Abstract
The past decade witnessed considerable debate over the factor structure of the Anxiety Sensitivity Index (ASI), with an eventual consensus emerging that supported a hierarchically organized factor structure. The present study attempted to replicate and examine the overall stability and utility of the hierarchical ASI factor pattern using a large sample of outpatients participating in an ongoing longitudinal study of anxiety disorders. Results supported a hierarchical factor structure for the ASI consisting of three lower-order factors measuring physical concerns, mental incapacitation concerns, and social concerns, all of which loaded significantly on a single second-order factor. Correlational analyses show good test–retest reliability and consistent patterns of intercorrelation for these factor-derived subscales across a 10-month time frame. Additional analyses provide support for the discriminant validity of the ASI subscales with regard to individuals with specific anxiety disorders. The theoretical implications of these findings for future evaluations of anxiety sensitivity are discussed.
Keywords: Anxiety sensitivity, Anxiety disorders
1. Introduction
As conceptualized by Reiss and his colleagues (Reiss, 1987; Reiss & McNally, 1985; Reiss, Peterson, Gurskey, & McNally, 1986), anxiety sensitivity (AS) refers to the fear of anxiety-related physical sensations resulting from the belief that these sensations may have potentially harmful somatic, psychological, or social consequences. An individual difference or trait variable, the concept of AS, along with the fear of anxiety more generally, has been an important aspect of many cognitive and behavioral theories of anxiety and panic (e.g. Barlow, 1988, 2001; Clark, 1986; Reiss, 1991), as well as in theoretical explanations for the development of anxiety disorders (e.g. Goldstein & Chambless, 1978; McNally, 1994). Numerous studies have also helped to illustrate empirically the role of AS in panic and other anxiety disorders (see Taylor, 1999, for a review).
The Anxiety Sensitivity Index (ASI; Reiss et al., 1986) has been one of the most widely used instruments to quantify the AS construct in empirical studies. Though intended by its developers to be a unidimensional measure of AS, several published studies factor analyzing the ASI have called into question the instrument’s factor structure. While some studies report as many as four factors in the ASI (Cox, Parker, & Swinson, 1996; Telch, Shermis, & Lucas, 1989; Wardle, Ahmed, & Hayward, 1990), several other studies found a three-factor solution (Stewart, Taylor, & Baker, 1997; Taylor, Koch, Woody, & McClean, 1996; Zinbarg, Barlow, & Brown, 1997), and at least one recent study reported a two-factor model (Cox, Enns, Walker, Kjernisted, & Pidlebury, 2001). Still other analyses of the ASI reported only a one-factor solution (Reiss et al., 1986; Sandin, Charot, & McNally, 1996; Taylor, 1996; Taylor, Koch, & Crockett, 1991; Taylor, Koch, McNally, & Crockett, 1992). These discrepant factor-analytic studies have sparked a heated debate regarding the overall structure of the AS construct and its theoretical utility (see Taylor 1995a,b; 1996; and Lilienfeld, Turner, & Jacob, 1993 and Lilienfeld, Turner, & Jacob, 1996).
More recently, however, a consensus has begun to emerge regarding the multidimensional nature of the AS construct. Typified by the work of Zinbarg et al. (1997), it now appears that the structure of the ASI is best explained by three lower order factors measuring physical concerns, mental incapacitation concerns, and social concerns, that all load on a single second-order factor of general AS. Although the goodness of fit for this hierarchical structure of the ASI has been confirmed in at least two data sets (Stewart et al., 1997; Zinbarg et al., 1997), additional independent analyses of this hierarchical model using other samples is needed to further support this position. Additionally, the acceptance of a hierarchically organized, multiple-factor solution for the ASI does raise important questions as to the construct validity and general utility of the ASI total score as employed in past studies (Lilienfeld et al., 1993; Taylor, 1996; Zinbarg et al., 1997).
Research on the structure of AS has been helpful to researchers interested in the pathology of different anxiety and mood disorders. Originally conceptualized as the key fear which differentiated people with panic disorder from other anxiety and mood disorder patients, elevated AS has been associated with the occurrence of panic attacks and the subsequent development of panic disorder in people with no history of the disorder (Schmidt, Larew, & Jackson, 1997, 1999), and with the experience of panic during panic-provocation tests (Eke & McNally, 1996; Rapee, Brown, Antony, & Barlow, 1992; Zinbarg, Brown, Barlow, & Rapee, 2001). However, studies have also found elevated AS relative to controls in patients with other anxiety disorders (for a review see Cox, Borger, & Enns, 1999). Further, patients with MDD also score higher than normal controls on the ASI, falling within the range of non-panic anxiety disorder patients (Otto, Pollack, Fava, Uccello, & Rosenbaum, 1995), and other studies have found ASI scores predictive of depressive symptoms (Schmidt et al., 1997; Taylor et al., 1997).
