Abstract
Background
Fingertip amputation is the most common type of injury in the upper limb. Goals in fingertip amputation reconstruction are covering the defect, establishing maximum tactile gnosis, keeping the length of the finger, protecting the joint function, acquiring a well-padded pulp tissue, providing a bed for growing nail, obtaining a satisfactory cosmetic appearance and allowing the patient to return to work as soon as possible. Adjacent skin and soft tissue are the best covers for fingertip injuries. However, local homodigital flaps lack enough tissue to cover the defect. To solve this problem, we used V–Y rotation advancement flap bilaterally in fingertip amputations which meets all the reconstruction goals. Rotation besides advancement makes this flap more mobile and easier to cover larger defects in all amputation planes.
Methods
Between 2007 and 2009, we performed bilateral V–Y rotation advancement flap on seven male patients’ pulpa (average age, 37.6 years) whose fingertips were not replantable.
Results
Fourteen flaps were made on 7 fingers. There was neither total nor partial flap loss. Patients had neither cold intolerance nor scar hypersensitivity. Stiffness of the PIP joint did not occur. No obvious hooked nail occurred in patients who have remaining nail matrix. Because flaps contain neurovascular bundle, there was no difference in sensation and perfusion between the finger’s pre-operative and post-operative status. The result was satisfactory with painless pinching.
Conclusion
In addition to the various and versatile fingertip reconstruction methods, we want to present V–Y rotation advancement flap as a quick, reliable and aesthetic method.
Keywords: Fingertip, Amputation, V–Y flap, Reconstruction, Pulpa
Introduction
We could use tools, carry things, eat and drink thanks to our hands. But they also help us express ourselves in social life and we describe ourselves with hands while talking. Children recognise the world fearlessly with their fingers. This is the reason why fingertip injuries constitute the largest part of hand traumas in children [8].
Doing fine work and holding things happen with fingertips. That is the reason why fingertip amputation is the most common type of injury seen in the upper limbs [8]. Goals in fingertip amputation reconstruction are covering the defect, establishing maximum tactile gnosis, keeping the length of the finger, protecting the joint function, acquiring a well-padded pulp tissue, providing a bed for growing nail, obtaining a satisfactory cosmetic appearance and allowing the patient to return to work as soon as possible. There are some factors that should be considered, which affect the reconstruction choice: nature of the injury, the size, place and condition of the defect, additional injuries in other parts of the hand, age, gender, the patient’s general health condition and surely the patient’s profession.
Treatment of fingertip injuries ranges in a large spectrum which correlates to the reconstruction ladder: secondary intention, primary closure, grafting (split, full thickness and composite [35, 41]) and flaps. Flaps are classified mainly into homodigital flaps [4, 10, 12, 17, 20, 25, 33, 39, 42], heterodigital flaps (cross-finger flap [7, 29]), distant flaps [10], island flaps (homodigital [1, 5, 13, 38, 44], heterodigital [30] and metacarpal [19]), perforator flaps [23] and free flaps [9, 21, 24, 27, 45].
In this variety of methods, a reconstructive surgeon’s duty is to choose the best method which meets the patient’s needs [42]. Adjacent skin and soft tissue are the best covers for fingertip injuries. Local homodigital flaps are easy to apply and teach, they usually do not need microsurgical instruments, their operation time is short, they do not need long immobilisation period and patients return to work earlier. In general, they lack soft tissue and skin to cover the defect. To solve this problem, we use V–Y rotation advancement flap, which is first described by Argamosa [3] and used by many surgeons [6, 11, 37], bilaterally in fingertip amputations. Rotation besides advancement makes this flap more mobile and easier to cover larger defects in all amputation planes. Because flaps contain neurovascular bundle, there is no difference in sensation and perfusion between the finger’s pre-operative and post-operative status.
