ABSTRACT
Purpose: The objective of this study was to compare hospital and home care employers' rankings of both the importance and the feasibility of workforce strategies for recruiting and retaining rehabilitation professionals. Methods: An online self-administered questionnaire was distributed to all employers of rehabilitation professionals in Ontario hospitals (n=144) and Community Care Access Centre home care providers (n=34). Importance and feasibility rankings were based on the percentage of high ratings; 95% CIs were used to determine significant differences between hospital and home care rankings of recruitment and retention strategies. Results: The response rate was 50% (72/144) from hospitals and 73.5% (25/34) from home-care settings. The recruitment and retention strategies considered most important and feasible for rehabilitation therapists, regardless of setting, were communication between employer and worker, compensation packages, access to research, and professional development in budget planning. Tangible resources, support personnel, work safety, and marketing rehabilitation careers to high school students were ranked significantly higher by hospitals than by home care providers. Conclusions: Similarities exist between hospital and home care employers in terms of the importance and feasibility of recruitment and retention strategies for rehabilitation professionals. However, when developing a rehabilitation health human resources plan, the strategies identified as different between hospital and home care settings should be taken into account.
Key Words: health manpower, home care services, rehabilitation, personnel selection
RÉSUMÉ
Objectif : L'objectif de cette étude était de comparer la place accordée par les centres hospitaliers et les employeurs en soins à domicile à l'importance et à la faisabilité d'une stratégie de recrutement et de rétention des professionnels en réadaptation. Méthode : Un questionnaire en ligne a été envoyé à tous les employeurs de professionnels de la réadaptation dans les hôpitaux de l'Ontario (n=144) et aux fournisseurs de soins à domicile des Centres d'accès aux soins communautaires (n=34). Les classements de l'importance et de la faisabilité étaient établis à partir de pourcentages de classement élevés; des intervalles de confiance de 95 % ont été utilisés et ont permis de constater des différences considérables entre les classements accordés par les hôpitaux et ceux obtenus dans le secteur des soins à domicile. Résultats : Le taux de réponse au questionnaire a été de 50 % (72/144) pour les hôpitaux et de 73,5 % (25/34) pour les établissements de soins à domicile. Les stratégies de recrutement et de rétention considérées comme étant les plus importantes et les plus réalisables pour les thérapeutes en réadaptation, sans égard au milieu de pratique, sont la communication entre employeur et travailleur, les forfaits de rémunération, l'accès à la recherche et le développement professionnel dans la planification budgétaire. Des ressources concrètes, du personnel de soutien, la sécurité au travail et le marketing des carrières en réadaptation auprès des élèves du secondaire se sont classés à des rangs beaucoup plus élevés dans les hôpitaux et du côté des fournisseurs de soins à domicile. Conclusions : Des similitudes existent dans la perception des employeurs en centre hospitalier et des fournisseurs de soins à domicile de l'importance et de la faisabilité de stratégies de recrutement et de rétention des professionnels en réadaptation. Toutefois, au moment d'élaborer un plan de ressources humaines en réadaptation, les stratégies identifiées comme différentes entre les hôpitaux et les fournisseurs de soins à domicile devraient être prises en compte.
Mots clés : recrutement, rétention, stratégies de ressources humaines, réadaptation, hôpitaux, soins à domicile
Recruiting and retaining rehabilitation professionals is considered to be challenging all over the world; in Canada, Ontario is projected to face the most difficulty because of its growing population.1–6 Rehabilitation services in publicly funded organizations such as hospitals and home care, the two main employers of rehabilitation therapists, have undergone major reforms in Ontario, and these reforms have affected both the availability of health care providers and service provision. For example, an environmental scan7 by the Ontario Hospital Association in October 2004 indicated that rehabilitation professionals, including occupational therapists, physiotherapists, and speech–language pathologists, were among the top 10 job listings for which hospitals reported recruitment difficulties. Similarly, funding for home care has not kept up with the increased need for service, thanks to deficit-cutting policy reforms around de-institutionalization and hospital restructuring.8
In 1995, a new organization for coordinating community or home care services, known as Community Care Access Centres (CCACs), was given the responsibility of contracting out services in Ontario through a staged competitive process called “managed competition.”9 Findings from the November 2004 survey of Ontario Physiotherapy Association members working in home care indicated that 19% of respondents did not want to continue in the home care sector because they felt that client access to care had decreased, the quality of physiotherapy had decreased, and their jobs were not secure.10 Another survey, conducted by the Ontario Association of Speech-Language Pathology and Audiologists in 2001, revealed that 59 of 87 speech–language pathology members (68%) reported recruitment as a problem, but, more important, 47% identified it as a long-standing crisis and 42% indicated that retention was also a problem.11 More recently, in 2006, the American Physical Therapy Association reported similar difficulties: the vacancy rate for physiotherapist positions was 13.8%, and, on average, most hospitals took between 61 and 180 days to fill a vacancy.12 Similarly, in the 2005 Speech-Language Pathology Health Care survey,13 48% of respondents (122 of 253) indicated that they had funded but unfilled positions for speech–language pathologists in their agency.