Studies using factor-derived subscales for the ASI have helped to shed some light on these findings. Particularly illuminating is the study by Zinbarg and colleagues comparing ASI subscale scores across anxiety disorder categories. In that study, higher scores on the physical concerns factor were found among panic and PTSD patients, elevated social concerns in patients with social phobia, and elevated mental incapacitation concerns in patients with mood disorders (Zinbarg et al., 1997). Similarly, Taylor et al. (1997) reported that, while overall ASI scores were higher in patients with panic than MDD patients, significantly elevated physical concerns and social concerns scores were found in patients with panic and significantly elevated mental incapacitation scores were associated with a diagnosis of MDD. Thus, it may be that elevated ASI scores reported in previous studies resulted from elevations in specific ASI factors. Further studies employing the factor-derived hierarchical approach to the ASI may be useful in clarifying the functional role of ASI in these specific anxiety or mood disorders, as well as to differentiate patients with specific anxiety or mood diagnoses.
In the present study, we examined the psychometric and conceptual structure of AS by analyzing the ASI in a large sample of anxiety disordered patients followed as part of the Harvard/Brown Anxiety Disorders Research Program (HARP). The current paper has two main goals. First, we attempted to replicate the hierarchical ASI factor structure reported by Zinbarg et al. (1997), following the methodology outlined in Zinbarg, Mohlman, and Hong (1999). Since HARP is a longitudinal study, we were also able to report test–retest reliability data for the ASI total and factor-derived subscale scores using data from yearly follow-ups. Second, we explored the ability of the factor-derived ASI subscales to differentiate between HARP patients with different anxiety and mood disorder diagnoses. Consistent with previous research, we hypothesized elevated physical concerns among HARP patients with panic disorder and elevated social concerns among our patients with social phobia. Participants with current MDD were expected to score higher on the mental incapacitation concerns subscale of the ASI when compared to participants without comorbid MDD.
2. Method
2.1. Participants and procedure
The present study is conducted as part of the larger Harvard/Brown Anxiety Disorders Research Program (HARP), a prospective, naturalistic, longitudinal study of the course of anxiety disorders in psychiatric outpatients. The study began in 1989 and recruited participants from 11 psychiatric practices and clinics located throughout the Boston area and central Massachusetts. At the time of study intake, all participants met Diagnostic and Statistical Manual of Mental Disorders 3rd Ed—Revised (DSM-III-R; American Psychiatric Association, 1987) diagnostic criteria for one or more of the following index anxiety disorders established by structured clinical interview employing the anxiety disorder modules of the Structured Clinical Interview for DSM-III-R Patient Version (SCID-P; Spitzer, Williams, Gibbon, & First, 1988): panic disorder with or without agoraphobia (PD or PDA), agoraphobia without a history of panic disorder (AWOPD), generalized anxiety disorder (GAD) or social phobia (SP). Other anxiety disorders that were diagnosed and followed longitudinally in HARP but are not among those disorders sufficient for inclusion in the study were posttraumatic stress disorder (PTSD), obsessive compulsive disorder (OCD), simple phobia (SIM), and anxiety disorder not otherwise specified (ADNOS). More precise descriptions of participant recruitment procedures, as well as the characteristics of the original sample can be found elsewhere (Massion, Warshaw, & Keller, 1993). Currently, participants are interviewed every 6 months and assessed as to their diagnostic status and symptom course using the Longitudinal Interval Follow-up Evaluation-Upjohn (LIFE-UP; Keller et al., 1987).
The administration of the ASI (Reiss et al., 1986) to HARP participants began in March 2000. The present study includes 206 individuals who completed the ASI one or more times and currently met DSM-III-R criteria for one or more anxiety disorders at the time of their ASI administration. Sixty-one participants completed the ASI but were not currently in episode of an anxiety disorder at the time they completed the ASI and are therefore not included in the study. Of the study participants, 7% were in episode of PD, 50% PDA, 3% AWOPD, 14% GAD, 29% SOC, 13% PTSD, 19% OCD and 29% major depression (MDD). Please note these percentages include participants with multiple diagnoses.
3. Assessment measures
3.1. Longitudinal Interval Follow-up Evaluation—Upjohn
The LIFE-UP (Keller et al., 1987) is an interviewer-administered assessment that collects detailed information on the course of anxiety disorder symptoms, psychosocial functioning, and treatment status. The LIFE-UP employs a six-point psychiatric status rating (PSR) scale to indicate the severity of psychiatric pathology. A PSR of 5 or 6 indicates the participant meets full DSM-III-R diagnostic criteria for the given disorder with low to moderate and severe functional impairment, respectively. A PSR of 2, 3 or 4 indicates the participant does not meet full DSM-III-R diagnostic criteria for the disorder, but still exhibits some symptoms to a minimal, mild or moderate degree, respectively. A PSR of 1 indicates the participant is without symptoms of the disorder. The LIFE-UP employs a ‘change point’ method to anchor participant reports of symptom levels to relevant life events such as birthdays, holidays, family vacations, etc., resulting in weekly ratings of psychiatric symptom severity. Three sub-studies have been conducted analyzing the reliability and validity of the LIFE-UP and are described in Warshaw, Keller, and Stout (1994). These studies found interrater reliability and long-term test–retest reliability for the LIFE-UP diagnostic ratings to be good to excellent for all index anxiety disorders and MDD.
