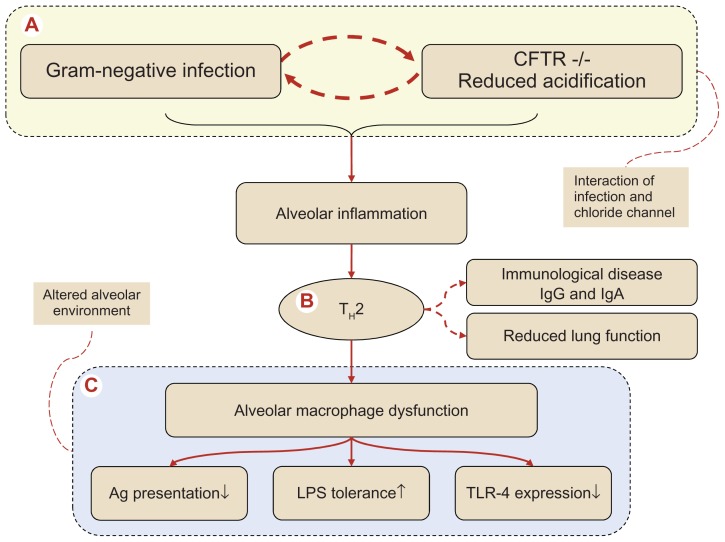
Figure 1.
Pathogenesis of the complex series of events in cystic fibrosis (CF) progressing to alveolar macrophage dysfunction via a TH2 dominated alveolar inflammation. (A) Denotes the interaction between the defective cystic fibrosis transmembrane conductance regulator (CFTR)−/− macrophages in respect to intracellular acidification and Gram-negative infection, an interaction involving a T-cell switch (B) to an alveolar T-helper 2 response with induction of B-cell activation with antibody formation, transforming CF into an immunological allergic disease characterized by increased systemic immunoglobulin formation (IgG and IgE). The TH2 response has been connected with an unfavorable accelerated declined spirometry. The end stage of the altered alveolar environment (C) with alveolar macrophage dysfunction, reflected by (i) reduced antigen (Ag) presentation, (ii) enhanced tolerance toward lipopolysaccharide (LPS) and finally (iii) reduced expression of recognition receptors, the so-called toll-like receptors (TLR) where TLR-4, which recognizes Gram-negatives, is decreased. In the end, remodeling of peripheral airways will take place producing a reduced alveolar host defense.