Abstract
Although relatively uncommon, fungi, atypical Mycobacteria, and Nocardia have been isolated from a variety of infections of eye including keratitis, scleritis, canaliculitis, dacryocystitis, endophthalmitis and orbital cellulites. The organisms typically cause a slowly progressive disease. The diseases caused by the organisms can pose both diagnostic and therapeutic challenges. In this manuscript we will describe updates on important aspects of the ocular infections caused by these organisms.
Keywords: fungi, non-tubercular Mycobacteria, Nocardia, keratitis, scleritis, endophthalmitis
Introduction
Infectious diseases of the eye have long been recognized as important causes of blindness. While Chlamydia trachomatis, Neisseria gonorrhoea, and Onchocerca volvulus are important causes of global blindness,1, 2 many other organisms can cause serious ocular morbidity. Although relatively uncommon, ocular infections caused by fungi, atypical Mycobacteria, and Nocardia can pose both diagnostic and therapeutic challenges. In this manuscript we will describe updates on important aspects of the ocular infections caused by these organisms.
Fungal infections of the eye
Although fungi are recognized as opportunistic pathogens, ocular fungal infections or ophthalmic mycoses are being increasingly recognized as important causes of morbidity and blindness, especially in tropical countries.3, 4, 5 An overwhelming number of fungal genera and species have been implicated as causes of ophthalmic mycoses, and this number is steadily increasing. Table 1 highlights some of the important genera and species isolated from various ophthalmic mycoses cases.
Table 1. Important fungi isolated from ocular infections.
| Fungi group | Fungal genus and species | Important ocular diseases |
|---|---|---|
| Hyaline filamentous | Fusarium (F. solani, F. dimerum, F. oxysporum) | Keratitis, scleritis, endophthalmitis |
| Aspergillus (A. fumingatus, A. terrus, A. terreus) | Keratitis, scleritis, endophthalmitis, oribital cellulitis Dacryocystitis | |
| Scedosporium (S. apiospermum, S. prolificanc) | Keratitis, scleritis, endophthalmitis Orbital cellulitis | |
| Paecilomyces (P. lilacinus, P. variotii) | Keratitis, endophthalmitis | |
| Acremonium (A. kilience, A. potronii) | Keratitis, endophthalmitis | |
| Dematiaceous | Bipolaris (B. specifera, B. hawaiiensis) | Keratitis, scleritis |
| Curvularia (C. lunata, C. geniculata) | Keratitis, scleritis | |
| Exserohilum (E. rostratum) | Keratitis, scleritis | |
| Exophiala (E. dermatitidis) | Keratitis, scleritis | |
| Lasiodiplodia theobromae | Keratitis | |
| Yeasts and zygomycetes | ||
| Yeasts | Candida (C. albicans, C. parapsilosis, C.guilliermondii) | Keratitis, infectious crystalline keratopathy, scleritis, endophthalmitis, orbital cellulitis |
| Cryptococcus (C. neoformans, C. laurentii) | Keratitis, blepharitis, endophthalmitis | |
| Zygomycetes | Rhizopus, Mucor, Rhizomucor | Orbital cellulitis, scleritis |
| Thermally dimorphic fungi | Paracoccidioides brasiliensis, Blastomyces dermatitidis, Sporothrix schenckii Histoplasma capsulatum | Eye lid infection, conjunctivitis, keratitis, endophthalmitis |
Keratitis
Keratitis is by far the most frequent fungal infection of eye.3, 4 Trauma is the most important predisposing factor.5 Other predisposing factors include corneal surgery, prolonged use of corticosteroids or antibiotics, pre-existing ocular diseases, systemic diseases such as diabetes mellitus, and contact lenses.3, 4, 6, 7
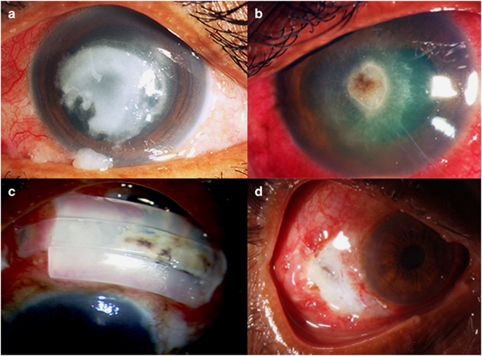
Fungi produce a slowly progressive disease characterized by localized infiltrate. Classical clinical features are shown in Figures 1a and b.
Figure 1.