3.2. Anxiety Sensitivity Index
The ASI (Reiss et al., 1986) is a 16-item self-report questionnaire designed to assess the construct of anxiety sensitivity: the dispositional tendency to fear the somatic and cognitive symptoms of anxiety due to a belief that these symptoms may be dangerous or harmful. Each item is rated on a five-point Likert scale ranging from 0 (very little) to 4 (very much). The ASI is the most widely used measure of the anxiety sensitivity construct, and the instrument’s psychometric properties and predictive validity have been well established (for reviews, see Peterson & Reiss, 1992; Peterson & Plehn, 1999).
4. Results
4.1. Exploratory and confirmatory factor analyses
As an initial step in analyzing the factor structure of the ASI, an exploratory principal components analysis was conducted. Since we were interested in testing and replicating the hierarchical model of AS reported by others (Zinbarg et al., 1997), an oblimin rotation was employed. The size of the resulting eigenvalues, in descending order, were 5.84, 1.75, 1.47, 1.00, 0.86, 0.77, 0.72, 0.56, 0.48, 0.46, 0.45, 0.39, 0.38, 0.33, 0.27 and 0.26. The three factors accounted for 36.5%, 10.9% and 9.1% of the total item variance before rotation and 30.6%, 25.9% and 14.1% of the item variance after rotation. Both the eigenvalues and the percentages of variance accounted for by the factors are notably similar to those reported by Zinbarg et al. (1997).
Table 1 shows the individual ASI items and their factor loadings. As can be seen, the items separated into relatively distinct factors tapping Physical Concerns (Factor 1), Mental Incapacitation Concerns (Factor 2), and Social Concerns (Factor 3). Only one item (‘It embarrasses me when my stomach growls’) failed to load >0.30 on any factor. Further, only one item (‘It scares me when I feel ‘shaky’’) loaded 0.30 on more than one factor. The resulting factors replicate those reported in Zinbarg et al. (1997) with nearly identical factor loadings.
Table 1.
First-order factor pattern matrix after oblimin rotation
| Item No. | Description | Factor
|
||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | M | SD | ||
| 6. | It scares me when my heart beats rapidly. | 0.76 | −0.08 | 0.20 | 3.28 | 1.23 |
| 10. | It scares me when I am short of breath. | 0.76 | −0.07 | 0.06 | 3.01 | 1.32 |
| 9. | When I notice that my heart is beating rapidly, I worry that I might have a heart attack. | 0.72 | −0.01 | −0.16 | 2.43 | 1.35 |
| 4. | It scares me when I feel faint. | 0.71 | −0.13 | 0.19 | 3.28 | 1.31 |
| 14. | Unusual body sensations scare me. | 0.54 | 0.20 | 0.09 | 2.61 | 1.22 |
| 3. | It scares me when I feel ‘shaky’ (trembling). | 0.43 | 0.16 | 0.32 | 2.86 | 1.26 |
| 11. | When my stomach is upset, I worry that I might be seriously ill. | 0.43 | 0.28 | −0.29 | 1.78 | 1.04 |
| 8. | It scares me when I am nauseous. | 0.56 | 0.16 | −0.12 | 2.26 | 1.21 |
| 2. | When I cannot keep my mind on a task, I worry that I might be going crazy. | −0.03 | 0.74 | −0.02 | 1.60 | 0.98 |
| 15. | When I am nervous, I worry that I am mentally ill. | −0.03 | 0.80 | −0.09 | 1.80 | 1.17 |
| 12. | It scares me when I unable to keep my mind on a task | −0.02 | 0.74 | 0.12 | 2.23 | 1.14 |
| 16. | It scares me when I am nervous. | 0.14 | 0.54 | 0.24 | 2.55 | 1.28 |
| 1. | It is important to me not to appear nervous. | 0.04 | 0.14 | 0.59 | 3.51 | 1.24 |
| 5. | It is important to me to stay in control of my emotions | 0.09 | 0.05 | 0.58 | 3.79 | 1.04 |
| 13. | Other people notice when I feel shaky. | 0.03 | 0.20 | 0.33 | 2.02 | 1.16 |
| 7. | It embarrasses me when my stomach growls. | 0.24 | 0.19 | 0.17 | 1.98 | 1.12 |
Note: factor loadings ≥|0.30| are listed in boldface type.
Next, a confirmatory factor analysis was conducted comparing the goodness-of-fit indices of the hierarchical model to other competing and more parsimonious models. As recommended by Zinbarg et al. (1999), we calculated the goodness of fit of two additional ASI models: a three-factor orthogonal model and a single factor solution. The goodness of fit indices for the hierarchical model and the two competing models are reported in Table 2.
Table 2.