Although labour-market demand and supply are influential in recruitment and retention decisions, developing strategies requires an understanding of conceptual frameworks or theories to categorize and explain how other underlying factors affect health care workers' mobility. For example, Lehmann and colleagues'14 model describes how health workers' decisions to accept and remain in public sector positions in remote areas depend on two interrelated aspects: the impact of different environments (individual, local, work, national, and international) and location of decision makers (local government, ministry of health, human resources directorate, public service, and other ministries). Behavioural and social science models, such as those explained by Tett and Meyer,15 show that job satisfaction and organizational commitment contribute independently to predicting intention to resign (turnover), and job satisfaction is a stronger predictor than organizational commitment. On the basis of this notion, considerable research has been devoted to identifying factors that affect job satisfaction among rehabilitation professionals. Although there is no single agreed-on model of job satisfaction, a variety of theoretical models have been studied to explain concepts and relationships associated with overall job satisfaction. The two most commonly used theories of job satisfaction for rehabilitation professionals are Herzberg and colleagues'16 motivation-hygiene theory and Mottaz's17 concepts of work values and work rewards.
Herzberg and colleagues'16 motivation-hygiene theory, also known as the two-factor theory of motivation, has been used in several rehabilitation studies18–22 to explain associations among motivation, job satisfaction, and retention factors among occupational therapists, physiotherapists, and speech–language pathologists. Herzberg and colleagues16 explained that two types of incidents occurred at people's jobs: one type that made them feel good or satisfied and another that made them feel bad or dissatisfied. According to this model, achievement, recognition, work itself, responsibility, advancement, and personal growth, referred to as motivators, lead to feelings of satisfaction; extrinsic factors such as work conditions, company policies, supervision, interpersonal work relations, salary, and job security, known as hygiene factors, prevent dissatisfaction. Because motivators directly affect a person's motivational drive to do a good job, they are believed to be more important than hygiene factors.
Mottaz,17 however, accounted for individual differences in job satisfaction among workers on the basis of two dimensions: work rewards and work values. Work rewards are perceived characteristics of the job and fall into three conceptual clusters: task, social, and organizational rewards. Mottaz described task rewards (intrinsic) as having five independent characteristics—skill variety, task identity, task significance, autonomy, and feedback—and include interesting and challenging work, self-direction and responsibility, creativity, opportunities to use one's skills, and feedback. Social rewards (extrinsic), however, are derived from interpersonal relationships established with others at work; having supportive colleagues and supervisors is an example of the social rewards of work. Last, organizational rewards (extrinsic) are tangible rewards provided by the employer or organization to facilitate performance, including working conditions, pay and fringe benefits, career advancement, and security. The second dimension of job satisfaction is based on work values, meaning the importance that individuals place on their work rewards.17 For example, some rehabilitation therapists may value extrinsic rewards such as pay and benefits over intrinsic factors such as clinical autonomy and challenging work. Although the conceptual frameworks of Herzberg and colleagues16 and Mottaz are organized differently, the job satisfaction variables of the two models are very similar (i.e., work conditions, pay, interpersonal relationships), and they both classify these factors as having intrinsic or extrinsic elements.
Despite the growing body of literature on recruitment and retention factors in various industries, there has been little study of these factors among rehabilitation professionals specifically. One published study, however, did look at the effects of extrinsic and intrinsic job satisfaction factors on recruitment and retention of rehabilitation professionals.21 According to the results of that study, occupational therapists and physiotherapists felt that intrinsic factors, such as professional growth and having a work environment in line with personal values, were more significant (p<0.01) than extrinsic factors such as pay and continuing education in predicting career satisfaction. The same intrinsic factors are also significant in predicting retention in rehabilitation professionals. Another study,23 looking at recruitment and retention of allied health professionals in rural areas in New South Wales, Australia, found that the main reasons people liked working in rural areas were the attractive environment and helpful team members; at the same time, 82% of employees (25 of 31) reported that having their spouse or partner move away was the number one reason for leaving a rural job. A similar study was conducted among occupational therapists and physiotherapists in northwestern Ontario;24 findings from that study indicated that factors contributing to an initial decision on location of practice include availability of leisure and recreation activities, proximity of family origin, and influence of spouse or partner. Study results also showed that the main reasons therapists left their jobs were a desire to be closer to family, lack of job opportunity, and spousal influence.
Simply understanding factors that influence recruitment and retention decisions is not sufficient for the development of a health human resource (HHR) plan for rehabilitation professionals. The most important and feasible workforce strategies need to be identified if the plan is to be effective and sustainable in addressing these factors. However, literature on HHR planning, recruitment, and retention strategies for rehabilitation professionals is lacking, because significant gaps exist in the availability of current and reliable data on supply, demand, and trends in the labour force participation of rehabilitation therapists.25–27 In an earlier study, therefore, we identified recruitment and retention strategies from the literature and then determined which strategies are important and feasible in the development of an HHR plan for rehabilitation professionals in Ontario, using an expert panel consensus process.28 Findings from the expert panels indicated that the four main areas of focus for recruitment and retention are quality of work life and work environment, workload and skill mix, financial incentives and marketing, and professional development. Workplace setting is among the key factors that need to be considered before strategy implementation; however, no studies have examined its effects on recruitment and retention of rehabilitation professionals. This study presents a workplace setting comparison of the ranking of importance and feasibility of rehabilitation recruitment and retention strategies in hospital and home care settings in Ontario, Canada, from the employer's perspective.