Materials and Methods
Between 2007 and 2009, we performed V–Y rotation advancement flap on seven male patients whose fingertips were not replantable. Patients’ age ranged from 21 to 65 years old (average, 37.6 years). All patients were heavy smokers (one pack or more per day). Four of the patients had history of previous hand trauma. Two patients had thumb tip, four had second fingertip and one had third fingertip amputations. Regarding the classification of Ishikawa et al. [18] for fingertip amputation, three patients’ amputation were in zone II, three others were in zone III and one was in zone I. Two fingers’ amputation plane were volar oblique, three fingers’ amputation plane were transverse, one finger’s amputation plane was dorsal oblique and one finger’s amputation plane was lateral oblique (Table 1). Patients had no additional injuries apart from finger amputation. Patients applied to the emergency service in 30 min to 5 h (average, 1.5 h) after the fingertip amputation. All the patients were vaccinated for tetanus and the injured hand’s X-rays were taken prior to plastic surgery consultation.
Table 1.
Patients’ data
| Patient | Age and sex | Injured finger | Mechanism of injury | Amputation zone (Ishikawa) | Amputation plane |
|---|---|---|---|---|---|
| 1 | 32, M | 1 | Avulsion | II | Volar oblique |
| 2 | 28, M | 1 | Crush | II | Transverse |
| 3 | 43, M | 2 | Sharp | III | Transverse |
| 4 | 48, M | 2 | Crush | III | Volar oblique |
| 5 | 21, M | 2 | Crush | III | Dorsal oblique |
| 6 | 26, M | 3 | Crush | II | Lateral oblique |
| 7 | 65, M | 2 | Sharp | I | Transverse |
Operative Technique
Operation was begun after digital block has been done with 1.5–2 cc prilocaine 2% bilaterally and a rubber glove was applied as a tourniquet to the base of the finger. Surgery lasted for 25–35 min (average, 28 min). None of the fingers’ exposed bone was shortened, only the sharp ends had been trimmed.
After haemostasis, V–Y rotation advancement flaps were planned bilaterally on the volar side of the remaining pulpa (Figs. 1 and 2). The length of the flap’s base was equal to half of the defect. Limbs of the “V” were planned in a convex manner in order to include the digital artery and nerve inside the flap (Fig. 3). A longitudinal line that divides the phalanx in half is drawn from the defect to the major volar joint crease. The long limb of “V” was drawn from the defect’s midpoint to the quarter point of the joint crease and tangent to the midline. The short limb of “V” was drawn from the quarter of the joint crease to the half of the remaining fingertip’s mid-lateral line. If more tissue is needed, short limb could be made from finger’s volar lateral line to the dorsal lateral line. Theoretically, the tissue between the distal point of the short limb and major volar crease is transferred to the defect by rotation. By adding advancement to this rotation, larger tissue could cover the defect (Figs. 4 and 5). Flaps were elevated above the flexor tendon’s paratenon by keeping the digital bundle inside the flap. Both flaps advanced and rotated to the defect where it closed as “Y” (Fig. 6). The flaps’ distal medial corners were sutured to the midpoint of the dorsal skin or remaining nail. These are the key sutures of the flaps. Then, the flaps’ distal edges were sutured to the dorsal skin or remaining nail. The flap’s inferomedial edges were sutured to the curved triangle that is formed after the flap elevation. Small triangle defects occurred at the junction between the joint crease and the finger’s lateral line. These defects were covered with dressing and left to secondary healing. Whole new reconstructed fingertip was covered with fucidin-absorbed gauze. Finger splint was not applied. Neither congestion nor paleness was observed after the procedure. Although all the injuries happened because of work accident, they were accepted as contaminated wounds and prophylactic amoxicillin/clavulanate 1,000 mg twice a day for 5 days were prescribed to all patients. Non-steroid analgesic was also prescribed, but patients were suggested not to use unless pain is irresistible because of its negative effects on wound healing. Hand elevation is recommended for pain relief and venous drainage. Patients were discharged from hospital after the operation.
Fig. 1.

Index finger, dorsal oblique amputation at Ishikawa zone III (patient 5)
Fig. 2.