Fungal infections of eye. (a) Shows fungal keratitis with dry gray to dirty white infiltrate and raised edges. (b) Shows keratitis with pigmented infiltrate. (c) Shows pigmented fungal growth on the surface of scleral buckle in a case of fungal scleritis. (d) Shows ulcerated scleritis lesion.
Although several features are characteristic, not all patients present with these features. Ring infiltrate mimicking acanthamoeba or frank suppuration mimicking bacterial keratitis or dendritic lesions, and even mutton fat endothelial lesions mimicking HSV endothelitis are not uncommon presentations in fungal keratitis. Further, non-fungal microorganisms such as acanthamoeba, nocardia and Gram-positive bacteria can present with clinical features resembling fungal infection.8, 9 Therefore, no clinical feature can be considered absolutely pathognomonic of fungal aetiology.10
Challenges with laboratory diagnosis
Although microscopic examination of smear using various stain and inoculation on culture media helps in identification of fungal infections, laboratory diagnosis can be challenging, especially in patients with deep-seated keratitis. In such cases, corneal biopsy helps to establish the diagnosis.11 Although this technique allows direct visualization of organisms, it has limitation of being less sensitive, involving tissue destruction and having a high sampling error. Confocal microscopy, a non-invasive, in-vivo technique for examination of cornea, offers an alternative and has been found to be useful in diagnosis of fungal and acanthamoeba infections.12 However, the technique is not without limitations; besides the cost of the instrument, it is not easy to get good-quality images in painful inflamed eyes, and experience is required for interpretation of images.13, 14
Therapeutic challenges
Fungal keratitis cases pose several therapeutic challenges. Only limited numbers of drugs are commercially available for ophthalmic use. Most of the drugs are fungistatic, have limited spectrum of activity, and have poor penetration through ocular structures. Therefore, medical treatment fails to control infection in a significant proportion of cases.15 Some of the new molecules investigated in recent past include azoles (voriconazole and posaconazole) and eccinocanidines (caspofungin and micafungin).16, 17 While the pharmacological properties, in-vitro susceptibility, as well as the anecdotal reports suggest superiority of voriconazole over other antifungal agents,16 a randomized clinical trail in South India comparing natamycin with voriconazole in treatment of mycotic keratitis did not find any difference in the scar size, visual acuity, and perforation rate.18 Therefore, more clinical trials are required to provide rigorous evidence basis to guide using these molecules.
Can we increase drug concentration at the site of infection?
As penetration into ocular tissues is a major limiting factor, attempts have been made to push the antifungal drugs directly into the site of infection. The group from the Bascom Palmer Eye Institute (BPEI) used iontophoresis to deliver amphotericin B into the corneal stroma.19 More recently, clinicians have tried intrastromal injection of water-soluble molecules such as amphotericin B and voriconazole. Sharma et al20 published a case series demonstrating the successful use of this technique in the management of recalcitrant keratitis. However, another approach worth exploring will be the use of nanotechnology. As the technology allows regulated release of drugs, it prolongs the antifungal activity.
Surgical treatment
Lessons learnt from understanding of distribution of fungal filaments in corneal tissues can help us improve the management of fungal keratitis. In two separate studies, we found that fungal filaments can be located entirely into anterior stroma (39%), especially in patients with plaque-like infiltrate,21, 22 and superficial keratectomy will help in management by reducing the fungal load in such cases.
Xie et al23 published successful management of fungal keratitis by deep anterior lamellar keratoplasty in a large series of cases. However, we need to exercise caution in patients with advanced keratitis, as fungal filaments were found to penetrate Descemet's membrane in 61.5% specimens from advanced keratitis cases (unpublished data).
Although penetrating keratoplasty seems to be a better option in patients with deep keratitis, the procedure is associated with several challenges.24 It is not surprising that 35% of the keratoplasty procedures performed for active fungal keratitis fail within the first month and 50% by the end of first year.25
Scleritis
Fungi are important aetiological agents of infective scleritis in tropical regions.26, 27 In a report published by us, 38% cases of infective scleritis were caused by fungi.26 The fungal infection of sclera commonly occurs following accidental trauma or following variety of surgical procedures, but can also occur as an extension from cornea or choroid and rarely as an endogenous infection.27
Fungal scleritis usually presents as slowly progressive scleral necrosis with suppuration. Figures 1c and d document various features of fungal scleritis.
The diagnosis of fungal scleritis is often delayed because the disease in initial stage appears identical to that caused by immune-mediated disease. Further, as the organisms lie deep in the stroma, negative microbiology is not rare in these cases. The outcome of medical therapy alone is usually poor due to poor penetration of topical and systemic antifungal agents into avascular sclera.