METHODS
This was a cross-sectional study using a self-administered online questionnaire. Study participants were people in hospitals and home care organizations who were responsible for the hiring of rehabilitation personnel.
Participant Recruitment and Survey Procedures
Included in the study were hospitals classified as Ontario hospital corporations and home care organizations that had contracts with the CCACs. The inclusion criteria required that an organization use at least one of the three types of rehabilitation therapists (occupational therapists, physiotherapists, and speech–language pathologists). Home care agencies for which the owner was the sole provider of rehabilitation services were excluded from the study. According to the public information available on the Ontario Ministry of Health and Long-Term Care Web site, there were 149 Ontario hospital corporations at the time of data collection;29 the Ontario Association of Community Care Access Centres Web site listed 45 home care agencies delivering occupational therapy, physiotherapy, or speech–language pathology services.30 Once study approval was received from the Research Ethics Board at the University of Toronto, each organization was contacted by telephone to investigate whether they used rehabilitation professionals and to inquire about the person most suitable to complete the survey. For organizations that met the inclusion criteria, the investigator contacted each nominee to establish his or her interest and ensure that the participant had access to the Internet to complete the online survey. All potential participants were e-mailed a study information letter explaining the purpose, risks, and benefits of the study along with an informed consent form that was faxed back to us. A numerical code assigned to each survey was used to track non-respondents and send reminder notices. Participants had approximately 3 weeks to complete the survey; an e-mail or phone reminder was sent at 2 weeks and another reminder was sent 48 hours before the survey deadline.
Questionnaire
Before dissemination, the questionnaire was field tested for readability and clarity. The questionnaire had three sections: (1) respondent profile, (2) organization profile, and (3) rehabilitation workforce strategies. Section 1 asked respondents to describe their demographic information, including age, group, gender, job title, description of global job responsibilities, years in current position, professional title (if applicable), and highest level of education completed. Section 2 included questions related to type of organization (i.e., hospital or home care service provider), geographic location, rehabilitation recruitment and retention difficulties, number of rehabilitation employees, and number of vacant full-time equivalent positions. Section 3 listed 23 recruitment and retention strategies identified from the literature and selected by HHR expert panels as both highly important and feasible in the development of a rehabilitation HHR plan in Ontario.28 Because most strategies were identified from grey literature, it was not surprising that no a priori peer-reviewed conceptual framework reflected the breadth of the strategies identified from the literature review. As a result, the themes used by the Health and Community Services Human Resources Sector Study in Newfoundland and Labrador formed the organizational framework for this study, because they aligned most closely with the identified strategies.31 The strategies were organized into four themes: (1) quality of work life and work environment (eight strategies); (2) workload and skill mix (two strategies); (3) financial incentives and marketing (six strategies); and (4) professional development (seven strategies). Importance and feasibility of workforce strategies were rated on a 9-point Likert scale (1=none, 9=maximum). Importance was defined as how valuable, appropriate, and useful the strategy would be for the development of a rehabilitation HHR plan in Ontario; feasibility required respondents to consider the practicality and cost implications of the strategy. Participants were also given the opportunity to indicate other workforce strategies currently in use that the questionnaire did not address.
Data Analysis
Demographic and organization information were entered into a spreadsheet and tabulated. The rating of each recruitment and retention strategy was based on the Rand/University of California, Los Angeles, appropriateness method:32 The ranking of each strategy was determined by the proportion of organizations that gave it a high rating (7, 8, or 9). For example, the highest-ranked strategy for importance or feasibility would be the strategy to which the largest proportion of organizations assigned a score of 7 or more. To determine statistically significant differences in strategy rankings between hospital and home care, 95% CIs were calculated for each proportion. Strategies with a non-overlapping 95% CI between the two groups were considered significantly different. The same analysis was used to determine significant differences between different types of hospitals (i.e., teaching vs. community and rehabilitation vs. non-rehabilitation). Fisher's exact test was used to compare proportions of other independent variables such as gender, age groups, and type of hospital (i.e., teaching, community, rehabilitation, and non-rehabilitation). All analyses were performed using the statistical software package SAS (version 9; SAS Institute, Cary, NC).
