Dear Editor:
Introduction
Several studies based on hospital billing codes showed an increase in the number of hospital stays involving pressure ulcers by nearly 80% between 1993 and 2006.1–4 The newly developed flax dressings (FlaxAid) were used to treat decubitus ulcers in this clinical study. It has been discovered that genetic engineering methods can be used to enrich bandages in particular antioxidant substances that promote healing in the wound bed.5 The highly hygroscopic linen fibers keep the ulcer at its optimal moisture level by absorbing the excess of exudates, and reduce inflammation in the wound thanks to the high quantities of fenolic acids and flavonoids, which have antiallergenic, antiviral, antiinflammatory, and vasodilator activities6,7 and strengthen the wound tissue against stresses.8,9 This therapy consist of three elements: the linen layer, the oil emulsion, and the seedcake extract and was performed as part of a complex ulcer therapy regime that included necrotic tissue debridement, infection control, nutritional support, physiotherapy, education about proper care, and analgesic and antiplatelet therapy.
Patient and Method
The patient was a 66-year-old male scientific worker (initials: JP). He had incurred a spinal cord injury in a car accident five years earlier, and has paresis of the low extremities, thus needing to use a wheelchair. He visited the surgery outpatient clinic due to nonhealing, lasting over 2 1/2 years, in the form of recurring bedsores in the region of his buttocks. The bedsores did not have accompanying pain. The wound pathophysiology was diagnosed based on the patient's medical history and a physical examination. His main complaints were: the large amount of exudates, meaning he had to change his dressings several times per day, the appearance of his back, his dependence on his family, and the discomfort in his sacral region. He found this last difficult to describe. The bedsores were surrounded with an erythematous area, and had irregular edges with several deep and penetrating rhagades, fibrin masses, and a large amount of exudates, but were without necrotic tissue or macroscopic features of infection. According to the patient's wife, over the 2 1/2 years the ulcer had become deeper and wider, despite local and general therapy.
Routine laboratory tests were performed on the patient during his first visit in order to assess his general state of health. Peripheral blood was collected in the morning after an overnight fast. The lab tests performed included a complete blood count with a differential chemistry profile including blood urea nitrogen, creatinine, uric acid, serum protein, C-reactive protein (CRP), fibrinogen, alanine aminotransferase, and aspartate aminotransferase; a lipid profile with total cholesterol, HDL cholesterol, LDL cholesterol and triglycerides; a coagulation profile with protrombine time (PT), activated partial tromboplastin time (APTT), and international normalized ratio (INR); the levels of fasting glucose and glycosylated hemoglobin; and a urinalysis. All of the results from these laboratory tests were in the range of the norm. The blood culture and ulcer culture, both of which were taken three times, were negative.
Treatment
The treatment period was divided into four stages, each lasting four weeks. The patient filled out a questionnaire the day before each weekly visit. During the visit a physician performed an evaluation of the ulcer, read the questionnaire, and prepared photographic and descriptive documentation. The ulcers were not measured because of the location of the bedsores and the wide range and irregular borders of the wounds.
In the zero (control) stage the patient's wounds were treated with cotton dressings and in the first with linen dressing, both wetted with an isotonic salt solution. The second stage involved treatment with linen dressings wetted with oil emulsion. At this stage the wounds were being supplied with polyunsaturated fatty acids and hydrophobic antioxidants, which should strengthen the plasma membranes and increase the antioxidant potential of the cells in the damaged area.10,11 In the third stage the wounds were treated with linen dressings wetted with a seedcake extract that contains a high quantity of antioxidants, mainly lignans, which increase the fibroblast proliferation.
All the dressings were changed every 24 hours; the first in each stage was applied by qualified hospital personnel. The patient's spouse changed the dressings thereafter, having been thoroughly instructed by a qualified nurse during the weekly visits.
The study was approved by the local bioethics committee. The patient was provided with written information on the purpose and design of the study.
Results
Several parameters were considered to evaluate the changes yielded by FlaxAid therapy: the wound exudate levels, the fibrin and granulation levels within the decubitus ulcers, and the sizes of the decubitus ulcers.
After the zero stage, slight but negative changes were observed in all the considered parameters, suggesting that the common treatment (cotton gauze wetted with an isotonic salt solution) has no positive impact on ulcer healing within four weeks.
After the first stage (dressings with isotonic salt solution), the patient's spouse noticed a decrease in the level of the exudates. This was confirmed by the examining physician. After four weeks (the end of the first stage), the ulcers had become shallower, a reduction in the wound size was observed, and there was a systematic decrease in the level of exudates and a slight decrease in the fibrin level.
