and solid tumors were CONS. Oxacillin resistance was seen in 61.8% of CONS.[31] In the present study, of a total of 20 isolates, three (15%) were S. aureus. Of these, two (10%) were isolated from the catheter tip culture and one (5%) was from blood culture. It was the second most common organism isolated from the catheter tip and blood cultures. Snydman et al. found that 25% catheter-related sepsis were caused by S. aureus.[32] Richet et al. in 1990 isolated S. aureus as the second most common microorganism from both central and peripheral venous catheters, accounting for 19.9% of all isolates.[5] O’Grady et al. reported that S. aureus was the second most frequently isolated microorganisms causing BSIs, accounting for 10% of the infections. More than 50% of all S. aureus isolates from the ICUs were resistant to oxacillin.[7] Schwaber et al. detected CVC-associated bacteremia using apheresis product culture. Methicillin-susceptible S. aureus (MRSA) were isolated from these infections.[33] In the present study, out of 20 isolates, two (10%) were K. pneumoniae. Of these, one (5%) was from the catheter tip and the other 5% were from blood culture with same antibiotic susceptibility pattern. This patient was suffering from multiple myeloma. The catheter tip was probably infected due to hematogenous seeding of the microorganism. Maki reported four cases of catheter-related septicemia, of which one was associated with Klebsiella species.[28] Similarly, in a study by Haslett, K. pneumoniae comprised 5% of the total isolates.[12] Richet found that 1.2% cases of CRI were due to K. oxytoca.[5] In our study, E. coli was isolated from blood culture in one patient. The tip culture of this patient showed S. haemolyticus. This patient had self-retaining urinary catheter. The probable cause of E. coli septicemia was urinary tract infection due to catheterization. Bozzetti analyzed the causes and routes of infection due to CVC. He isolated E. coli from 17 catheters, but every time it came from distant foci.[34] In our study, out of 20 isolates, C. albicans was isolated from a single catheter tip (5%). By SQC method, Maki isolated Candida species from two catheter tips, of which one was associated with CRS.[28] Snydman isolated three Candida species from three different catheters, which included C. tropicalis, C. parapsilosis and C. albicans. Of these, three episodes were due to Candida species that included C. albicans and C. tropicalis.[32] Haslett et al. found that 3% of the catheters were infected due to C. tropicalis.[12] Similarly, Widmer recovered C. albicans, which comprised 31% of the total isolates.[11]
Antimicrobial susceptibility testing by the Krebry Breur disc diffusion method of all organisms was carried out. All gram positive cocci showed 100% resistance to penicillin. S. epidermidis showed maximum susceptibility to erthromycin, ampicillin, amikacin, doxycycline and ciprofloxacin. Of the nine isolates of S. epidermidis, five isolates were resistant to oxacillin. All nine (100%) isolates were susceptible to vancomycin. S. haemolyticus showed maximum susceptibility to erythromycin, amikacin and ciprofloxacin. Of three isolates of S. haemolyticus, two isolates were resistant to oxacillin, but all three (100%) isolates were susceptible to vancomycin. S. saprophyticus was isolated from a single catheter tip culture. It was resistant to penicillin and cotrimoxazole but susceptible to other antibiotics tested. Similarly, S. aureus showed maximum susceptibility to all the antibiotics except for penicillin, which was 100% resistant. All the three (100%) isolates were oxacillin-susceptible S. aureus. Multiple drug resistance was found in gram negative organisms. K. pueumoniae isolates were resistant to all the antibiotics except amikacin and ciprfloxacin. Similarly, E. coli was resistant to all the antibiotics except amikacin and cefotaxime. According to Winston et al., in their study, at least 50% of the CONS were resistant to erythromycin, penicillin, oxacillin and clindamycin, while 18% were resistant to cephalothin. Vancomycin susceptibility testing was performed on two isolates, and both were sensitive to vancomycin.[35] Velasco et al. studied that 61.8% of the CONS isolated from blood were resistant to oxacillin.[31] Kloos et al. in their study showed that many of the CONS species were commonly resistant to antibiotics that are being indicated for staphylococcal infections, with the exception of vancomycin.[36]