It is therefore important to:
Consider infective aetiology in differential diagnosis of all cases of suppurative scleritis, especially if there is history of accidental or surgical trauma or debilitating systemic disease.
Remember that the negative microbiology does not rule out infection. Such cases should be subjected to scleral biopsy.
Combine medical management with surgical intervention involving excision of overlying conjunctiva, Tenon's capsule and necrotic sclera, and debridement of the ulcer base.
Continue antifungal treatment for a long time after clinical resolution to take care of viable fungi that can still be found in tissues after presumed cure.
Remove buckling elements and sutures along with thorough debridement of any white deposits from underlying sclera and irrigation with 5% povidone iodine in patients with buckle infection.
Endophthalmitis
Fungi have been isolated from cases of both exogenous and endogenous endophthalmitis.28, 29, 30, 31 Similar to keratitis and scleritis, fungal endophthalmitis poses diagnostic and therapeutic challenges. Although classically described to have longer latency compared with bacterial infection, many reports on fungal endophthalmitis have described infection developing within 4 days of inoculation.30, 31 The clinical picture is variable, and depending on the virulence can resemble bacterial endophthalmitis. The variable presentation coupled with lack of clinical suspicion results in delayed diagnosis in many cases. To avoid this, ophthalmologists should consider fungal aetiology in post-trauma or post-cataract surgery infections in geographic areas where fungal infections are common.
Another important aspect in diagnosis of endophthalmitis is submitting appropriate sample for microbiology. Traditionally, vitreous aspirate is believed to be more sensitive than an anterior chamber aspirate. In the study from BPEI, six cases with positive anterior chamber aspirate results had negative vitreous culture results.31 This was attributed to the primary location of the infection. Furthermore, some fungi may be less capable of penetrating the vitreous cavity. Therefore, whenever possible, both anterior chamber and vitreous aspirates should be submitted for a complete endophthalmitis evaluation.
The management of fungal endophthalmitis primarily comprises of vitrectomy and intravitreal injection of antifungal drugs. Traditionally, amphotericin B has been the preferred antifungal agent for intraocular injection. More recently, the use of voriconazole is gaining popularity.31 Intracameral injection of antifungal agents can be considered when the intraocular infection primarily involves the anterior chamber. One must also remember that patients with fungal endophthalmitis often require multiple intraocular injections. However, there are no definitive protocols to guide repeat injections, and more studies are needed to determine the optimal antifungal regimen.
Atypical mycobacteria and the eye
Atypical mycobacteria, also known as nontuberculous mycobacteria (NTM), are aerobic, non-motile, non-spore forming bacilli, and have been isolated from a wide variety of ocular infections including keratitis, scleritis, canaliculitis, dacryocystitis, orbital cellulitis, uveitis, and endophthalmitis.32, 33, 34, 35 The vast majority of ocular infections are caused by the Runyon group IV organisms M. fortuitum, and M. chelonae. The other less common organisms include M. sulzi, M. flavescens, M. avium-intracellulare, M. gordonae, and M. marinum.36, 37, 38
Keratitis remains the most common ocular infection of NTMs.32, 33 On the basis of the experience with the 35 cases managed at the LV Prasad Eye Institute and by review of the literature, it is evident that trauma and the metallic corneal foreign body in particular are the most common predisposing factors. The infection has also been reported following a variety of surgical procedures including cataract and refractive surgery.39, 40, 41, 42
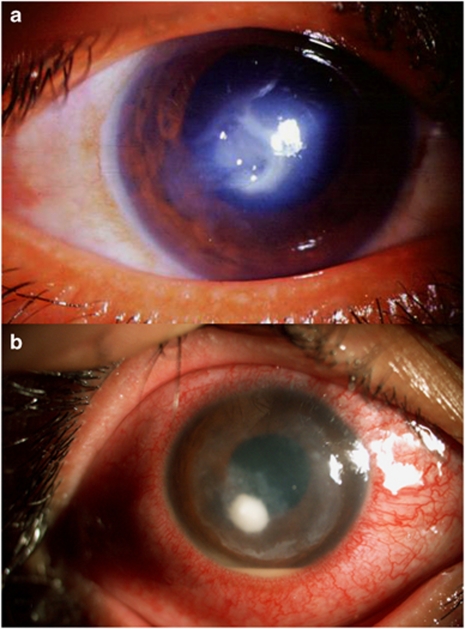
One of the characteristic features of NTM keratitis is the delay in the onset of clinical disease after corneal trauma. The disease presents with a broad spectrum of clinical features including cracked windshield appearance, ring infiltrate, satellite lesions, and infectious crystalline keratopathy. In our series, all patients presented with central or paracentral localized infiltrate extending for a variable depth of stroma (Figure 2).