Goodness-of-fit indices for hierarchical factor model and two comparison models
| Model | df | χ2 | CFI | AIC | SRMC | RMSEA |
|---|---|---|---|---|---|---|
| One-factor | 104 | 479.33 | 0.704 | 271.33 | 0.0968 | 0.131 |
| Three-factor | 104 | 379.12 | 0.783 | 171.12 | 0.2116 | 0.112 |
| Hierarchicala | 101 | 272.78 | 0.865 | 70.78 | 0.0824 | 0.089 |
Note. CFI=Bentler’s (1989) robust comparative fit index; AIC=Akaike’s (1987) information criterion; SRMR=standardized root mean squared residual; RMSEA=root mean square error of approximation.
The hierarchical model contained three first-order factors that each loaded on a single second-order factor.
Hierarchical χ2 tests confirmed that the differences among the three models in goodness of fit suggested by these indices were statistically different. The hierarchical model provided a significantly better fit to the data than did the model with three orthogonal factors, χ2 (1, N=206) =106.34, p<0.001, indicating that the second-order, general factor accounts for a significant proportion of variance beyond what can be accounted for by the three first-order factors alone. In addition, the hierarchical model provided a significantly better fit to the data than did the single-factor model, χ2 (3, N=206)=206.55, p<0.001, indicating that the first-order factors account for a significant proportion of the variance beyond what can be account for by the general factor alone.
4.2. Factor intercorrelation analyses
A series of Pearson correlations were conducted examining the interrelationships among the ASI subdimensions and their relationship to the total ASI scale. Due to the longitudinal nature of HARP, we were also able to examine data on the 86 participants who completed a second administration of the ASI as part of their yearly assessment battery (mean length of time between ASI administrations=44.3 weeks (SD=13.3 weeks)). These analyses allowed us to examine the general stability of the ASI total score and the sum scores on its subscales across time, as well as the test–retest reliability of ASI total and subscale scores. The results of these correlational analyses are depicted in Figure 1.
Fig. 1.
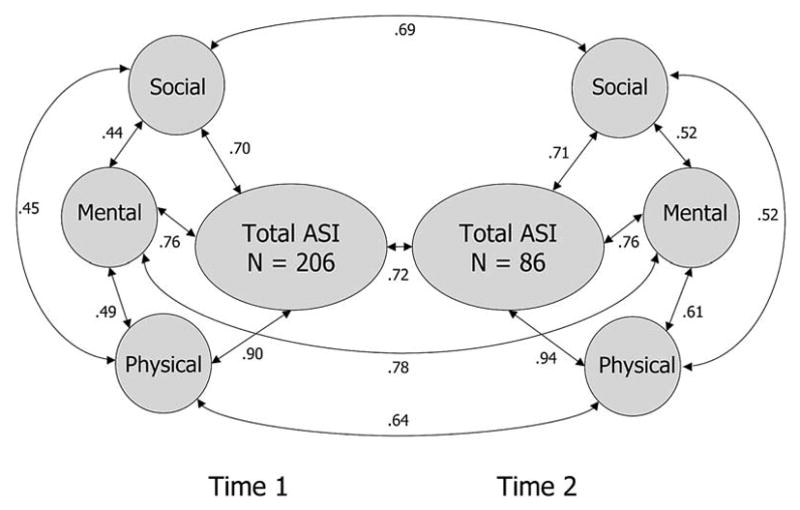
Pearson correlations between the ASI subscales and total scores across two yearly administrations.
As can be seen in the figure, the subdimensions of the ASI show large-sized correlations with the overall ASI total score at both assessment points. The strongest of these correlations is between ASI physical concerns and the ASI total score. The physical concerns, mental incapacitation concerns, and social concerns subscales also show large-sized correlations with each other, but these correlations are notably smaller than the correlation between these scales and the ASI total score. Examination of the ASI and its subscales over time indicated large correlations between Time 1 and Time 2 administrations, suggesting that scores on the ASI remain relatively stable over time. The test–retest reliability for the ASI total score is comparable to that reported in other studies (e.g. Reiss et al., 1986; Maller & Reiss, 1992).
4.3. Profile analysis
HARP does not assign a ‘primary diagnosis’ to the participants in our study who have multiple anxiety disorders. Furthermore, rates of anxiety and mood disorder comorbidity among study participants are quite high (for a description of the rates of anxiety disorder comorbidity in HARP, see Goisman, Goldenberg, Vasile, & Keller (1995)). Consequently, we were unable to directly compare the different anxiety disorders as primary diagnoses with regard to elevations on specific ASI subdomains. As an alternative approach, we conducted a series of multiple regressions wherein participants’ diagnostic status for PD, PDA, GAD, SP and MDD at the time of ASI assessment was dummy coded and used to predict ASI total score, as well as the sum scores for each ASI subscale. As a reference, Table 3 presents the means and standard deviations for ASI total and subscale scores for the entire sample, and for participants with a given anxiety diagnosis.
Table 3.