In present study, the incidence of catheter infection was 33.33% in subclavian venous catheters. In femoral and internal jugular venotheters, the rate of infection was 23.81% and 25%, respectively, with no statistical difference in the incidence of CRI. Deshpande et al. reported that there was no statistically significant difference in the incidence of infection and colonization at the subclavian, internal jugular and femoral sites. These findings were comparable with our study.[22] According to Mermel et al., the internal jugular vein catheters were associated with increased risk of infection. This was due to the close proximity to oropharyngeal secretions, presence of hair in the area, catheter motion and difficulty in maintaining sterile dressing.[3] Lorente et al. in their study concluded that the order, to minimize the CVC-related infection risk, should be subclavian (first order), jugular (second order) and femoral vein (third order).[37] In the CDC guidelines, catheter insertion at the subclavian site is recommended in preference to femoral and jugular accesses. Kemp et al. stated that in patients receiving total parenteral nutrition, femoral site was at greater risk for CRI. The overall incidences of catheter colonization were 36% for femoral, 17% for internal jugular and 5% for subclavian sites.[38]
In the present study, 16 catheters for placed for ≤3 days, of which only two (12.5%) were infected. Of the 38 placed for more than 3 days, 13 (34.21%) were infected. The CRI increased with the duration of catheterization. According to Eyes et al., the patients requiring central catheters for <72 h had zero catheter-related sepsis incidence. The patients with central catheters for >7 days had a significant incidence of bacteremia and death.[39]
A total of 29 CVCs were inserted as an emergency procedure, of which nine (36%) were infected. And, 29 catheters were inserted as an elective procedure, of which six (20.69%) were infected. CRI was higher when emergency procedures were performed compared with elective procedures. Similarly, Maki et al. stated that catheters placed in the emergency room were more likely to produce severe phlebitis than were catheters placed in an inpatient unit.[40]
In our study, 28 out of 54 catheters were placed in a single attempt, 11 in two attempts and nine in three attempts. Of these, one (3.57%) was infected in a single attempt and six (35.29%) and eight (88.89%) in the second and third attempts, respectively. CRI was highest among the catheters that were inserted in the third attempt and least in those inserted in a single attempt. Richet et al. reported that there is a positive correlation between the number of attempts at catheterization and the sepsis rate.[5]
In the present study, catheter culture positivity was 33.3% in catheters having a length of <20 cm and 23.8% in catheters having a length >20 cm inside. There was no significant correlation of CRI with length of catheter inside. According to McGee et al., the average safe insertion depth for CVCs through subclavian or internal jugular veins was shown to be 16.5 cm for the majority of the adult population.[41]
In the present study, of 54 patients, 25 received antibiotics and 29 did not receive any antibiotics. Of these, eight (32%) patients who received antibiotics developed infection and seven (24.14%) developed infection among patients who did not receive any antibiotics. The use of systemic antibiotics was not shown to confer any protection from CAI. Mermel et al. stated that antibiotic therapy for CRI is often initiated empirically. Although there are no data that support the use of specific empirical antibiotic therapy for device-related blood stream infection, vancomycin is usually recommended in those hospitals with an increased incidence of MRSA.[3]
In the present study, out of 54 patients, 13 catheters were associated with local site infections and 41 without infection. Of these, three (23.08%) catheters were infected and 12 (29.27%) were not associated with infection. There was no correlation between the local catheter insertion site infection and CRI.