Figure 2.
Non-tubercular mycobacteria keratitis after accidental trauma (a) and laser in-situ keratomileusis (b).
Although there was no case in the series published by us,28 NTMs have been isolated from few cases of scleritis.34, 38 The clinical picture in NTM scleritis is indistinguishable from fungal infection.
NTMs have also been isolated from both endogenous35, 43 and exogenous endophthalmitis cases including postoperative endophthalmitis.38, 44, 45, 46 The most characteristic sign of NTM endophthalmitis following cataract surgery is multiple white plaques between intraocular lens and posterior capsule or on the anterior hyaloid face mimicking P. acne endophthalmitis.
The diagnosis of NTM infection poses several challenges. The diagnosis is often delayed primarily because it being rare, the clinicians do not consider it in differential diagnosis. The clinical picture mimics the infections caused by other low-virulent bacteria and fungi. Further, the organisms stain poorly on routine screening dyes or are seen as partially stained bacilli.47 Furthermore, although the members of Runyon group IV produce positive cultures within 7 days, the infection caused by slow growers is likely to be missed on routine microbiology as culture plates are often discarded after 7 days. Therefore, the diagnosis of NTM infection depends to a large extent on the clinicians' vigilance. In all the suspected cases, they should order specific stains such as the Ziehl–Neelsen acid fast stain and culture on specific media such as the Lowenstein–Jensen media.
Treatment of NTM ocular infections is also challenging. In vitro antimicrobial susceptibility studies uniformly suggest amikacin clarithromycin and azithromycin to be the best drugs in its management. There is an interest in the use of fluoroquinolones, both for prophylaxis and treatment. The results of susceptibility test including minimum inhibitory concentrations show that fluoroquinolones, including the fourth-generation ones, are unlikely to be useful for this infection.48 Despite the use of sensitive antibiotics, several patients of NTM infection do not respond to medical treatment and require surgical intervention.
Nocardia and the eye
Nocardia organisms and mycobacteria belong to the same bacterial order Actinomycetales; they exhibit similarities with respect to cell wall antigens and bacteriophage susceptibility. These are, however, differentiated by staining characteristics, morphology, and the lipid composition of cell wall. Although the organisms are known to cause pulmonary infections in immunocompromised individuals, these are also identified as rare but important cause of ocular infections.
Various infections caused by these organisms include—keratitis,9 scleritis,9, 26 conjunctivitis, canaliculitis, dacryocystitis, orbital cellulitis, and endophthalmitis.9
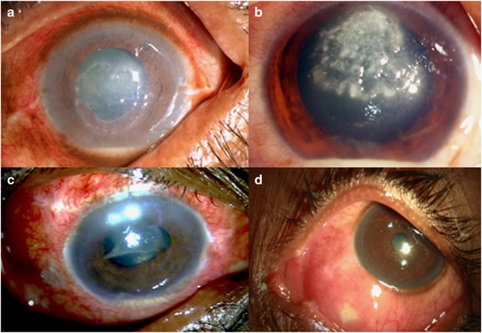
Corneal infection is by far the most common ocular infection caused by Nocardia and is reported after accidental and surgical trauma including refractive surgery.9, 49, 50 The clinical picture is characterized by a relatively slow and recalcitrant keratitis with mean time to presentation 24.5±22.2 days in our series. Figure 3 shows various corneal pictures of this infection. Patchy anterior stromal infiltrates with yellow-white pin-head-sized raised calcareous lesions arranged in a wreath pattern is the most characteristic feature of this infection. However, this classical clinical picture is not seen in post-surgery infections and in advanced keratitis cases. Nocardia are the second most common cause of infectious scleritis in Southern India.26 The predisposing factors and clinical picture of Nocardia scleritis are almost similar to that of fungal and NTM scleritis.
Figure 3.
Nocardia infections of eye. (a) Shows nocardia keratitis with characteristic wreath-like lesion. (b) Shows a case of advanced keratitis with dry-looking infiltrate mimicking fungal infection. (c) Shows nocardia keratitis with suppurative lesion. (d) Shows suppurative nodular scleritis.
