Abstract
Neonatal lupus erythematosus (NLE) is an autoimmune disease affecting the fetus as a result of transplacental transfer of anti-Ro autoantibodies. Typically, it presents in the first few months of life with an annular form of subacute cutaneous lupus erythematosus. We report an unusual case of NLE presenting at birth with scaly erythematous telangiectatic patches and macules with skin atrophy involving the face, head, and upper trunk. Thrombocytopenia was discovered on laboratory investigations. Histopathology of skin biopsy was consistent with subacute cutaneous lupus. The mother was clinically free of disease and had no family history of autoimmune disease. Serology (extra-nuclear antigens) was positive in both the baby and the mother. This is a rare presentation of a rare disease.
Keywords: Atrophic lesions, congenital lupus erythematosus, Saudi Arabia
Introduction
Neonatal lupus erythematosus (NLE) is the result of fetal injury caused by passive transfer of autoantibodies from the mother to the fetus. The autoantibodies are directed against extranuclear antigens SSA/Ro and SSB/La. It presents over a period of weeks to months with a photosensitive annular transient skin rash, reversible alteration of hematological and hepatic function and irreversible cardiac disease. The cutaneous manifestations are histologically identical to those of subacute cutaneous lupus. The cutaneous manifestations typically resolve with few sequelae if any. In contrast to the cutaneous manifestations, the cardiac disease presents at birth. The major cardiac finding is heart block with or without cardiomyopathy.
We report an unusual presentation of NLE presenting at birth with erythematous patches and macules, with telangiectasias and scales distributed on the face and head and atrophic scars on the trunk.
Case Report
The infant was a product of full-term normal spontaneous vaginal delivery. She was born to a 23-year-old mother, P1+0 at fullterm of gestation. She weighed 2.48 kg with an Apgar score of 9/10 and had no perinatal complications. She is the offspring of a nonconsanguinous marriage. The mother had regular antenatal visits and was completely healthy.
The infant was noted to have a skin rash by the pediatrician at birth and was referred to dermatology. On examination, she had erythematous patches and macules with telangiectasias and atrophy, with fine scales in a few lesions. The changes were concentrated but were not limited to the face, in particular the periorbital region [Figure 1]. On the upper trunk and scalp, there were multiple atrophic macules with telangiectasias. No dysmorphic features were noted.
Figure 1.

Erythematous confluent macular rash involving the face, especially the periocular area, with atrophic depressed lesion on the forehead
A thorough physical examination was performed by the pediatrician, which failed to reveal lymphadenopthy or organomegaly. Abdominal ultrasonography was normal.
On investigations, a complete blood count (CBC) showed a platelet count of 92.4 × 10.e9/L. On repeat CBC, a value of 81.6 × 10.e9/L was obtained. Liver enzymes were normal. A full TORCH screen, herpes and syphilis screening for the newborn and the mother was negative. Serology for anti nuclear antibody (ANA) and extractable nuclear antigen (ENA) antibodies were tested for the infant and mother. The infant had positive anti-Ro and anti-La antibodies. ANA was negative. A 3-mm skin biopsy was taken from a lesion on the scalp. The histopathological examination of the skin biopsy revealed epidermal atrophy, follicular plugging, vacuolar interface dermatitis at the dermoepidermal junction and superficial perivascular lymphocytic infiltrate with dermal edema [Figure 2]. Alcian blue stain was positive for dermal mucin deposition. Direct immunoflourescence microscopy revealed a band of IgG, IgM and C3 deposits at the dermoepidermal junction.
Figure 2.
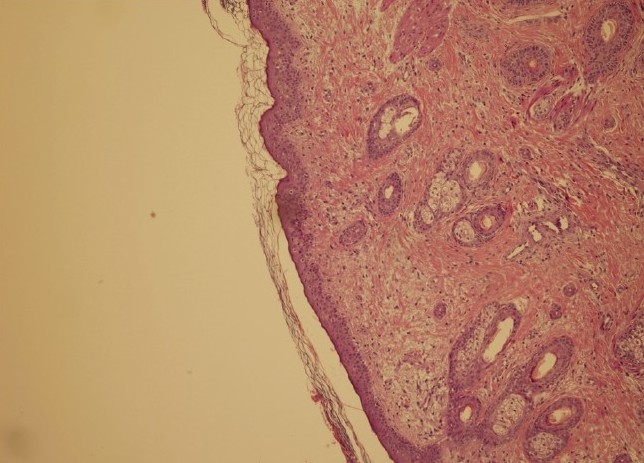
Flattened epidermis with follicular plugging and vacuolar degeneration of the basal layer. There is edema of the papillary dermis (H & E stain, 100×)
This confirmed the diagnosis of NLE. The patient was referred to cardiology and had an electrocardiogram (ECG) and an echocardiograph done. The physical examination and both studies were normal.
In view of these results, the mother was seen by a rheumatologist and screened for collagen vascular disease. The clinical examination was normal but the serology was positive for both anti-Ro and anti-La autoantibodies.