RESULTS
Sample
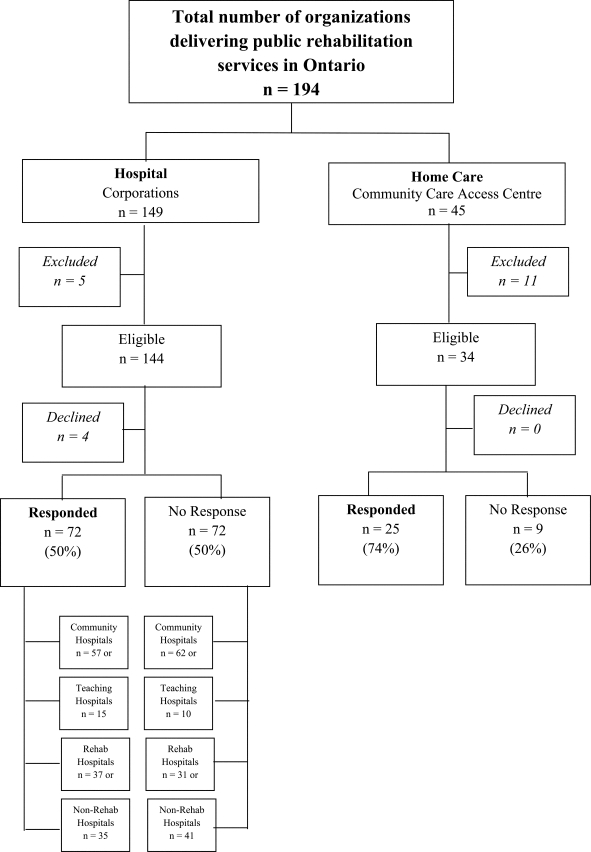
Of 149 hospital corporations, 144 were eligible for the study. Five hospital corporations were excluded: One hospital used only one part-time physiotherapist; two had other hospitals conduct their rehabilitation recruitment; one did not hire any rehabilitation professionals; and the individual responsible for hiring rehabilitation personnel was away indefinitely. Of the 144 eligible hospitals, 4 (2.8%) declined to participate, and no response was obtained from 72 hospital corporations, yielding a 47.2% response rate. Of the 45 home care agencies, 11 were excluded because the agency owner was the sole rehabilitation provider. Of the 34 home care organizations that met the inclusion criteria, 25 responded to the survey, yielding a response rate of 73.5%. Figure 1 illustrates this process.
Figure 1.
Data-collection flowchart.
Respondents were predominantly female in both settings (hospital=84.8%; home care=100%). Demographic characteristics of the participants and organizations are given in Table 1. No statistically significant differences were found between hospital and home care respondents in terms of gender, age group, or professional group, but more respondents were in management roles in home care (87.5%) than in hospitals (55.1%). The ratio of respondents versus non-respondents was fairly equal among all types of hospitals (teaching, community, rehabilitation, and non-rehabilitation). Not all respondents answered the demographic section of the survey; therefore, these findings should be interpreted with caution.
Table 1.
Characteristics of Respondents
| No. (%) of respondents* |
||
|---|---|---|
| Characteristic | Hospital; n=69 | Home care; n=24 |
| Sex | ||
| Female | 56 (84.8) | 24 (100) |
| Male | 10 (15.2) | 0 |
| Age, y | ||
| 20–39 | 19 (28.8) | 7 (30.4) |
| 40–49 | 28 (42.4) | 7 (30.4) |
| ≥50 | 19 (28.8) | 9 (39.1) |
| Job title | ||
| Management | 38 (55.1) | 21 (87.5) |
| Human resources officer | 22 (31.9) | 3 (12.5) |
| Clinician | 9 (13.0) | 0 |
| Years in current position | ||
| Management | ||
| <1 | 2 (5.3) | 1 (5.0) |
| 1– 5 | 20 (52.6) | 7 (35.0) |
| >5 | 16 (42.1) | 12 (60.0) |
| Human resources officers | ||
| <1 | 1 (4.5) | 0 |
| 1–5 | 13 (59.1) | 3 (100) |
| >5 | 8 (36.4) | 0 |
| Clinicians | ||
| <1 | 0 | 0 |
| 1–5 | 8 (88.9) | 0 |
| >5 | 1 (11.1) | 0 |
| Profession (if applicable) | ||
| Occupational therapist | 2 (3.9) | 4 (25.0) |
| Physiotherapist | 21 (41.2) | 5 (31.3) |
| Speech–language pathologist | 10 (19.6) | 3 (18.8) |
| Other | 18 (35.3) | 4 (25.0) |
| Recruitment difficulties reported | ||
| No | 21 (31.3) | 4 (16.7) |
| Yes | 46 (68.7) | 20 (83.3) |
| Retention difficulties reported | ||
| No | 39 (57.4) | 13 (54.2) |
| Yes | 29 (42.6) | 11 (45.8) |
| No. of vacancies (FTEs) | ||
| Occupational therapist | 32 | 28 |
| Physiotherapist | 57 | 45 |
| Speech–language pathologist | 15 | 24 |
FTE=full-time equivalent.
Unless otherwise indicated.
Importance Rankings for Strategies
Table 2 illustrates the 23 strategy areas and the CIs for the proportion of hospital and home care organizations ranking each strategy as highly important (score ≥7). The three strategy areas ranked highest in importance among all hospital respondents, in order of ranking, were communication between employer and worker, work safety, and competitive wage compensation packages. Home care respondents also ranked communication between employer and worker as the most important strategy; however, congruence between employer and staff values and training and growth opportunities were ranked second and third. A significantly higher proportion of hospital employers than of home-care employers rated tangible resources, support personnel, increase high school student awareness of rehabilitation careers, and career paths as important.
Table 2.