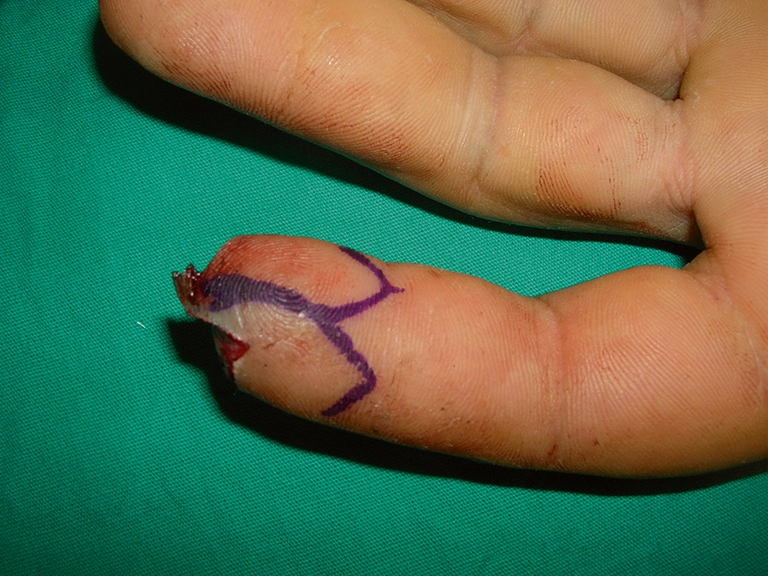
Pre-operative drawing of V–Y rotation advancement flap for dorsal obliquely amputated fingertip (patient 5)
Fig. 3.
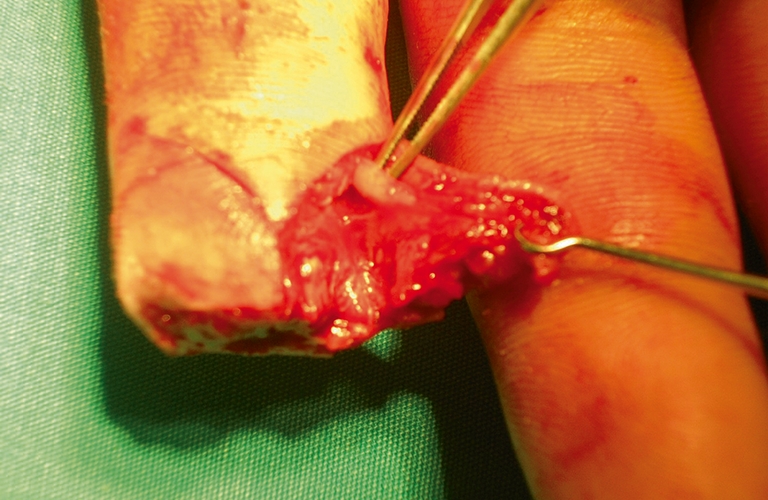
Demonstration of digital artery inside the flap (patient 3)
Fig. 4.

Incision of the flap (patient 5)
Fig. 5.

Rotation and the advancement of movements of the flap (patient 5)
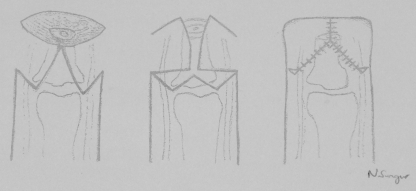
Fig. 6.
Illustration of the fingertip reconstruction with V–Y rotation advancement flap. Left Ishikawa zone III, transverse fingertip amputation and design of “V”-shaped flaps. Centre transfer of flaps by keeping neurovascular bundle inside. Right “Y”-shaped closure of the defect
Results
Fourteen flaps were made on 7 fingers. The size of the defect ranged from 1 × 0.4 to 2 × 1 cm. The mean unilateral flap size was about 1.5 × 0.6 cm (from 1 × 0.5 to 1.8 × 0.9 cm). Dressings were changed every other day and sutures were removed on the 10th–14th post-operative day. The follow-up period was 3 months to 2 years (average, 18 months). There was neither total nor partial flap loss (Figs. 7 and 8). Physical therapy was not necessary because the fingers had full range of motion. None of the patients had cold intolerance or scar hypersensitivity. No stiffness of the PIP joint was seen. No obvious hooked nails occurred in patients who have remaining nail matrix. Satisfactory function and sensation on the amputation stump were obtained. Most patients returned to work in about 1.5–2.5 weeks (the mean time off work was 9 days). In all patients, two-point discrimination test was 6 mm or less and the same as the contralateral finger.