Of 54 catheters, 26 were inserted by less experienced venipuncturist (i.e., those who have done <25 catheterizations) and 28 by experienced venipuncturists (≥25 catheterizations). A total of 10 (38.46%) catheters inserted by less experienced venipuncturists were infected and five (17.86%) inserted by experienced venipuncturists were infected. CRI was higher in the catheters inserted by less experienced venipuncturists. This shows that experience of the venipuncturist was an important factor influencing CRIs. Similarly, Maki et al. stated that the experience of the person inserting an intravenous catheter clearly influences the risk of catheter-related sepsis.[40] Similar to the results of the present study, Safdar et al. stated that increased risk of CRBSI was associated with inexperience of the operator and nurse-to-patient ratio in the ICU, catheter insertion with less than maximal sterile barriers, placement of a CVC in the internal jugular or femoral vein rather than subclavian vein and duration of CVC placement >7 days.[42]
In our study, of a total of 54 patients, 43 (79.63%) of CVC were removed because they were no longer needed. The catheters were removed in 10 (18.52%) patients, which was attributed to complications due to central venous catheterization. Only one (1.85%) patient with CVC died, of which the cause of death was not related to the CVC infection. Catheters should be removed when infection is suspected because there can be a higher incidence of catheter-related bacteremia. Therefore, catheter insertion site should be inspected daily for the presence of infection. Zhang et al. stated that vascular devices cultured conventionally and reported as noninfective may at times potentially be a significant source of sepsis in critically ill patients. Alternative methods may be required for the accurate diagnosis of CRI in critically ill patients.[43]
The present study represents central venous CRBSIs in patients admitted with critical illness in MICU in the hospitals that cater to the relatively lower socioeconomic group. Many prospective multicentric studies should be conducted for better management of CRI by proper knowledge of catheter tip bacteriology, which will prevent indiscriminate use of antibiotics and future development of multidrug-resistant organisms.
Limitations of the study
The population in the present study sample is small. More prospective studies of sufficient size and to address all potential risk factors will enhance our understanding of the pathogenesis of CVC-related BSI and guide to develop more effective strategies for their prevention.
Conclusions
The overall incidence of CRI in the present study was 27.77%. The incidence of CAI was 18.56% and of definitive CAB was 7.41%. The rate of BSI associated with CVCs placed in the MICU was 47.31 per 1000 catheter-days. S. epidermidis was the most common organism isolated from the CVC infections. All staphylococci were resistant to penicillin and ampicillin. Majority of the isolates were susceptible to amikacin, doxycycline and amoxycillin/clavulanic acid. Oxacillin susceptibility was seen in 56.25% of CONS. All staphylococci were susceptible to vancomycin. Gram negative bacilli showed multidrug-resistant patterns. CRIs were high among catheters that were placed for more than 3 days. CVC infections were higher in emergency procedures as compared with elective procedures. Central various catheter infections were high in patients where two or more attempts were required for catheter insertion compared with single attempt catheterization. The use of systemic antibiotics did not reduce the CRI in the present study. CRI was low in the catheters inserted by experienced venipuncturists. Preventive measures against these infections include placement and maintenance of catheters by a skilled infusion-therapy team, coating of catheters with