Nocardia are isolated from cases of both exogenous and endogenous endophthalmitis.9, 51 A large number of these cases are reported from South India.9, 51, 52 Similar to keratitis and scleritis, the organism produces a slow insidious disease; the mean time to presentation from symptom onset was 21.5±20.6 days and the mean duration from surgery to presentation was 47.5±49.4 days in our series.9 The clinical picture is characterized by distinctive anterior chamber findings such as the exudates on corneal endothelium or nodule-like deposits at the pupillary border in significant number of patients. These intense anterior segment findings are coupled with minimal vitritis or posterior segment findings.9, 51, 52 Cases with advanced endophthalmitis present with white fluffy exudates on posterior capsule and anterior vitreous mimicking fungal endophthalmitis. The clinical presentation in endogenous endophthalmitis is much different than exogenous endophthalmitis and is characterized by large choroidal lesions with overlying haemorrhages.
In contrast to NTM, the diagnosis of Nocardia infection of cornea is usually straightforward. In our series, the diagnosis was suspected in 45% patients at the first visit, based on the characteristic corneal infiltrate. In contrast, nocardia scleritis and endophthalmitis resembles closely with fungal and NTM infections. Even in these cases, microscopic examination of ocular specimen using Gram stain as well as 1% acid-fast stain (81.1% of cases in our series) facilitates early diagnosis. The organisms are not fastidious and grow on routine culture media, although bit slowly.
While identification of organism to the genus level is easy, speciation is often difficult using standard microbiology protocols. We subjected 19 isolates identified as Nocardia species on routine biochemical tests to identification by gene sequencing of 16S rRNA gene. We identified eight isolates that have never been reported in ocular infections.53 On the basis of this experience, we concluded that time has come when we should use molecule methods for the precise identification of microorganisms.
Treatment
The Nocardia organisms show a good susceptibility to amikacin and sulphonamides.53, 54 Other aminoglycosides such as gentamicin and tobramycin are the next best options in the treatment of this infection. The susceptibility to fluoroquinolones is variable. Although keratitis and scleritis cases respond very well to amikacin therapy, the outcome of endophthalmitis management is not encouraging.
Conclusion
Fungi, atypical Mycobacteria, and Nocardia are rare but important causes of ocular infections. The infection caused by these organisms poses several diagnostic and therapeutic challenges. A high degree of clinical suspicion, with appropriate diagnostic tests will help early diagnosis and institution of appropriate therapy.
The authors declare no conflict of interest.
Footnotes
This work was presented at the Cambridge Ophthalmological Symposium.
References
- Thylefors B, Negrel AD, Pararajasegaram R, Dadzie KY. Global data on blindness. Bull WHO. 1995;73:115–121. [PMC free article] [PubMed] [Google Scholar]
- Congdon NG, Friedman DS, Lietman T. Important causes of visual impairment in the world today. JAMA. 2003;290:2057–2060. doi: 10.1001/jama.290.15.2057. [DOI] [PubMed] [Google Scholar]
- Thomas PA. Current perspectives on ophthalmic mycoses. Clin Microbiol Rev. 2003;16:730–797. doi: 10.1128/CMR.16.4.730-797.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkanci A, Ozdek S. Ocular fungal infections. Curr Eye Res. 2011;36:179–189. doi: 10.3109/02713683.2010.533810. [DOI] [PubMed] [Google Scholar]