Proportion of Hospital and Home Care Employers' Ranking of Each Strategy as Highly Important
| No. (%) of respondents; 95% CI |
||
| Strategy area | Hospitals | Home care |
|---|---|---|
| Communication between employer and worker | 72 (97.2); 90.3–99.7 | 25 (100); 86.3–100 |
| Work safety | 70 (97.1); 90.1–99.7 | 24 (75.0); 53.3–90.2 |
| Competitive compensation packages | 70 (92.9); 84.1–97.6 | 24 (87.5); 67.6–97.3 |
| Access to research information | 70 (91.4); 82.3–96.8 | 24 (87.5); 67.6–97.3 |
| Professional development in budget planning | 70 (91.4); 82.3–96.8 | 24 (87.5); 67.6–97.3 |
| Tangible resources* | 72 (90.3); 81.5–96.0 | 25 (60.0); 38.7–78.9 |
| Training and growth opportunities | 71 (90.1); 80.7–95.9 | 24 (91.7); 73.0–99.0 |
| Support personnel* | 70 (88.6); 78.7–94.9 | 24 (58.3); 36.6–77.9 |
| Personal safety | 70 (87.3); 77.3–94.0 | 24 (83.3); 62.6–95.3 |
| Increase high school student awareness of rehabilitation careers* | 70 (85.7); 75.3–92.9 | 24 (54.2); 32.8–74.5 |
| Congruence between employer and staff values | 70 (82.9); 75.6–88.7 | 24 (95.8); 78.9–99.9 |
| Preceptorship training | 70 (82.9); 75.6–88.7 | 24 (58.3); 43.2–72.4 |
| Rural and remote mentors | 69 (76.8); 65.1–86.1 | 24 (87.5); 67.6–97.3 |
| Percentage of payroll to professional development | 70 (75.7); 64.0–85.2 | 24 (58.3); 36.6–77.9 |
| Workplace audit | 70 (74.3); 62.4–84.0 | 24 (79.2); 57.9–92.9 |
| Community-based professional development | 70 (74.3); 62.4–84.0 | 24 (62.5); 40.6–81.2 |
| Caseload management database | 70 (72.9); 60.9–82.8 | 24 (70.8); 48.9–87.4 |
| Career paths* | 70 (72.9); 60.9–82.8 | 24 (33.3); 15.6–55.3 |
| Rural and remote orientation packages | 70 (72.9); 60.9–82.8 | 24 (87.5); 67.6–97.3 |
| Minimize rural and remote isolation | 70 (71.4); 59.4–81.6 | 24 (70.8); 48.9–87.4 |
| Increase public awareness of rehabilitation careers | 70 (70.0); 57.9–80.4 | 24 (54.2); 32.8–74.5 |
| Employer or workplace awards | 70 (48.6); 36.4–60.8 | 24 (37.5); 18.8–59.4 |
| Family relocation programs | 70 (30.0); 19.6–42.1 | 24 (29.2); 12.6–51.1 |
Non-overlapping 95% CI.
Comparing recruitment and retention strategies as a function of hospital facility type showed that, on one hand, respondents from community hospitals ranked work safety, communication between employer and worker, and training and growth opportunities as highest in importance. Teaching hospitals, on the other hand, ranked communication between employer and worker, competitive wage compensation packages, and access to research information as their top three. However, no statistically significant differences in rankings were found between these two settings. Similarly, importance rankings in rehabilitation and non-rehabilitation hospitals were comparable: work safety, communication between employer and worker, and professional development in budget planning were ranked among the top five strategies by respondents from both settings, but differences were not statistically significant. Interestingly, providing competitive wage compensation packages was ranked as one of the most important strategies among non-rehabilitation hospitals but ranked eighth among rehabilitation hospitals.
Feasibility Rankings for Strategies
Feasibility rankings for hospital and home care organizations are provided in Table 3. Among all hospital respondents, the three top-ranked strategy areas in terms of feasibility, in order of ranking, were communication between employer and worker, personal safety, and work safety. Similarly, communication between employer and worker was rated the most feasible strategy by home care employers, and congruence between employer and staff values and access to research information were ranked second and third. Three statistically significant differences in feasibility rankings were found between hospital and home care settings: work safety, support personnel, and increase high school student awareness of rehabilitation careers.
Table 3.