Mean ASI total and subscale scores by diagnosis
| ASI Subscales
|
|||||
|---|---|---|---|---|---|
| n | ASI Total | Physical Concerns | Mental Incap. Concerns | Social Concerns | |
| PD | 15 | 44.20 (9.21) | 23.93 (5.40) | 8.07 (3.37) | 12.20 (3.67) |
| PDA | 103 | 44.61 (11.77) | 23.83 (6.94) | 9.18 (4.06) | 11.60 (3.20) |
| GAD | 69 | 44.23 (11.71) | 22.63 (7.07) | 9.99 (4.03) | 12.35 (3.14) |
| SP | 60 | 45.45 (10.87) | 22.55 (6.45) | 9.75 (3.96) | 13.15 (2.98) |
| MDD | 60 | 46.47 (10.87) | 23.65 (6.54) | 10.23 (4.36) | 12.58 (3.28) |
| Total sample | 206 | 42.45 (11.37) | 22.14 (6.88) | 8.76 (3.87) | 11.54 (3.20) |
Note. Sum of diagnostic group n’s is greater than total sample n due to comorbidity. PD=panic disorder without agoraphobia. PDA=panic disorder with agoraphobia. GAD=generalized anxiety disorder. SP=social phobia. MDD=major depressive disorder. Mental Incap. Concerns=Mental Incapacitation Concerns.
The first regression model (see Table 4) found significant associations between increases in ASI total score and the diagnoses of PDA, SP and MDD, with the most significant association being with the PDA diagnosis. Consistent with theory, this same model also found a non-significant trend for an association with PD diagnosis and an increase in ASI total score, however, the small number of subjects in the sample with PD likely affected the significance of this result. The second regression found significant increases in the ASI Physical Concerns score associated with the diagnoses of both PD and PDA. Once again, the most significant associations were for PDA. The third regression found the diagnosis of MDD to be most significantly associated with increased ASI Mental Incapacitation Concern, with the diagnoses of GAD and SP also showing significant associations. The final regression indicated increased scores on the Social Concerns subdomain of the ASI were most significantly associated with the diagnosis of SP, although GAD and MDD were also significantly associated with increased scores on ASI Social Concerns.
Table 4.
Multiple regression analysis with diagnostic status predicting ASI total and subscale scores
| Variable | B | SE | Model Fa | Adjusted R2 |
|---|---|---|---|---|
| ASI Total Score | 6.11**** | 0.11 | ||
| PD | 5.09+ | 3.02 | ||
| PDA | 5.63*** | 1.63 | ||
| GAD | 1.44 | 1.62 | ||
| SP | 5.30** | 1.71 | ||
| MDD | 4.10* | 1.70 | ||
| Physical Concerns | 4.74*** | 0.08 | ||
| PD | 4.04* | 1.86 | ||
| PDA | 4.19**** | 1.00 | ||
| GAD | −0.87 | 0.99 | ||
| SP | 1.63 | 1.05 | ||
| MDD | 1.50 | 1.04 | ||
| Mental Incap. Concerns | 5.61**** | 0.10 | ||
| PD | −0.13 | 1.04 | ||
| PDA | 0.84 | 0.56 | ||
| GAD | 1.41* | 0.55 | ||
| SP | 1.38* | 0.59 | ||
| MDD | 1.58** | 0.58 | ||
| Social Concerns | 7.98**** | 0.15 | ||
| PD | 1.18 | 0.83 | ||
| PDA | 0.60 | 0.45 | ||
| GAD | 0.90* | 0.45 | ||
| SP | 2.29**** | 0.47 | ||
| MDD | 1.01* | 0.47 |
Note. PD=panic disorder without agoraphobia. PDA=panic disorder with agoraphobia. GAD=generalized anxiety disorder. SP=social phobia. MDD=major depressive disorder. Mental Incap. Concerns=Mental Incapacitation Concerns.
df=5, 200.
p<0.10.
p<0.05.
p<0.01.
p<0.001.
p<0.0001.
5. Discussion
The underlying factor structure of the ASI has been the source of significant debate over the years with a consensus recently emerging that supports a hierarchical factor structure. The results of our study provide additional support for such a hierarchical model of the ASI that contains three distinct first-order factors corresponding to physical concerns, mental incapacitation concerns, and social concerns that all load on a single second-order factor. Both the factor structure and composition replicate the results reported in other studies (Taylor, 1996; Zinbarg et al., 1997). Our analyses further confirm the hierarchical factor solution is significantly better than orthogonal three-factor and single-factor solutions. In addition, we expanded upon previous examinations of the factor structure of the ASI by presenting intercorrelations and test–retest reliabilities for both the ASI total score and the subscale scores. These analyses indicated that participant scores on the physical concerns, mental incapacitation concerns, and social concerns dimensions remain relatively stable across time, suggesting these subscales do represent enduring individual differences in the propensity to fear different aspects of anxiety.