- Gopinathan U, Sharma S, Garg P, Rao GN. Review of epidemiological features, microbiological diagnosis and treatment outcome of microbial keratitis: experience of over a decade. Indian J Ophthalmol. 2009;57:273–279. doi: 10.4103/0301-4738.53051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopinathan U, Garg P, Fernandes M, Sharma S, Athmnathan S, Rao GN. The epidemiological features and laboratory results of fungal keratitis: a 10-year review. Cornea. 2002;21:555–559. doi: 10.1097/00003226-200208000-00004. [DOI] [PubMed] [Google Scholar]
- Khor W, Aung T, Saw S, Wong T, Tambyah PA, Tan AL, et al. An outbreak of Fusarium keratitis associated with contact lens wear in Singapore. JAMA. 2006;295:2867–2873. doi: 10.1001/jama.295.24.2867. [DOI] [PubMed] [Google Scholar]
- Sahu SK, Das S, Sharma S, Vemuganti GK. Acanthamoeba keratitis presenting as a plaque. Cornea. 2008;27:1066–1067. doi: 10.1097/ICO.0b013e318174dbe6. [DOI] [PubMed] [Google Scholar]
- Decroos FC, Garg P, Reddy AK, Sharma A, Krishnaiah S, Mungale M, et al. Hyderabad Endophthalmitis Research Group Optimizing diagnosis and management of nocardia keratitis, scleritis, and endophthalmitis: 11-year microbial and clinical overview. Ophthalmology. 2011;118:1193–1200. doi: 10.1016/j.ophtha.2010.10.037. [DOI] [PubMed] [Google Scholar]
- Thomas PA, Leck AK, Myatt M. Characteristic clinical features as an aid to the diagnosis of suppurative keratitis caused by filamentous fungi. Br J Ophthalmol. 2005;89:1554–1558. doi: 10.1136/bjo.2005.076315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexandrakis G, Haimovici R, Miller D, Alfonso EC. Corneal biopsy in the management of progressive microbial keratitis. Am J Ophthalmol. 2000;129:571–576. doi: 10.1016/s0002-9394(99)00449-3. [DOI] [PubMed] [Google Scholar]
- Kaufman SC, Musch DC, Belin MW, Cohen EJ, Meisler DM, Reinhart WJ, et al. Confocal microscopy: a report by the American Academy of Ophthalmology. Ophthalmology. 2004;111:396–406. doi: 10.1016/j.ophtha.2003.12.002. [DOI] [PubMed] [Google Scholar]
- Hau SC, Dart JKG, Vesaluoma M, Parmar DN, Claerhout I, Bibi K, et al. Diagnostic accuracy of microbial keratitis with in vivo scanning laser confocal microscopy. Br J Ophthalmol. 2010;94:982–987. doi: 10.1136/bjo.2009.175083. [DOI] [PubMed] [Google Scholar]
- Garg P. Diagnosis of microbial keratitis. Br J Ophthalmol. 2010;94:961–962. doi: 10.1136/bjo.2010.182550. [DOI] [PubMed] [Google Scholar]
- Lalitha P, Prajna NV, Kabra A, Mahadevan K, Srinivasan M. Risk factors for treatment outcome in fungal keratitis. Ophthalmology. 2006;113:526–530. doi: 10.1016/j.ophtha.2005.10.063. [DOI] [PubMed] [Google Scholar]
- Hariprasad SM, Mieler WF, Lin TK, Sponsel WE, Graybill JR. Voriconazole in the treatment of fungal eye infections: a review of current literature. Br J Ophthalmol. 2008;92:871–878. doi: 10.1136/bjo.2007.136515. [DOI] [PubMed] [Google Scholar]
- Hurtado-Sarrió M, Duch-Samper A, Cisneros-Lanuza A, Díaz-Llopis M, Peman-Garcíia J, Vazquez-Polo A. Successful topical application of caspofungin in the treatment of fungal keratitis refractory to voriconazole. Arch Ophthalmol. 2010;128:941–942. doi: 10.1001/archophthalmol.2010.110. [DOI] [PubMed] [Google Scholar]
- Prajna NV, Mascarenhas J, Krishnan T, Reddy PR, Prajna L, Srinivasan M, et al. Comparison of natamycin and voriconazole for the treatment of fungal keratitis. Arch Ophthalmol. 2010;128:672–678. doi: 10.1001/archophthalmol.2010.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo SH, Dursun D, Dubovy S, Miller D, Alfonso E, Forster RK, et al. Lontophoresis for the treatment of paecilomyces keratitis. Cornea. 2002;21:131–132. doi: 10.1097/00003226-200201000-00029. [DOI] [PubMed] [Google Scholar]
- Sharma N, Agarwal P, Sinha R, Titiyal JS, Velpandian T, Vajpayee RB. Evaluation of intrastromal voriconazole injection in recalcitrant deep fungal keratitis: case series. Br J Ophthalmol. 2011;95:1735–1737. doi: 10.1136/bjo.2010.192815. [DOI] [PubMed] [Google Scholar]