The mother and infant were discharged from the hospital after 1 week. The patient was given 1% hydrocortisone cream to be applied twice-daily to the lesions and advised the use of sun protection. They were seen in follow-up 2 weeks later. The erythematous patches on the face and scalp improved, leaving telangiectasias and atrophy.
Discussion
Neonatal lupus erythematous is an uncommon autoimmune disorder described first in 1954 by McCuiston and Schoch.[1] It is a passive autoimmune disease secondary to the transplacental transfer of ANA and extractable nuclear antigen (anti-Ro and anti-La; U1-RNP) antibodies to the fetus.[2] The mother may be apparently healthy or may have an overt connective tissue disorder.[3] NLE is characterized by a combination of dermatological, cardiac, hematological and hepatic manifestations. The skin lesions are characterized by annular or polycyclic erythematous scaly plaques evolving within the first month of birth, and involve mostly the face, especially the periocular area. The lesions are transient and resolve over a period of 6–9 months along with a decline in the autoantibody levels, but may leave behind residual dyspigmentation, scarring and telangectasia. Cardiac manifestations are seen in half of the NLE cases and present as irreversible conduction defects.[4] About 10% of the NLE is present with both cardiac and dermatologic disease. Hematological and hepatic abnormalities are often asymptomatic and transient. They include hemolytic anemia, neutropenia, thrombocytopenia and elevated liver enzymes, respectively.[5]
The presence of congenital cutaneous lesions showing evidence of atrophy is very rare, with only few cases reported in the literature.[6,7] It indicates the occurrence of the lesions during pregnancy with an irreversible outcome.
Our patient presented with both inflammatory lesions as well as atrophic scars at birth. The inflammatory lesions were present on the scalp, face and ears as oval scaly erythematous macules with confluence over the central portion of the face. The characteristic annular skin lesions of NLE were not seen in our patient. The skin on the scalp and forehead had multiple depressed, atrophic scars with telangiectasias. Some of the lesions on the trunk had a morphea-like appearance. The presence of scars and telangectasia made us consider other possible differential diagnoses, which include congenital viral infections and genetic disorders, such as Rothmond-Thompson and Goltz syndrome besides NLE.
The congenital presence of the inflammatory lesions seen in our patient also puts a doubt over the role of ultraviolet rays as a primary triggering factor for the dermatitis seen in NLE. The diagnosis of NLE was confirmed by the histopathology and direct immunoflouresence of the skin biopsy as well as the presence of the autoantibodies seen in both the neonate and the mother.
In conclusion, we believe this to be a very interesting case of NLE presenting at birth. The presence of cutaneous involvement at birth, in addition to the lack of maternal history, posed a diagnostic challenge. Confirmation of the diagnosis was made on skin biopsy and positive serology.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.McCuiston CH, Schoch EP. Possible discoid lupus erythematosus in newborn infant. Arch Dermatol. 1954;70:781–5. [Google Scholar]
- 2.Crowley E, Frieden IJ. Neonatal lupus erythematosus: An unusual congenital presentation with cutaneous atrophy, erosion, alopecia and pancytopenia. Pediatr Dermatol. 1998;15:38–42. doi: 10.1046/j.1525-1470.1998.1998015038.x. [DOI] [PubMed] [Google Scholar]
- 3.Miyagawa S, Shinohara K, Kidoguchi KI, Fujita T, Fukumoto T, Yamashina Y, et al. Neonatal lupus erythematosus: HLA-DR and DQ distribution are different among the groups of anti-Ro/SSA-positive mothers with different neonatal outcomes. J Invest Dermatol. 1997;108:881–5. doi: 10.1111/1523-1747.ep12292592. [DOI] [PubMed] [Google Scholar]
- 4.Winkler RB, Nora AH, Nora JJ. Familial congenital complete heart block and maternal systemic lupus erythematosus. Circulation. 1977;56:1103–6. doi: 10.1161/01.cir.56.6.1103. [DOI] [PubMed] [Google Scholar]
- 5.Watson RM, Kang JE, May M, Hudak M, Kickler T, Provost TT. Thrombocytopenia in the neonatal lupus syndrome. Arch Dermatol. 1988;124:560–3. [PubMed] [Google Scholar]
- 6.Cimaz R, Biggioggero M, Catelli L, Muratori S, Cambiaghi S. Ultraviolet light exposure is not a requirement for the development of cutaneous neonatal lupus. Lupus. 2000;11:257–60. doi: 10.1191/0961203302lu171cr. [DOI] [PubMed] [Google Scholar]
- 7.Diociaiuti A, Paone C, Giraldi L, Paradisi M, El Hachem M. Congenital Lupus Erythematosus: Case report and review of the literature. Pediatr Dermatol. 2005;22:240–2. doi: 10.1111/j.1525-1470.2005.22313.x. [DOI] [PubMed] [Google Scholar]