Fig. 7.
a Dorsal view of patient 3 with transverse, Ishikawa zone III index fingertip amputation. b Volar view of the finger. c Design of flaps which extend to the lateral sides of the finger. d Transfer of flaps. e Dorsal view of the closure. f Volar view of the closure. g Dorsal view, first post-operative month. h Volar view, first post-operative month. i Volar view, sixth post-operative month
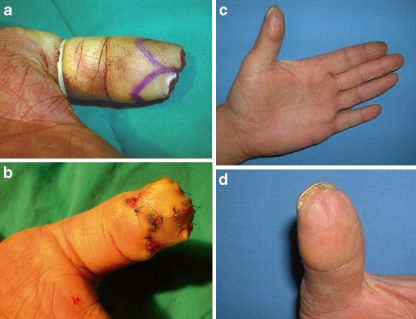
Fig. 8.
a Flaps design of patient 2 who has Ishikawa zone II, transverse thumb tip amputation. b Volar view of the closure. c Lateral view of the thumb, first post-operative month. d Close-up view of pulpa with minimal incision scar
Discussion
Fingertip injuries are the most common injuries in hand trauma patients. The major cause for adult patients is occupational accidents [8, 43] and this data supports our patients’ aetiology. There are several classifications for fingertip injuries [2, 14]. Treatment options vary depending on the injury mechanism, defect’s size and plane, surgeon’s intention, patient’s needs, condition of the stump and the amputated part. However, there is a consensus that replantation is the best choice by maintaining the length of the finger and the normal anatomy of the nail complex, if only the amputated fragment is available, in replantable condition and well preserved [34, 42]. If replantation is not possible, reconstruction ladder could be used for fingertip injuries: secondary healing, primary closure, skin grafting, homodigital flaps (V–Y advancement [4], V–Y cup [41], dorsal visor [20], Kutler [25], Moberg [35], hatchet [4], Hueston [10], linguiform rotation [12], dorsal adipofascial flaps [26, 28, 40], cross-finger flap [20, 25], island flaps (homodigital [5, 7, 13, 29, 38], heterodigital [30] and metacarpal [19]) (antegrade and retrograde [38]), digital artery perforator flaps [23], distant flaps (thenar flap [10], groin and abdominal), free flap (free toe pulp [9, 22, 31], venous [33, 39] and medial plantar perforator [17, 42]).
Secondary healing is ideal for non-bone-exposed, clean wounds smaller than 1–1.5 cm2 in adult patients [7, 29]. However, secondary healing is vulnerable to infection and it discourages patients by frequent and painful dressing changes. Due to prolonged complete wound healing time, varying between 2 and 6 weeks regarding the defect size [38], patients have difficulty in returning work. Additional major disadvantages are scarring and pulp’s soft tissue loss [36]. In conclusion, this method might have satisfactory results, but they are often inferior to other reconstruction techniques [7].
Primary closure in fingertip injuries is possible only in lacerations and blunt crushes. However, the most common type of injury is tip amputation where there is a lack of soft tissue and skin. Most of the reconstructive surgeons and patients do not prefer this method because of its need for bone shortening. In advantage, sensation will not be compromised in direct closure, which is crucial for function. If there is not enough soft tissue to cover the bone, the patient could suffer from the solid and sharp end of the bone while pinching. Moreover, tight closure results in flexion deformity, which may progress to finger stiffness, and cold sensitivity happens more in direct closure than grafting [15].
Split and full thickness grafts are a good choice for clean wounds larger than 1–1.5 cm2 where bone or tendon is not exposed and for patients who do not want to spend time for the secondary healing process. But there will always be a donor scar which may be cosmetically unacceptable and may cause excessive scarring and hypersensitivity. In addition, immobilisation is obligatory after grafting. Their results are often acceptable, but some complications may occur, e.g. loss of pulpa contour, scar contracture (mostly in split thickness graft), hypoaesthesia or hyperaesthesia [13, 29]. Nevertheless, skin grafts would rather be used only if the wound is too large for secondary healing and if it is not worth trying another method [7].