- Vemuganti GK, Garg P, Gopinathan U, Naduvilath TJ, Buddi R, Rao GN. Evaluation of agent and host factors in progression of mycotic ketatitis: a histological and microbiological study of 167 corneal buttons. Ophthalmology. 2002;109:1538–1546. doi: 10.1016/s0161-6420(02)01088-6. [DOI] [PubMed] [Google Scholar]
- Garg P, Vemuganti GK, Chaterjee S, Gopinathan U, Rao GN. Pigmented plaque presentation of dematiaceous fungal keratitis: a clinicopathologic correlation. Cornea. 2004;23:571–576. doi: 10.1097/01.ico.0000126318.90271.3c. [DOI] [PubMed] [Google Scholar]
- Xie L, Zhai H, Shi W, Zhao J, Sun S, Zang X. Hyphal growth pattern and recurrence of fungal keratitis after lamellar keratoplasty. Ophthalmology. 2008;115:983–987. doi: 10.1016/j.ophtha.2007.07.034. [DOI] [PubMed] [Google Scholar]
- Sharma N, Sachdev R, Jhanji V, Titiyal JS, Vajpayee RB. Therapeutic keratoplasty for microbial keratitis. Curr Opin Ophthalmol. 2010;21:293–300. doi: 10.1097/ICU.0b013e32833a8e23. [DOI] [PubMed] [Google Scholar]
- Chen WL, Wu CY, Hu FR, Wang IJ. Therapeutic penetrating keratoplasty for microbial keratitis in Taiwan from 1987 to 2001. Am J Ophthalmol. 2004;137:736–743. doi: 10.1016/j.ajo.2003.11.010. [DOI] [PubMed] [Google Scholar]
- Jain V, Garg P, Sharma S. Microbial scleritis-experience from a developing country. Eye. 2009;23:255–261. doi: 10.1038/sj.eye.6703099. [DOI] [PubMed] [Google Scholar]
- Alfonso EC, Forster RK, Garg P, Sharma S.Fungal infectionsIn: Foster CS, Azar DT, Dohlman CH (eds).Smolin and Thoft's The Cornea: Scientific Foundations and Clinical Practice4th ed.Lippincott Williams & Wilkins: Philadelphia; 2005405–425. [Google Scholar]
- Montan P. Endophthalmitis. Curr Opin Ophthalmol. 2001;12:75–81. doi: 10.1097/00055735-200102000-00013. [DOI] [PubMed] [Google Scholar]
- Smith SR, Kroll AJ, Lou PL, Ryan EA. Endogenous bacterial and fungal endophthalmitis. Int Ophthalmol Clin. 2007;47:173–183. doi: 10.1097/IIO.0b013e31803778f7. [DOI] [PubMed] [Google Scholar]
- Chakrabarti A, Shivaprakash MR, Singh R, Tarai B, George VK, Fomda BA, et al. Fungal endophthalmitis: fourteen years' experience from a center in India. Retina. 2008;28:1400–1407. doi: 10.1097/iae.0b013e318185e943. [DOI] [PubMed] [Google Scholar]
- Wykoff CC, Flynn HW, Jr, Miller D, Scott IU, Alfonso EC.Exogenous fungal endophthalmitis: microbiology and clinical outcomes Ophthalmology 20081151501–1507.1507.e1-2. [DOI] [PubMed] [Google Scholar]
- Huang SCM, Soong HK, Chang JS, Liang YS. Non tuberculosis mycobacterial keratitis: a study of 22 cases. Br J Ophthalmol. 1996;80:962–968. doi: 10.1136/bjo.80.11.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalitha P, Rathinam SR, Srinivasan M. Ocular infections due to non-tuberculous mycobacteria. Indian J Med Microbiol. 2004;22:231–237. [PubMed] [Google Scholar]
- Rich RM, Smiddy WE, Davis JL. Infectious scleritis after retinal surgery. Am J Ophthalmol. 2008;145:695–699. doi: 10.1016/j.ajo.2007.11.024. [DOI] [PubMed] [Google Scholar]
- Matieli LCV, Freitas DE, Sampaio J, Moraes NSB, Zorat MC, Halfling-Lima AL. Mycobacterium abscessus endopthalmitis: treatment dilemma and review of literature. Retina. 2006;26:826–830. doi: 10.1097/01.iae.0000244276.80716.96. [DOI] [PubMed] [Google Scholar]
- Moore MB, Newton C, Kaufman HE. Chronic keratitis caused by Mycobacterium gordonae. Am J Ophthalmol. 1986;102:516–552. doi: 10.1016/0002-9394(86)90083-8. [DOI] [PubMed] [Google Scholar]
- Knapp A, Stern GA, Hood CI. Mycobacterium avium-intracellulare corneal ulcer. Cornea. 1987;6:175–180. doi: 10.1097/00003226-198706030-00004. [DOI] [PubMed] [Google Scholar]
- Schonherr U, Naumann GOH, Lang GK, Bialasiewicz AA. Sclerokeratitis caused by Mycobacterium marinum. Am J Ophthalmol. 1989;108:607–608. doi: 10.1016/0002-9394(89)90449-2. [DOI] [PubMed] [Google Scholar]