Studies confirming that the ASI possesses an underlying hierarchically-organized, multidimensional structure have important implications for anxiety sensitivity theory. Reiss and colleagues (Reiss et al., 1986; Reiss & McNally, 1985) initially conceptualized anxiety sensitivity as an individual difference in the tendency to fear anxiety sensations that plays a unique role in the development of panic disorder. The results of more recent studies such as this one indicate that elevations in anxiety sensitivity are not unique to panic patients as originally theorized. They additionally suggest that the level of differentiation within anxiety sensitivity can be even more fine-grained than Reiss and colleagues anticipated. That is, individuals may not only differ in their level of overall fear of anxiety sensations, but they may further differ in their fears of specific anxiety symptoms. This latter finding would be of obvious importance to etiological theories of the various anxiety disorders, as well as to researchers interested in understanding the longitudinal course of anxiety disorders. Elevated ASI total scores have already been shown to be predictive of the development of panic symptoms in those without a history of the disorder (Schmidt et al., 1997, 1999). Future studies may also wish to examine the predictive validity of the physical concerns, mental incapacitation concerns, and social concerns subscales of the ASI as they apply the development and maintenance of the different anxiety disorders.
Our study also examined the more specific relationships between physical concerns, mental incapacitation concerns, and social concerns and each of the anxiety disorders in our sample. Controlling for the effects of diagnostic comorbidity using multiple regression analysis, the diagnosis of panic disorder with agoraphobia was associated with a significant elevation in physical concerns relative to those without the disorder. Similarly, a significant elevation in social concerns was found for participants with social phobia, where those with GAD had moderate increases in both social concerns and mental incapacitation concerns relative to those participants without the respective disorders. Given the nature of the anxiety disorders examined and the composition of the ASI subscales, these differences are rather intuitive. Nonetheless, these results provide some evidence for the discriminant validity of these subdimensions of anxiety sensitivity among anxiety disordered outpatients.
Significant elevations in overall anxiety sensitivity, social concerns, and mental incapacitation concerns were also observed for participants in the sample with MDD relative to those without the disorder. Since anxiety sensitivity is a theoretical construct unique to anxiety disorders, such elevations with regard to major depression are not predicted by theory, even though they have also been observed by other researchers (e.g. Taylor et al., 1997). Since the present sample is composed entirely of participants with anxiety disorders, interpretations of this finding are limited. One possible explanation is that comorbid major depression may exacerbate the individual differences in anxiety sensitivities already present in anxiety disorder patients, thus producing the observed elevations. Alternatively, individuals prone to major depression may have an inherent fear of the somatic, cognitive or social sequelae of their disorder that manifests in a fashion comparable to anxiety sensitivity. The lack of a comparison group of non-anxious participants with major depression prevents further testing of these hypotheses in the current study. Future studies in this area are needed to further explore the relationship between anxiety sensitivity and depression.
Since HARP’s design does not assign a primary anxiety disorder diagnosis to participants with multiple comorbid diagnoses, we were unable to make direct comparisons between patients with different primary anxiety disorders regarding their scores on the sub-dimensions of anxiety sensitivity. Similar analyses have been reported by other researchers elsewhere (e.g. Zinbarg et al., 1997), and help to illustrate the differences between anxiety disorders in regard to lower-order anxiety sensitivities. That being said, our alternative approach, controlling for the presence or absence of a specific anxiety disorder within a multiple regression, also provides equally useful clinical data. Given the high rates of diagnostic comorbidity typically found among individuals with anxiety disorders, comparisons based on a ‘primary’ diagnosis could be considered somewhat artificial and non-reflective of the typical anxiety patient who has multiple co-occurring anxiety and mood conditions. Rather, our analyses illustrate the contribution of the different anxiety disorder diagnoses to elevations in a given anxiety sensitivity.
Finally, it should be noted that, even though the ASI is the gold standard assessment of the anxiety sensitivity construct and possesses well established psychometric properties, the inventory itself is composed of only 16 items and was originally developed to assess what was then considered a theoretically unidimensional construct. As a consequence, factor-derived subscales of the ASI are of unequal length and may not adequately assess the full range of individual differences in anxiety sensitivities. Other, more comprehensive measures of the anxiety sensitivity construct have since been developed, however, and these inventories may provide more robust assessments of subdimensions of anxiety sensitivity (Taylor & Cox, 1998). In the future, researchers may wish to consider the utility of employing alternative measures of anxiety sensitivity in their research programs in order to more fully explore the potential variation and influence of this clinically and theoretically important construct.