Local flaps are a good choice to cover exposed vital tissues (bone, tendon, digital nerve and artery) without shortening the bone and other fingers are kept untouched. They are also better than skin grafting to restore pulp contour and fullness. As they are random flaps, surgeons must be sure that an artery is included into the flap. Surgeons also must be aware of the patient’s age, smoking habit and associated diseases (diabetes, atherosclerosis, Reynaud’s disease, etc.) which could compromise flap circulation [1]. Local flaps’ major disadvantages are limited length of advancement, limited size of flaps and loss of pulp sensation due to scar line (V–Y advancement) and lack of nerve incorporation (thenar flap) in the flap.
Cross-finger flap is a good option if other local flaps are not available. Flap elevation from a healthy finger results in new morbidities such as joint stiffness, unacceptable scars and contour deformities. This technique always needs skin grafting for donor site and a second surgery for flap separation. This method is out of the question for patients who do not want to have stuck fingers for 2–3 weeks. In general, physical therapy is necessary to repossess normal joint range of movement which delays patient’s return to work.
Island flaps are sophisticated reconstruction methods and demanding technically which needs operating room condition and fine instruments. It causes a second donor wound which could not be closed always by primary closure. Unipedicled island flaps need larger dissection, frequently the whole length of the finger that may result in finger stiffness. Regardless of having nerves inside the flap or not, all island flaps require an interval to restore sensation, and in some flaps, it is not fully recovered. Disadvantages of homodigital island flaps are possibility of graft and flap loss, sacrificing a major artery of the finger, hypersensitivity at the grafted donor area and finger and non-satisfactory appearance [44]. In addition, significant number of patients suffer from cold intolerance [1, 30].
Heterodigital flaps are used for larger digital defects that could not be covered by local flaps or homodigital island flaps [1]. Venous congestion is common in island flaps, and in heterodigital flaps, tunnelling the pedicle under the skin increase that risk.
Distant flaps (abdominal, groin, etc.) or thenar flaps are used in case there is not sufficient tissue to close the defect either by direct closure or local flap [16]. These flaps require multiple stage operations that need prolonged immobilisation between procedures, resulting in joint stiffness.
Reconstruction with free flaps such as partial second toe pulp flap [31], venous flap [21, 45], medial plantar perforator flap and trimmed toe tip method [22] replaces the fingertip with similar glabrous tissue. However, these operations that are time-consuming and costly require experienced surgeons and special fine instruments. Venous congestion is common and it mostly resolves in days with or without medical treatment. Major complications are partial and total flap necrosis that might be the consequence of artery or vein thrombosis. Therefore, similar to island flaps, patients have to stay longer in the hospital than other methods for flap follow-up and medical treatment (IV high molecular dextran, IV heparin, medicinal leech therapy). Patient’s general health condition and smoking habits are very important for flap perfusion. Free pulp or hemipulp transfers’ sensory results are excellent [9, 22], but these results could be also obtained by local flaps. Lee et al. points out that a high proportion of the reconstructed fingers need additional surgeries [31].
To overcome these disadvantages, we describe a new method of bilateral V–Y rotation advancement flap. It is an easy, quick, reliable and versatile method that does not need neither experienced hands nor fine instruments. It could be performed in emergency room conditions. It is a one-stage surgery that uses similar coloured and textured adjacent tissues. It does not need any donor site that may cause additional complications. V–Y rotation advancement flap could be adjusted to every amputation planes by only planning the flaps differently and without bone shortening. It could be called as an axial flap because its pedicle is in the digital bundle. Compared to other regional or distant flaps that give well-padded tissue with random sensation, it uses digital nerve, not smaller branches. That is the reason why there is no alteration in sensation and cortical relearning is not needed.
Due to its rotation while advancing, V–Y rotation advancement flap advance more than V–Y advancement flap and Kutler flap. It differs from the hatchet flap of Tuncali et al. from being bilateral and depending on two different pedicles for smaller flaps than one pedicle for larger flaps [39]. We have not seen any perfusion problem because the digital artery and its branches are more than enough for such a small flap. As the dorsal side of the finger is left intact, there is no venous congestion on the finger’s tip which is a big deal in island and free flaps.