Proportion of Hospital and Home Care Employers' Ranking of Each Strategy as Highly Feasible
| No. (%) of respondents; 95% CI |
||
|---|---|---|
| Strategy area | Hospitals | Home care |
| Communication between employer and worker | 72 (90.3); 81.0–96.0 | 25 (100); 86.3–100 |
| Personal safety | 71 (87.3); 77.3–94.0 | 24 (79.2); 57.9–92.9 |
| Work safety* | 70 (87.1); 77.0–94.0 | 24 (54.2); 32.8–74.5 |
| Access to research information | 70 (82.9); 72.0–90.8 | 24 (83.3); 62.6–95.3 |
| Professional development in budget planning | 70 (81.4); 70.3–89.7 | 24 (75.0); 53.3–90.2 |
| Support personnel* | 70 (80.0); 68.7–88.6 | 24 (33.3); 15.6–55.3 |
| Increase high school student awareness of rehabilitation careers* | 70 (80.0); 68.7–88.6 | 24 (45.8); 25.6–67.2 |
| Congruence between employer and staff values | 70 (75.7); 64.0–85.2 | 24 (83.3); 62.6–95.3 |
| Training and growth opportunities | 70 (74.7); 62.9–84.2 | 24 (66.7); 44.7–84.4 |
| Competitive compensation packages | 70 (72.9); 60.9–82.8 | 24 (66.7); 44.7–84.4 |
| Tangible resources | 71 (66.7); 54.6–77.3 | 25 (48.0); 27.8–68.7 |
| Rural and remote orientation packages | 70 (65.7); 53.4–76.7 | 24 (79.2); 57.9–92.9 |
| Preceptorship training | 70 (64.3); 51.9–75.4 | 24 (41.7); 22.1–63.4 |
| Community-based professional development | 70 (62.9); 50.5–74.1 | 24 (70.8); 48.9–87.4 |
| Minimize rural and remote isolation | 70 (58.6); 46.2–70.2 | 24 (62.5); 40.6–81.2 |
| Workplace audit | 70 (55.7); 43.3–67.6 | 24 (66.7); 44.7–84.4 |
| Caseload management database | 70 (54.3); 41.9–66.3 | 24 (70.8); 48.9–87.4 |
| Rural and remote mentors | 69 (53.6); 41.2–65.7 | 24 (70.8); 48.9–87.4 |
| Increase public awareness of rehabilitation careers | 70 (51.4); 39.2–63.6 | 24 (41.7); 22.1–63.4 |
| Percentage of payroll to professional development | 70 (47.1); 35.1–59.5 | 24 (33.3); 15.6–55.3 |
| Employer and workplace awards | 70 (41.4); 29.8–53.8 | 24 (37.5); 18.8–59.4 |
| Career paths | 70 (37.1); 25.9–49.5 | 24 (20.8); 7.1–42.2 |
| Family relocation programs | 70 (17.1); 9.2–28.0 | 24 (12.5); 2.7–32.4 |
Non-overlapping 95% CI.
For community hospitals, the three top-ranked strategy areas in terms of feasibility were communication between employer and worker, personal safety, and work safety. Conversely, teaching hospitals ranked access to research information, communication between employer and worker, and work safety as the top three. Similar to the importance rankings, no statistically significant differences in feasibility rankings were found between these two practice settings. Only one statistically significant difference was observed between rehabilitation and non-rehabilitation settings: Although training/growth opportunities were ranked 11th by rehabilitation hospitals (62.2%; 95% CI, 44.8–77.5) in terms of feasibility, non-rehabilitation hospitals (88.2%; 95% CI, 78.1–94.8) ranked it second.
DISCUSSION
Several similarities were found between hospital and home care employers' rankings of the importance of recruitment and retention strategies for rehabilitation professionals. More than 75% of employers rated communication, compensation, research, professional development, training and growth opportunities, personal safety, organizational values, and work safety as highly important for the development of a rehabilitation HHR plan in Ontario. Of these strategies, however, only communication, personal safety, and professional development were rated as highly feasible by more than 75% of employers. Although no research has compared recruitment and retention strategies for rehabilitation professionals between hospitals and home care, some strategies were similar to retention strategies used for nurses. Leurer and colleauges33 conducted semi-structured interviews with 16 nurses from diverse practice settings (acute, long-term care, rehabilitation, and community hospitals and home health care agencies) in western Canada to investigate what retention strategies they would recommend to policymakers. Similar to our study, they found that consultation and communication with nurses and professional development were among the seven major themes commonly mentioned by participants. Likewise, our results from the home care setting were consistent with Randolph's21 study, in which investigators found that having a work environment in line with personal values is more significant in predicting career satisfaction and desire to stay on the job than extrinsic factors such as pay and continuing education.
Strategies for support personnel and increasing high school students' awareness of careers in rehabilitation were rated differently between practice settings: Hospital employers perceived these as significantly more important and more feasible than did home care employers. Although it was not within the scope of our study to identify the reasons for these disparities, other studies have identified factors that may explain them. For example, one study34 surveyed the use of physical therapist assistants in home health care agencies in New York 1 year after a legislative amendment (Bill 48-C, which in October 1993 amended the New York State Education Law to help alleviate the shortage of licensed physiotherapists by allowing physical therapy assistants to work in the home setting without direct on-site supervision). Results from this study demonstrated that despite the amendment, 32 of 39 agencies (82%) providing physical therapy, rehabilitative services, or both did not use physical therapy assistants. The most common factors contributing to the decision not to use support personnel, in order of highest frequency, were that (1) physical therapy assistants were too difficult to supervise, (2) physiotherapy staff were adequate, (3) physical therapy assistants were not qualified, and (4) physical therapy assistants were not cost-effective. Further research in this area is needed to identify whether these factors apply to the Ontario home care setting.