Acknowledgments
The Harvard–Brown Anxiety Disorder Research Program is conducted with the participation of the following investigators: M.B. Keller, M.D. (Chairperson); M.T. Shea, Ph.D. (Veterans Administration Hospital, Providence–Brown Medical School); J. Eisen, M.D., K. Phillips, M.D., R. Stout, Ph.D. (Butler Hospital–Brown Medical School); S.E. Bruce, Ph.D., R.B. Weisberg, Ph.D., M.G. Warshaw, M.S.S., M.A. (Brown Medical School); R.M. Goisman, M.D. (Massachusetts Mental Health Center–Harvard Medical School); A. Massion, M.D. (University of Massachusetts Medical Center); M.P. Rogers, M.D. (Brigham and Women’s Hospital–Harvard Medical School); C. Salzman, M.D. (Massachusetts Mental Health Center–Harvard Medical School); G. Steketee, Ph.D. (Boston University School of Social Work); K. Yonkers, M.D. (Yale University School of Medicine); I. Goldenberg, Psy.D.; G. Mallya, M.D. (McLean Hospital–Harvard Medical School); T. Mueller, M.D. (Butler Hospital–Brown Medical School); F. Rodriguez-Villa, M.D. (McLean Hospital–Harvard Medical School); R. Vasile, M.D. (Beth Israel Deaconess Medical Center–Harvard Medical School); C. Zlotnick, Ph.D. (Butler Hospital–Brown Medical School); E. Fierman, M.D. Additional contributions from: P. Alexander, M.D. (Butler Hospital–Brown Medical School); J. Curran, M.D.; J. Cole, M.D. (McLean Hospital–Harvard Medical School); J. Ellison, M.D., M.P.H. (Harvard Pilgrim Health Care–Harvard Medical School); A. Gordon, M.D., S. Rasmussen, M.D. (Butler Hospital–Brown Medical School); R. Hirschfeld Ph.D. (University of Texas, Galveston); J. Hooley, D.Phil. (Harvard University); P. Lavori, Ph.D. (Stanford University); J. Perry, M.D. (Jewish General Hospital–McGill University School of Medicine, Montréal); L. Peterson (Midcoast Medical Group, Rockport, ME); J. Reich, M.D., M.P.H.; J. Rice, Ph.D. (Renard Hospital–Washington University School of Medicine); H. Samuelson, M.A. (Brigham and Women’s Hospital); D. Shera, M.S. (Harvard School of Public Health); N. Weinshenker, M.D. (New Jersey Medical School); M. Weissman, Ph.D. (Columbia University); K. White, M.D. This investigation was supported in part by Wyeth-Ayerst Laboratories, through its Global Research Program on Anxiety and Depression. This project was supported in part by NIMH Grant no. MH51415. The authors would like to thank the anonymous reviewers for helpful comments on a previous draft of this manuscript.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. New York: Guilford Press; 1988. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford Press; 2001. [Google Scholar]
- Clark DM. A cognitive approach to panic. Behaviour Research and Therapy. 1986;24:461–470. doi: 10.1016/0005-7967(86)90011-2. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Borger SC, Enns MW. Anxiety Sensitivity and Emotional Disorders: Psychometric Studies and their theoretical implications. In: Taylor S, editor. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. New Jersey: Erlbaum; 1999. pp. 115–148. [Google Scholar]
- Cox BJ, Enns MW, Walker JR, Kjernisted K, Pidlebury SR. Psychological vulnerabilities in patients with major depression vs panic disorder. Behaviour Research and Therapy. 2001;39:563–567. doi: 10.1016/s0005-7967(00)00027-9. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Parker JA, Swinson RP. Anxiety sensitivity: confirmatory evidence for a multidimensional construct. Behavior Research and Therapy. 1996;34:591–598. doi: 10.1016/0005-7967(96)00006-x. [DOI] [PubMed] [Google Scholar]
- Eke M, McNally RJ. Anxiety Sensitivity, suffocation fear, trait anxiety, and breath-holding duration as predictors of response to carbon dioxide challenge. Behaviour Research and Therapy. 1996;34:603–607. doi: 10.1016/0005-7967(96)00044-7. [DOI] [PubMed] [Google Scholar]
- Goisman RM, Goldenberg I, Vasile RG, Keller MB. Comorbidity of anxiety disorders in a multicenter anxiety study. Comprehensive Psychiatry. 1995;36:303–311. doi: 10.1016/s0010-440x(95)90076-4. [DOI] [PubMed] [Google Scholar]
- Goldstein AJ, Chambless DL. A reanalysis of agoraphobia. Behavior Therapy. 1978;9:47–59. [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott NC, Andreasen NC. The longitudinal interval follow-up evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Lilienfield SO, Turner SM, Jacob RG. Anxiety sensitivity: an examination of theoretical and methodological issues. Advances in Behavior Research and Therapy. 1993;15:147–183. [Google Scholar]
- Lilienfield SO, Turner SM, Jacob RG. Further comments on the nature and measurement of anxiety sensitivity: A reply to Taylor. Journal of Anxiety Disorders. 1996;10:411–424. [Google Scholar]
- Maller RG, Reiss S. Anxiety sensitivity in 1984 and panic attacks in 1987. Journal of Anxiety Disorders. 1992;6:241–247. [Google Scholar]
- Massion AO, Warshaw MG, Keller MB. Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. American Journal of Psychiatry. 1993;150:600–607. doi: 10.1176/ajp.150.4.600. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Panic disorder: A critical analysis. New York: Guilford Press; 1994. [Google Scholar]