antiseptic agents and the use of silver-impregnated cuffs (for short-term CVCs) and topical disinfectants such as chlorhexidine, chlorhexidine-impregnated sponge dressing, CVCs with an antiinfective coating, antiinfective CVC hubs and novel needleless connectors and topical antibiotics. The antimicrobial sensitivity patterns of common isolates provide guidelines for the intensivist in critical care medicine to start appropriate empirical antibiotic therapy depending upon the clinical scenario. This can be cost-effective and can prevent indiscriminate use of antibiotics. The importance of strict asepsis and ideal catheter care has to be reinforced. All intensivists are required to follow standard protocols that uniformly demand the use of sterile gowns, gloves, masks and large drapes during insertion to reduce CVC-associated infection. It is important that the critical care practitioner be proficient in the techniques of central venous catheterization.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
References
- 1.Raad I, Hanna H, Maki D. Intravascular catheter-related infections: advances in diagnosis, prevention, and management. Lancet Infect Dis. 2007;7:645–57. doi: 10.1016/S1473-3099(07)70235-9. [DOI] [PubMed] [Google Scholar]
- 2.Frasca D, Dahyot-Fizelier C, Mimoz O. Prevention of central venous catheter-related infection in the intensive care unit. Crit Care. 2010;14:212. doi: 10.1186/cc8853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;49:1. doi: 10.1086/599376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355:2725–32. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- 5.Richet H, Hubert B, Nitemberg G, Andremont A, Buu-Hoi A, Ourbak P, et al. Prospective multicenter study of vascular-catheter–related complications and risk factors for positive central catheter cultures in intensive care unit patients. J Clin Microbial. 1990;28:2520–5. doi: 10.1128/jcm.28.11.2520-2525.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maki DG, Weise CE, Saratin HW. A semiquantitative culture method for identifying intravenous catheter related infection. N Eng J Med. 1977;296:1305–9. doi: 10.1056/NEJM197706092962301. [DOI] [PubMed] [Google Scholar]
- 7.O’Grady NP, Alexander M, Dellinger EP, Gerberding JL, Heard SO, Maki DG, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2002;35:1281–307. [Google Scholar]
- 8.Koneman EW, Allen SD, Janda WM, Schreckenberger PC, Winn WC., Jr . The gram-positive cocci. I. Staphylococci and related organisms. In Color atlas and textbook of diagnostic microbiology. 5th ed. Philadelphia, PA: Lippincott/ The Williams and Wilkins Co; 1997. pp. 539–76. [Google Scholar]
- 9.Performance standards for antimicrobial susceptibility testing. Twelfth informational supplement. Wayne PA: M100-S12 NCCLS; 2002. National committee for clinical laboratory standards. [Google Scholar]
- 10.Miles RS, Amyes SG. Laboratory control of antimicrobial therapy. In: Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie and McCartney Practical Medical Microbiology. 14th ed. Vol. 2. London: Churchill Livingstone; 1996. pp. 151–78. [Google Scholar]
- 11.Widmer AF, Nettleman M, Flint K, Wenzel RP. The clinical impact of culturing central venous catheters. Arch Intern Med. 1992;152:1299–302. [PubMed] [Google Scholar]
- 12.Haslett TM, Isenberg HD, Hilton E, Tucci V, Kay BG, Vellozzi EM. Microbiology of indwelling central intravascular catheters. J Clin Microbiol. 1988;26:696–701. doi: 10.1128/jcm.26.4.696-701.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Groeger JS, Lucas AB, Thaler HT, Friedlander-Klar H, Brown AE, Kiehn TE, et al. Infectious morbidity associated with long term use of venous access devices in patients with cancer. Ann Intern Med. 1993;119:1168–74. doi: 10.7326/0003-4819-119-12-199312150-00003. [DOI] [PubMed] [Google Scholar]