After the second stage of treatment (dressings with emulsion), the bedsores were clean, with a disappearance of the fibrin, and the wound bed was dry: the bandages could be changed once per 24 hours. There was also a significant reduction in the size of the wounds, and the deep ulcerations within the bedsores had become shallower.
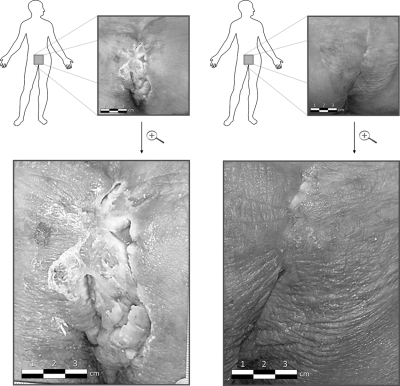
All of these effects were also visible in the third stage after which the decubitus ulcer was healed, with only a thin scar remaining, and the patient did not feel any discomfort (Figure 1).
FIG 1.
Photos of the bedsore in the region of the patient's buttocks before his inclusion in the study and after the 12-week treatment period.
In conclusion: after 12 weeks of the therapy, the patient's bedsores had been cured, and the patient only had to use skin grease and dry dressings, and change his sitting position several times per day when using his wheelchair.
Six months later at a follow-up appointment the bedsores were found to still be cured.
Acknowledgment
This study was supported by grant no. NR 12000906 from the Polish Ministry of Science and Education.
References
- 1.Russo CA. Steiner C. Spector W. Agency for Healthcare Research and Quality; Rockville, MD: Dec, 2008. [Jan 29;2009 ]. Hospitalizations related to pressure ulcers among adults 18 years, older, 2006. HCUP Statistical Brief #64. [PubMed] [Google Scholar]
- 2.Reddy M. Gill SS. Rochon PA. Preventing pressure ulcers: a systematic review. JAMA. 2006;296:974. doi: 10.1001/jama.296.8.974. [DOI] [PubMed] [Google Scholar]
- 3.Lyder CH. Pressure ulcer prevention and management. JAMA. 2003;289:223. doi: 10.1001/jama.289.2.223. [DOI] [PubMed] [Google Scholar]
- 4.Sopata M. Łuczak J. Prevention, treatment of pressure ulcers (part 1). Zakażenia. Klinika zakażeń szpitalnych. 2003;(4):81–88. [Google Scholar]
- 5.Arora A. Muraleedharan GN. Strasburg GM. Structure activity relationships for antioxidant activities of a series of flavonoids in a liposomal system. Free Radical Biol Med. 1998;9:1355–1363. doi: 10.1016/s0891-5849(97)00458-9. [DOI] [PubMed] [Google Scholar]
- 6.Wróbel M. Zebrowski J. Szopa J. Polyhydroxybutyrate synthesis in transgenic flax. J Biotech. 2004;107:41–54. doi: 10.1016/j.jbiotec.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 7.Lorenc-Kukuła K. Oszmiański J. Doermann P. Starzyki M. Skała J. Żuk M. Kulma A. Szopa J. Pleiotropic effect of phenolic compounds content increases in transgenic flax plant. J Agric Food Chem. 2005;53:3685–3692. doi: 10.1021/jf047987z. [DOI] [PubMed] [Google Scholar]
- 8.Harborne JB. Williams ChA. Advances in flavonoids research since 1992. Phytochemistry. 2000;55:481–504. doi: 10.1016/s0031-9422(00)00235-1. [DOI] [PubMed] [Google Scholar]
- 9.Lee JH. Shim JS. Lee JS. Kim JK. Yang IS. Chung MS. Kim KH. Inhibition of pathogenic bacterial adhesion by acidic polysaccharide from green tea (Camellia sinensis) J Agric. Food Chem. 2006;54:8717–8723. doi: 10.1021/jf061603i. [DOI] [PubMed] [Google Scholar]
- 10.Phan T'See P. GJR Chan S-Y. Lee ST. Phenolic compounds of Chromolaena odorata protect cultured skin cells from oxidative damage: implication for cutaneous wound healing. Biol Pharm Bull. 2001;24:1373–1379. doi: 10.1248/bpb.24.1373. [DOI] [PubMed] [Google Scholar]
- 11.Ruthin DJ. M-GKA Both (n-3) and (n-6) fatty acids stimulate wound healing in the rat intestinal epithelial cell line, IEC-6. J Nut. 1999;129:1791–1798. doi: 10.1093/jn/129.10.1791. [DOI] [PubMed] [Google Scholar]