Respondents representing hospitals also considered ensuring that workers have the tangible resources (e.g., computers and specialized equipment, telephone systems, office space) to do their jobs more important and feasible than did home care employers. The same pattern was seen for improving and maintaining the safety of rehabilitation therapists by minimizing the susceptibility to work-related injury. However, although home-care employers ranked rural and remote strategies (i.e., rural and remote mentors and orientation packages; minimizing rural and remote isolation) among their top 10 strategies in terms of importance, the same strategies were ranked in the bottom 10 by hospital employers. This finding is consistent with those of Canadian studies examining factors affecting job turnover, attrition, and retention in rural and remote services among rehabilitation professionals.23,35–37 Beggs and Noh36 found that therapists working in community and hospital settings were more likely to consider relocation than those working in private practice. Retention factors including marital status, satisfaction with northern lifestyle (both self and spouse or partner), professional experience, and satisfaction with career opportunities demonstrated a direct relationship with intention to relocate. Perceived opportunity for career development was the most significant factor related to job turnover. The same authors conducted a follow-up study 2 years later that determined the predictive validity of variables identified in the initial study. Professional experience, practice location (hospital, community or private), and opportunity for career development were the only factors significant in predicting job turnover and regional attrition. The opportunity for career development continued to be the most significant predictor of job turnover and regional attrition. Similarly, Solomon and colleagues24 found that the top five sources of job dissatisfaction among all practising occupational therapists and physiotherapists in northwestern Ontario were lack of opportunity for continuing education; professional isolation; hours of work or clinical workload; lack of long-term security; and lack of opportunity for promotion. On the basis of our study's findings and those of previous research, developing rural and remote workforce strategies for rehabilitation therapists should be one of the priority areas in HHR planning.
Overall, quality of work life and work environment (i.e., communication, training and growth, safety) and professional development types of strategies (i.e., access to research) appear to be the most important and widely used in both types of workplace settings. Although nearly 90% of employers ranked providing a competitive compensation package as highly important in recruiting and retaining rehabilitation staff, fewer than 75% of respondents used this strategy, and even fewer considered it feasible. Findings from a U.S.-based study38 found that the most commonly used recruitment and retention strategies among occupational therapy directors were not reported to be the most effective or the most important: Although strategies relating to the work itself were the most important (i.e., conducting research and interpersonal staff member relationships), competitive salary, student internships, and student sponsorships were the most effective recruitment strategies overall. Similarly, although employee appraisals and continuing education were the most commonly used retention strategies, a supportive environment and competitive pay were the most effective in retaining staff. Despite the fact that most US health care facilities are privately funded and our study targeted publicly funded workplace settings in Canada, the strategies used were quite similar with the exception of compensation.
Our study has four main limitations. The response rate among hospital employers was only 50%, which may have introduced some bias. For example, hospitals with fewer recruitment or retention difficulties may have been less likely to participate. Therefore, to the extent that these non-respondents might have rated particular strategies as less important or less feasible than those hospitals that did respond, the between-group differences may be attenuated. In addition, the survey was not targeted to specific types of rehabilitation therapists, and hence study findings could not be generalized for each discipline (occupational therapy, physiotherapy, or speech–language pathology). All data are self-reported and therefore may not reflect actual practice in terms of strategy use. Not knowing the strategies' effectiveness in the recruitment and retention of rehabilitation professionals is a limitation.
Because geographic location was not taken into account, there may have been some confounding findings related to rural and remote strategies. Therefore, future studies should analyze the impact of rural and remote versus urban settings on the effectiveness of recruitment and retention strategies.
Last, although some strategies—such as competitive wage packages, training and growth opportunities and professional development—are viewed as incentives for both recruitment and retention, other strategies do not overlap and are appropriate for only one of the two tasks. Future researchers should therefore consider studying recruitment and retention strategies separately, so that a distinction between the two can be made.
CONCLUSION
To our knowledge, this study is the first to examine hospital and home care employers' perceptions of workforce strategies that should be used to recruit and retain rehabilitation therapists in the Canadian setting. The key important and feasible strategies identified for recruiting and retaining these professionals, regardless of setting, included communication between employer and worker, personal safety, access to research information, professional development, and congruence between employer and staff values. Despite these commonalities, future research should investigate why other strategies such as tangible resources, support personnel, work safety, and marketing rehabilitation careers to high school students are ranked higher in hospitals than in the home care setting, whereas strategies focusing on rural and remote areas, such as orientation packages, mentors, and minimizing isolation, are more important in home care settings than in hospitals.
If these strategies are to be implemented effectively, further research is needed to explore the relationship between feasibility and importance. Prioritizing these strategies for different workplace settings will enable employers to target the appropriate employees. This may not only reduce turnover and thus save money but also have a positive effect on patient outcomes by ensuring that staff have the appropriate knowledge to deliver optimum care. Furthermore, from a health care organization perspective, having the proper infrastructure and identifying who will be responsible for each strategy will support the development of a HHR plan for rehabilitation. Once these steps are in place, health care stakeholders can set benchmarks so that the outcomes of future planning activities can be evaluated and assessed for their efficiency and effectiveness.
KEY MESSAGES
What Is Already Known on This Topic
There have been several reports on HHR planning and recruitment and retention strategies for physicians and nurses; however, information related to rehabilitation professionals, and particularly occupational therapists, physiotherapists, and speech–language pathologists, is lacking. Rehabilitation services in publicly funded organizations such as hospitals and home care, the two main employers of rehabilitation therapists, have undergone major health care reform in Ontario, thereby affecting the availability of human health care resources and service provision. Findings from earlier studies have shown that key factors influencing recruitment and retention among rehabilitation professionals include quality of work life and work environment, workload and skill mix, financial incentives, marketing, and professional development. The importance and feasibility of these key factors in different workplace settings (hospital vs. home care) have not previously been compared.