The patient could move his or her finger without any restriction immediately after the operation, which protects finger from stiffness. This is not the case in free flaps, island flaps, thenar flaps or groin flaps, which needs immobilisation, and in volar advancement flap where flexion deformity usually occurs. Due to non-affected finger movement, patients do not need physical therapy and could return their work after suture removal.
Triangle defects, left after flap transfer, are smaller than 0.5 cm2. They are left to secondary intention and able to heal in 3 to 5 days. As patients are seen every other day until suture removal, extra doctor visits for defects’ dressings are not necessary. Similar to other flaps, it gives a well-padded tissue, but in addition, pulp bears an excellent sensation. Owing to digital nerve presence in flaps, regardless of pulpa scar, none of the patients had pain, hypoesthesia, cold intolerance or scar hypersensitivity. Although the hand is the second most conspicuous part of the body after the face [32], we think that our method restores good aesthetic appearance of the fingertip.
Our method’s advantages are as follows:
It covers the defect with adjacent tissue in a single operation,
It is simple, quick and could be done under local anaesthesia,
It preserves the finger length while providing a well-padded, durable tip with tactile gnosis for pinching and nail growth,
It protects joint range of motion by not necessitating any splint,
Acceptable cosmetic appearance,
It assures early return to work.
Conclusion
Additional to the various and versatile fingertip reconstruction methods, we want to present V–Y rotation advancement flap as a quick, reliable and aesthetic method.
References
- 1.Alagoz MS, et al. Reverse homodigital artery flap coverage for bone and nailbed grafts in fingertip amputations. Ann Plast Surg. 2006;56(3):279–283. doi: 10.1097/01.sap.0000200086.24613.da. [DOI] [PubMed] [Google Scholar]
- 2.Allen MJ. Conservative management of finger tip injuries in adults. Hand. 1980;12(3):257–265. doi: 10.1016/S0072-968X(80)80049-0. [DOI] [PubMed] [Google Scholar]
- 3.Argamaso RV. V–Y–S-plasty for closure of a round defect. Plast Reconstr Surg. 1974;53(1):99–101. doi: 10.1097/00006534-197401000-00025. [DOI] [PubMed] [Google Scholar]
- 4.Atasoy E, et al. Reconstruction of the amputated finger tip with a triangular volar flap. A new surgical procedure. J Bone Joint Surg Am. 1970;52(5):921–926. [PubMed] [Google Scholar]
- 5.Bene MD, et al. Reverse dorsal digital island flap. Plast Reconstr Surg. 1994;93(3):552–557. doi: 10.1097/00006534-199493030-00017. [DOI] [PubMed] [Google Scholar]
- 6.Borman H, Maral T. The gluteal fasciocutaneous rotation-advancement flap with V–Y closure in the management of sacral pressure sores. Plast Reconstr Surg. 2002;109(7):2325–2329. doi: 10.1097/00006534-200206000-00025. [DOI] [PubMed] [Google Scholar]
- 7.Cohen BE, Cronin ED. An innervated cross-finger flap for fingertip reconstruction. Plast Reconstr Surg. 1983;72(5):688–697. doi: 10.1097/00006534-198311000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Alwis W. Fingertip injuries. Emerg Med Australas. 2006;18(3):229–237. doi: 10.1111/j.1742-6723.2006.00851.x. [DOI] [PubMed] [Google Scholar]
- 9.Deglise B, Botta Y. Microsurgical free toe pulp transfer for digital reconstruction. Ann Plast Surg. 1991;26(4):341–346. doi: 10.1097/00000637-199104000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Dellon AL. The proximal inset thenar flap for fingertip reconstruction. Plast Reconstr Surg. 1983;72(5):698–704. doi: 10.1097/00006534-198311000-00022. [DOI] [PubMed] [Google Scholar]