- 14.Pemberton LB, Ross V, Cuddy P, Kremer H, Fessler T, McGurk E. No difference in catheter sepsis between standard and antiseptic central venous catheters. Arch Surg. 1996;131:986–9. doi: 10.1001/archsurg.1996.01430210084018. [DOI] [PubMed] [Google Scholar]
- 15.Safdar N, Maki DG. The pathogenesis of catheter-related bloodstream infection with noncuffed short-term central venous catheters. Intensive Care Med. 2004;30:62–7. doi: 10.1007/s00134-003-2045-z. [DOI] [PubMed] [Google Scholar]
- 16.Trick WE, Miranda J, Evans AT, Charles-Damte M, Reilly BM, Clarke P. Prospective cohort study of central venous catheters among internal medicine ward patients. Am J Infect Control. 2006;34:636–41. doi: 10.1016/j.ajic.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 17.LeMaster CH, Schuur JD, Pandya D, Pallin DJ, Silvia J, Yokoe D, et al. Infection and natural history of emergency department-placed central venous catheters. Ann Emerg Med. 2010;56:492–7. doi: 10.1016/j.annemergmed.2010.05.033. [DOI] [PubMed] [Google Scholar]
- 18.Lemaster CH, Agrawal AT, Hou P, Schuur JD. Systematic review of emergency department central venous and arterial catheter infection. Int J Emerg Med. 2010;3:409–23. doi: 10.1007/s12245-010-0225-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koh DB, Gowardman JR, Rickard CM, Robertson IK, Brown A. Prospective study of peripheral arterial catheter infection and comparison with concurrently sited central venous catheters. Crit Care Med. 2008;36:397–402. doi: 10.1097/CCM.0b013e318161f74b. [DOI] [PubMed] [Google Scholar]
- 20.Lucet JC, Bouadma L, Zahar JR, Schwebel C, Geffroy A, Pease S, et al. Infectious risk associated with arterial catheters compared with central venous catheters. Crit Care Med. 2010;38:1030–5. doi: 10.1097/CCM.0b013e3181d4502e. [DOI] [PubMed] [Google Scholar]
- 21.Fortún J, Perez-Molina JA, Asensio A, Calderón C, Casado JL, Mir N, et al. Semiquantitative culture of subcutaneous segment for conservative diagnosis of intravascular catheter related infection. JPEN J Parenter Enteral Nutr. 2000;24:210–4. doi: 10.1177/0148607100024004210. [DOI] [PubMed] [Google Scholar]
- 22.Deshpande KS, Hatem C, Ulrich HL, Currie BP, Aldrich TK, Bryan-Brown CW, et al. The incidence of infectious complications of central venous catheters at the subclavian, internal jugular and femoral sites in an intensive care unit population. Crit Care Med. 2005;33:13–20. doi: 10.1097/01.ccm.0000149838.47048.60. discussion 234-5. [DOI] [PubMed] [Google Scholar]
- 23.Cobb DK, High KP, Sawyer RG, Sable CA, Adams RB, Lindley DA, et al. A controlled trial of scheduled replacement of central venous and pulmonary-artery catheters. N Engl J Med. 1992;327:1062–8. doi: 10.1056/NEJM199210083271505. [DOI] [PubMed] [Google Scholar]
- 24.Charalambous C, Swoboda SM, Dick J, Perl T, Lipsett PA. Risk factors and clinical impact of central line infections in the surgical intensive care unit. Arch Surg. 1998;133:1241–6. doi: 10.1001/archsurg.133.11.1241. [DOI] [PubMed] [Google Scholar]
- 25.Juste RN, Hannan M, Glendenning A, Azadin B, Soni N. Central venous blood culture: a useful test for catheter colonisation? Intensive Care Med. 2000;26:1373–5. doi: 10.1007/s001340000582. [DOI] [PubMed] [Google Scholar]
- 26.Aufwerber E, Ringertz S, Ransjo U. Routine semiquantitative cultures and central venous catheter related bacteremia. APMIS. 1991;99:627–30. doi: 10.1111/j.1699-0463.1991.tb01237.x. [DOI] [PubMed] [Google Scholar]
- 27.Mermel LA, Farr BM, Sherertz RJ, Raad II, O’Grady N, Harris JS, et al. Guidelines for the management of intravascular catheter – related infections. Clin Infect Dis. 2001;32:1249–72. doi: 10.1086/320001. [DOI] [PubMed] [Google Scholar]
- 28.Maki DG, Ringer M, Alvarado CJ. Prospective randomized trial of povidone-iodine, alcohol, and chlorhexidine for prevention of infection associated with central venous and arterial catheters. Lancet. 1991;338:339–43. doi: 10.1016/0140-6736(91)90479-9. [DOI] [PubMed] [Google Scholar]