- Otto MW, Pollack MH, Fava M, Uccello R, Rosenbaum JF. Elevated anxiety sensitivity index scores in patients with major depression: Correlates and changes with antidepressant treatment. Journal of Anxiety Disorders. 1995;9:117–123. [Google Scholar]
- Peterson RA, Plehn K. Measuring anxiety sensitivity. In: Taylor S, editor. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. New Jersey: Erlbaum; 1999. pp. 61–81. [Google Scholar]
- Peterson RA, Reiss S. Anxiety sensitivity index manual. 2. Worthington, OH: International Diagnostic Systems; 1992. [Google Scholar]
- Rapee RM, Brown TA, Antony MM, Barlow DH. Response to hyperventilation and inhalation of 5.5% carbon dioxide-enriched air across the DSM-III-R anxiety disorders. Journal of Abnormal Psychology. 1992;101:538–552. doi: 10.1037//0021-843x.101.3.538. [DOI] [PubMed] [Google Scholar]
- Reiss S. Expectancy model of fear, anxiety, and panic. Clinical Psychology Review. 1991;11:141–153. [Google Scholar]
- Reiss S. Theoretical perspectives on the fear of anxiety. Behavior Therapy. 1987;19:84–91. [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretical issues in behavior therapy. San Diego, CA: Academic Press; 1985. pp. 107–121. [Google Scholar]
- Reiss S, Peterson RA, Gurskey DM, McNally RJ. Anxiety sensitivity, anxiety frequency, and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Sandin B, Chorot P, McNally RJ. Validation of the Spanish version of the Anxiety Sensitivity Index in a clinical sample. Behavior Research and Therapy. 1996;34:283–290. doi: 10.1016/0005-7967(95)00074-7. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Larew DR, Jackson RJ. The role of anxiety sensitivity in the pathogensis of panic: Prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Larew DR, Jackson RJ. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: Replication and extension. Journal of Abnormal Psychology. 1999;108:532–537. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R Patient Version (SCID-P) New York: Biometrics Research Department, New York State Psychiatric Institute; 1988. [Google Scholar]
- Stewart SH, Taylor S, Baker JM. Gender differences in dimensions of anxiety sensitivity. Journal of Anxiety Disorders. 1997;11:179–200. doi: 10.1016/s0887-6185(97)00005-4. [DOI] [PubMed] [Google Scholar]
- Taylor S. Anxiety Sensitivity: Theoretical perspectives and recent findings. Behaviour Research and Therapy. 1995a;33:243–258. doi: 10.1016/0005-7967(94)00063-p. [DOI] [PubMed] [Google Scholar]
- Taylor S, editor. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. New Jersey: Erlbaum; 1999. [Google Scholar]
- Taylor S. Issues in conceptualization and measurement of anxiety sensitivity. Journal of Anxiety Disorders. 1995b;9:163–174. [Google Scholar]
- Taylor S. Nature and measurement of anxiety sensitivity: Reply to Lilienfield, Turner and Jacob (1996) Journal of Anxiety Disorders. 1996;9:163–174. [Google Scholar]
- Taylor S, Cox BJ. An expanded Anxiety Sensitivity Index: Evidence for a hierarchic structure in a clinical sample. Journal of Anxiety Disorders. 1998;12:463–483. doi: 10.1016/s0887-6185(98)00028-0. [DOI] [PubMed] [Google Scholar]
- Taylor S, Koch WJ, Crockett DJ. Anxiety sensitivity, trait anxiety, and the anxiety disorders. Journal of Anxiety Disorders. 1991;5:293–311. [Google Scholar]
- Taylor S, Koch WJ, McNally RJ, Crockett DJ. Conceptualizations of anxiety sensitivity. Psychological Assessment. 1992;4:245–250. [Google Scholar]
- Taylor S, Koch WJ, Woody SR, McClean P. Anxiety sensitivity and depression: How are they related. Journal of Abnormal Psychology. 1997;105:474–479. doi: 10.1037//0021-843x.105.3.474. [DOI] [PubMed] [Google Scholar]
- Telch MJ, Shermis MD, Lucas JA. Anxiety sensitivity: Unitary personality trait or domain-specific appraisals? Journal of Anxiety Disorders. 1989;3:25–32. [Google Scholar]
- Wardle J, Ahmad T, Hayward P. Anxiety sensitivity in agoraphobia. Journal of Anxiety Disorders. 1990;4:325–333. [Google Scholar]
- Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. Journal of Psychiatric Research. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Barlow DH, Brown TA. The hierarchical structure and general factor saturation of the Anxiety Sensitivity Index: Evidence and implications. Psychological Assessment. 1997;9:277–284. [Google Scholar]
- Zinbarg RE, Brown TA, Barlow DH, Rapee RM. Anxiety sensitivity, panic, and depressed mood: A reanalysis teasing apart the contributions of the two levels in the hierarchical structure of the Anxiety Sensitivity Index. Journal of Abnormal Psychology. 2001;110:372–377. doi: 10.1037//0021-843x.110.3.372. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Mohlman J, Hong NN. Dimensions of anxiety sensitivity. In: Taylor S, editor. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. New Jersey: Erlbaum; 1999. pp. 83–114. [Google Scholar]