- Matoba AY, Torres J, Wilhelmus KR, Hamill MB, Jones DB. Bacterial keratitis after radial keratotomy. Ophthalmology. 1989;96:1171–1175. doi: 10.1016/s0161-6420(89)32761-8. [DOI] [PubMed] [Google Scholar]
- Jain V, Garg P, Sharma S, Vemuganti GK. Suture-less wound infection by unusual acid-fast organisms. Cornea. 2008;27:615–618. doi: 10.1097/ICO.0b013e318166efdf. [DOI] [PubMed] [Google Scholar]
- Garg P, Chaurasia S, Vaddavalli PK, Muralidhar R, Mittal V, Gopinathan U. Microbial keratitis after LASIK. J Refract Surg. 2010;26:209–216. doi: 10.3928/1081597X-20100224-07. [DOI] [PubMed] [Google Scholar]
- Srinivasan M, Prajana L, Prajana V. A cluster of cases of Mycobacterium chelonae keratitis following penetrating keratoplasty. Indian J Ophthalmol. 2005;53:67–68. doi: 10.4103/0301-4738.15292. [DOI] [PubMed] [Google Scholar]
- Ambler JS, Meisler DM, Zakov ZN, Hall GS, Spech TJ. Endogenous Mycobacterium chelonae endophthalmitis. Am J Ophthalmol. 1989;108:338–339. doi: 10.1016/0002-9394(89)90136-0. [DOI] [PubMed] [Google Scholar]
- Ramaswamy AA, Biswas J, Bhaskar V, Gopal L, Rajagopal R, Madhavan HN. Postoperative Mycobacterium chelonae endophthalmitis after extracapsular cataract extraction and posterior chamber intraocular lens implantation. Ophthalmology. 2000;107:1283–1286. doi: 10.1016/s0161-6420(00)00162-7. [DOI] [PubMed] [Google Scholar]
- Benz MS, Murray TG, Dubovy SR, Katz RS, Eifrig CW. Endophthalmitis caused by mycobacterium chelonae abscessus after intravitreal injection of triamcinolone. Arch Ophthalmol. 2003;121:271–273. doi: 10.1001/archopht.121.2.271. [DOI] [PubMed] [Google Scholar]
- Gedde SJ, Scott IU, Tabandeh H, Luu KK, Budenz DL, Greenfield DS, et al. Late endophthalmitis associated with glaucoma drainage implants. Ophthalmology. 2001;108:1323–1327. doi: 10.1016/s0161-6420(01)00598-x. [DOI] [PubMed] [Google Scholar]
- Garg P, Athmanathan S, Rao GN. Mycobacterium Chelonei masquerading as Corynebacterium in a case of infectious keratitis: a diagnostic dilemma. Cornea. 1998;17:230–232. doi: 10.1097/00003226-199803000-00021. [DOI] [PubMed] [Google Scholar]
- Reddy AK, Garg P, Babu KH, Gopinathan U, Sharma S. In vitro antibiotic susceptibility of rapidly growing non-tuberculous mycobacteria isolated from patients with microbial keratitis. Curr Eye Res. 2010;35:225–229. doi: 10.3109/02713680903502258. [DOI] [PubMed] [Google Scholar]
- Bharathi MJ, Ramakrishnan R, Vasu S, Meenakshi R, Chirayath A, Palaniappan R. Nocardia asteroides keratitis in South India. Indian J Med Microbiol. 2003;21:31–36. [PubMed] [Google Scholar]
- Garg P, Chaurasia S, Vaddavalli PK, Muralidhar R, Mittal V, Gopinathan U. Microbial keratitis after LASIK. J Refract Surg. 2010;26:209–216. doi: 10.3928/1081597X-20100224-07. [DOI] [PubMed] [Google Scholar]
- Ramakrishnan R, Bharathi MJ, Shivkumar C, Mittal S, Meenakshi R, Khadeer MA, et al. Microbiological profile of culture-proven cases of exogenous and endogenous endophthalmitis: a 10-year retrospective study. Eye (Lond) 2009;23:945–956. doi: 10.1038/eye.2008.197. [DOI] [PubMed] [Google Scholar]
- Lalitha P, Rajagopalan J, Prakash K, Ramasamy K, Prajna NV, Srinivasan M. Postcataract endophthalmitis in South India incidence and outcome. Ophthalmology. 2005;112:1884–1889. doi: 10.1016/j.ophtha.2005.05.020. [DOI] [PubMed] [Google Scholar]
- Reddy AK, Garg P, Kaur I. Speciation and susceptibility of Nocardia isolated from ocular Infections. Clin Microbiol Infect. 2010;16:1168–1171. doi: 10.1111/j.1469-0691.2009.03079.x. [DOI] [PubMed] [Google Scholar]
- Lalitha P, Tiwari M, Prajna NV, Gilpin C, Prakash K, Srinivasan M. Nocardia keratitis: species, drug sensitivities, and clinical correlation. Cornea. 2007;26:255–259. doi: 10.1097/ICO.0b013e318033d853. [DOI] [PubMed] [Google Scholar]