- 11.Demir Z, Velidedeoglu H, Celebioglu S. V–Y–S plasty for scalp defects. Plast Reconstr Surg. 2003;112(4):1054–1058. doi: 10.1097/01.PRS.0000076394.39302.9F. [DOI] [PubMed] [Google Scholar]
- 12.Furlow LT., Jr V–Y “cup” flap for volar oblique amputation of fingers. J Hand Surg Br. 1984;9(3):253–256. doi: 10.1016/0266-7681(84)90036-6. [DOI] [PubMed] [Google Scholar]
- 13.Henry M, Stutz C. Homodigital antegrade-flow neurovascular pedicle flaps for sensate reconstruction of fingertip amputation injuries. J Hand Surg Am. 2006;31(7):1220–1225. doi: 10.1016/j.jhsa.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 14.Hirase Y. Salvage of fingertip amputated at nail level: new surgical principles and treatments. Ann Plast Surg. 1997;38(2):151–157. doi: 10.1097/00000637-199702000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Holm A, Zachariae L. Fingertip lesions. An evaluation of conservative treatment versus free skin grafting. Acta Orthop Scand. 1974;45(3):382–392. doi: 10.3109/17453677408989160. [DOI] [PubMed] [Google Scholar]
- 16.Hong JP, et al. Reconstruction of fingertip and stump using a composite graft from the hypothenar region. Ann Plast Surg. 2003;51(1):57–62. doi: 10.1097/01.SAP.0000054340.77574.D8. [DOI] [PubMed] [Google Scholar]
- 17.Hueston J. Local flap repair of fingertip injuries. Plast Reconstr Surg. 1966;37(4):349–350. doi: 10.1097/00006534-196604000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Ishikawa K, Ogawa Y, Soeda H, Yoshida Y. A new classification of the amputation level for the distal part of the finger. J Jpn Soc Microsurg. 1990;3:54–62. [Google Scholar]
- 19.Karamursel S, Celebioglu S. Reverse-flow first dorsal metacarpal artery flap for index fingertip reconstruction. Ann Plast Surg. 2005;54(6):600–603. doi: 10.1097/01.sap.0000164527.28417.bf. [DOI] [PubMed] [Google Scholar]
- 20.Karamursel S, et al. Dorsal visor flap in fingertip reconstruction. Plast Reconstr Surg. 2001;108(4):1014–1018. doi: 10.1097/00006534-200109150-00033. [DOI] [PubMed] [Google Scholar]
- 21.Kayikcioglu A, et al. Arterialized venous dorsal digital island flap for fingertip reconstruction. Plast Reconstr Surg. 1998;102(7):2368–2372. doi: 10.1097/00006534-199812000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Koshima I, et al. Fingertip reconstructions using partial-toe transfers. Plast Reconstr Surg. 2000;105(5):1666–1674. doi: 10.1097/00006534-200004050-00011. [DOI] [PubMed] [Google Scholar]
- 23.Koshima I, et al. Digital artery perforator flaps for fingertip reconstructions. Plast Reconstr Surg. 2006;118(7):1579–1584. doi: 10.1097/01.prs.0000232987.54881.a7. [DOI] [PubMed] [Google Scholar]
- 24.Koshima I, et al. Perforator flaps and supermicrosurgery. Clin Plast Surg. 2010;37(4):683–689. doi: 10.1016/j.cps.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 25.Kutler W. A new method for finger tip amputation. J Am Med Assoc. 1947;133(1):29. doi: 10.1001/jama.1947.62880010007007. [DOI] [PubMed] [Google Scholar]
- 26.Lai CS, et al. The adipofascial turn-over flap for complicated dorsal skin defects of the hand and finger. Br J Plast Surg. 1991;44(3):165–169. doi: 10.1016/0007-1226(91)90119-5. [DOI] [PubMed] [Google Scholar]
- 27.Lai CH, et al. Free medial plantar artery perforator flaps for the resurfacing of thumb defects. Ann Plast Surg. 2010;65(6):535–540. doi: 10.1097/SAP.0b013e3181d376df. [DOI] [PubMed] [Google Scholar]