- 29.Mimoz O, Pieroni L, Lawrence C, Edouard A, Costa Y, Samii K, et al. Prospective, randomized trial of two antiseptic solutions for prevention of central venous or arterial catheter colonization and infection in intensive care unit patients. Crit Care Med. 1996;24:1818–23. doi: 10.1097/00003246-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Moonens F, el Alami S, Van Gossum A, Struelens MJ, Serruys E. Usefulness of gram staining of blood collected from total parenteral nutrition catheter for rapid diagnosis of catheter related sepsis. J Clin Microbiol. 1994;32:1578–9. doi: 10.1128/jcm.32.6.1578-1579.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Velasco E, Thuler LC, Martins CA, Nucci M, Dias LM, Gonçalves VM, et al. Epidemiology of bloodstream infections at a cancer center. Sao Paulo Med J. 2000;118:131–8. doi: 10.1590/S1516-31802000000500004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Snydman DR, Gorbea HF, Pober BR, Majka JA, Murray SA, Perry LK. Predictive value of surveillance skin cultures in total parenteral nutrition-related infection. Lancet. 1982;18:1385–8. doi: 10.1016/s0140-6736(82)91281-8. [DOI] [PubMed] [Google Scholar]
- 33.Schwaber MJ, Krasner CN, Gold HS, Venkataraman L, Avigan DE, Karchmer AW, et al. Detection of Staphylococcus aureus in peripheral blood stem cell cultures after sterilization of standard blood cultures. J Clin Apher. 2003;1:37–9. doi: 10.1002/jca.10046. [DOI] [PubMed] [Google Scholar]
- 34.Bozzetti F, Terno G, Camerini E, Baticci F, Scarpo D, Pupa A. Pathogenesis and predictability of central venous catheter related sepsis. Surgery. 1982;91:383–9. [PubMed] [Google Scholar]
- 35.Winston DJ, Dudnick DV, Chapin M, Ho WG, Gale RP, Martin WJ. Coagulase-negative staphylococcal bacteremia in patients receiving immunosuppressive therapy. Arch Intern Med. 1983;143:32–6. [PubMed] [Google Scholar]
- 36.Kloos WE, Bannerman TL. Update of clinical significance of coagulase negative staphylococci. Clin Microbiol Rev. 1994;7:117–40. doi: 10.1128/cmr.7.1.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lorente L, Henry C, Martín MM, Jiménez A, Mora ML. Central venous catheter-related infection in a prospective and observational study of 2,595 catheters. Crit Care. 2005;9:R631–5. doi: 10.1186/cc3824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kemp L, Burge J, Choban P, Harden J, Mirtallo J, Flancbaum L. The effect of catheter type and site on infection rates in total parenteral nutrition patients. JPEN J Parenter Enteral Nutr. 1994;18:71–4. doi: 10.1177/014860719401800171. [DOI] [PubMed] [Google Scholar]
- 39.Eyer S, Brummitt C, Crossley K, Siegel R, Cerra F. Catheter related sepsis: prospective randomized trial of three methods of longterm catheter maintenance. Crit Care Med. 1990;18:1073–9. [PubMed] [Google Scholar]
- 40.Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006;81:1159–71. doi: 10.4065/81.9.1159. [DOI] [PubMed] [Google Scholar]
- 41.McGee WT, Ackerman BL, Rouben LR, Prasad VM, Bandi V, Mallory DL. Accurate placement of central venous catheters: a prospective randomized, multicentre trial. Crit care Med. 1993;21:1118–23. doi: 10.1097/00003246-199308000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Safdar N, Kluger DM, Maki DG. A review of risk factors for catheter-related bloodstream infection caused by percutaneously inserted, noncuffed central venous catheters: implications for preventive strategies. Medicine (Baltimore) 2002;81:466–79. doi: 10.1097/00005792-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 43.Zhang L, Sriprakash KS, McMillan D, Gowardman JR, Patel B, Rickard CM. Microbiological pattern of arterial catheters in the intensive care unit. BMC Microbiol. 2010;19(10):266. doi: 10.1186/1471-2180-10-266. [DOI] [PMC free article] [PubMed] [Google Scholar]