- 28.Laoulakos DH, et al. The dorsal reverse adipofascial flap for fingertip reconstruction. Plast Reconstr Surg. 2003;112(1):121–125. doi: 10.1097/01.PRS.0000066165.23202.45. [DOI] [PubMed] [Google Scholar]
- 29.Lassner F, et al. Sensory reconstruction of the fingertip using the bilaterally innervated sensory cross-finger flap. Plast Reconstr Surg. 2002;109(3):988–993. doi: 10.1097/00006534-200203000-00029. [DOI] [PubMed] [Google Scholar]
- 30.Lee JY, Teoh LC, Seah VW. Extending the reach of the heterodigital arterialized flap by cross-finger transfer. Plast Reconstr Surg. 2006;117(7):2320–2328. doi: 10.1097/01.prs.0000218872.01792.33. [DOI] [PubMed] [Google Scholar]
- 31.Lee DC, et al. Partial second toe pulp free flap for fingertip reconstruction. Plast Reconstr Surg. 2008;121(3):899–907. doi: 10.1097/01.prs.0000299945.03655.0d. [DOI] [PubMed] [Google Scholar]
- 32.Manske PR. Aesthetic hand surgery. J Hand Surg Am. 2002;27(3):383–384. doi: 10.1053/jhsu.2002.33938. [DOI] [PubMed] [Google Scholar]
- 33.Moberg E. Aspects of sensation in reconstructive surgery of the upper extremity. J Bone Joint Surg Am. 1964;46:817–825. [PubMed] [Google Scholar]
- 34.Pederson WC. Replantation. Plast Reconstr Surg. 2001;107(3):823–841. doi: 10.1097/00006534-200103000-00027. [DOI] [PubMed] [Google Scholar]
- 35.Rose EH, et al. The “cap” technique: nonmicrosurgical reattachment of fingertip amputations. J Hand Surg Am. 1989;14(3):513–518. doi: 10.1016/S0363-5023(89)80014-0. [DOI] [PubMed] [Google Scholar]
- 36.Russell RC, Casas LA. Management of fingertip injuries. Clin Plast Surg. 1989;16(3):405–425. [PubMed] [Google Scholar]
- 37.Sungur N, et al. V–Y rotation advancement fasciocutaneous flap for excisional defects of pilonidal sinus. Plast Reconstr Surg. 2006;117(7):2448–2454. doi: 10.1097/01.prs.0000219170.74059.94. [DOI] [PubMed] [Google Scholar]
- 38.Takeishi M, et al. Innervated reverse dorsal digital island flap for fingertip reconstruction. J Hand Surg Am. 2006;31(7):1094–1099. doi: 10.1016/j.jhsa.2006.02.029. [DOI] [PubMed] [Google Scholar]
- 39.Tuncali D, et al. The hatchet flap for reconstruction of fingertip amputations. Plast Reconstr Surg. 2006;117(6):1933–1939. doi: 10.1097/01.prs.0000209916.36072.c7. [DOI] [PubMed] [Google Scholar]
- 40.Unlu RE, et al. Dorsal adipofascial turn-over flap for fingertip amputations. J Hand Surg Br. 1999;24(5):525–530. doi: 10.1054/jhsb.1999.0223. [DOI] [PubMed] [Google Scholar]
- 41.Uysal A, et al. An alternative technique for microsurgically unreplantable fingertip amputations. Ann Plast Surg. 2006;57(5):545–551. doi: 10.1097/01.sap.0000226944.08332.41. [DOI] [PubMed] [Google Scholar]
- 42.Xu JH, et al. Linguiform rotation flap for amputations of the fingertip. Scand J Plast Reconstr Surg Hand Surg. 2007;41(6):320–325. doi: 10.1080/02844310701546896. [DOI] [PubMed] [Google Scholar]
- 43.Yeo CJ, Sebastin SJ, Chong AK. Fingertip injuries. Singapore Med J. 2010;51(1):78–86. [PubMed] [Google Scholar]
- 44.Yildirim S, et al. Complications of the reverse homodigital island flap in fingertip reconstruction. Ann Plast Surg. 2002;48(6):586–592. doi: 10.1097/00000637-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 45.Yoshimura M, et al. The venous skin graft method for repairing skin defects of the fingers. Plast Reconstr Surg. 1987;79(2):243–250. doi: 10.1097/00006534-198702000-00016. [DOI] [PubMed] [Google Scholar]