What This Study Adds
Employers from both hospital and home-care settings considered communication between employer and worker, personal safety, access to research information, professional development, and congruence between employer and staff values the most important and feasible strategies for recruiting and retaining rehabilitation professionals. Despite these commonalities, however, hospital employers considered other strategies such as tangible resources, support personnel, work safety, and marketing rehabilitation careers to high school students to be more important and feasible than did their home care counterparts. Strategies focusing on rural and remote areas, such as orientation packages, mentors, and minimizing isolation, were considered to be more important and feasible in home care than in hospitals. Prioritizing these strategies for different workplace settings will not only target appropriate employees but increase recruitment and reduce therapist turnover.
Physiotherapy Canada 2012; 64(1);31–41; doi:10.3138/ptc.2010-43
References
- 1.Taylor L, Roigard A, Sung T, et al. The New Zealand physiotherapy workforce: an audit of current gaps and implications for future needs. New Zeal J Physiother. 2006;34(2):112–3. [Google Scholar]
- 2.Struber J. Recruiting and retaining allied health professionals in rural Australia: Why is it so difficult? [cited 2006 Jan 1];Int J Allied Health Sci Pract. 2004 Apr;2(2):8. Available from: http://ijahsp.nova.edu/articles/Vol2num2/pdf/Struber.pdf. [Google Scholar]
- 3.Devine S. Perceptions of occupational therapists practising in rural Australia: a graduate perspective. Aust Occup Ther J. 2006;53(3):205–10. [Google Scholar]
- 4.Powell JM, Griffith SL, Kanny EM. Occupational therapy workforce needs: a model for demand-based studies. Am J Occup Ther. 2005;59(4):467–74. doi: 10.5014/ajot.59.4.467. Medline:16124213. [DOI] [PubMed] [Google Scholar]
- 5.Rossiter D. Recruitment and retention: the black and white picture. Royal Coll Speech Lang Therapists Bull. 2000;579:12–4. [Google Scholar]
- 6.Landry MD, Rickettes TC, Verrier MC. The precarious supply of physical therapists across Canada: exploring national trends in health human resources (1991 to 2005) Hum Resour Health. 2007;5:23. doi: 10.1186/1478-4491-5-23. doi: 10.1186/1478-4491-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown S, Kang N. Environmental scan. Toronto: Provincial Health Human Resources Strategic Advisory Groups, Ontario Hospital Association; 2004. [Google Scholar]
- 8.Williams AM. Restructuring home care in the 1990s: geographical differentiation in Ontario, Canada. Health Place. 2006;12(2):222–38. doi: 10.1016/j.healthplace.2004.09.002. Medline:16338637. [DOI] [PubMed] [Google Scholar]
- 9.Vanderbent SD. Private sector delivery of home health care in Ontario [Internet] Toronto: Ontario Home Health Care Providers' Association (OHHCPA); 2001. [cited 2005 Dec 30]. Available from: http://www.homecareontario.ca/public/docs/papers/private-sector-delivery-of-home-health-care-in-ontario.pdf. [Google Scholar]
- 10.Alliance of Professional Associations for Community-Based Therapy Services (APACTS) Review of managed competition. Toronto (ON): Alliance of Professional Associations for Community-Based Therapy Services; 2004. [Google Scholar]
- 11.Ontario Association of Speech-Language Pathologists and Audiologists (OSLA) Recruitment and retention of speech-language pathologists and audiologists in Ontario. Toronto (ON): The Association; 2001. [Google Scholar]
- 12.American Physical Therapy Association. Physical therapy workforce project: physical therapy vacancy and turnover rates in acute care hospitals [Internet] Alexandria (VA): The Association; 2008. [cited 2008 Sept 8]. Available from: http://www.apta.org/AM/Template.cfm?Section=Physical_Therapy_Workforce & Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=48&ContentID=46693. [Google Scholar]
- 13.American Speech-Language-Hearing Association. SLP health care survey 2005 [Internet] Rockville (MD): The Association; 2005. [cited 2008 Sept 8]. Available from: http://www.asha.org/uploadedFiles/research/memberdata/HC05WorkforceRprt.pdf. [Google Scholar]
- 14.Lehmann U, Dieleman M, Martineau T. Staffing remote rural areas in middle- and low-income countries: a literature review of attraction and retention. BMC Health Serv Res. 2008;8:19. doi: 10.1186/1472-6963-8-19. http://www.biomedcentral.com/1472-6963/8/19 doi: 10.1186/1472-6963-8-19. Medline:18215313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tett RP, Meyer JP. Job satisfaction, organizational commitment, turnover intention, and turnover: Path analyses based on meta-analytic findings. Person Psychol. 1993;46(2):259–93. [Google Scholar]
- 16.Herzberg F, Mausner B, Snyderman B. The motivation to work. New York: Wiley; 1959. [Google Scholar]
- 17.Mottaz C. The relative importance of intrinsic and extrinsic rewards as determinants of work satisfaction. Sociol Q. 1985;26:365–85. [Google Scholar]
- 18.Bordieri JE. Job satisfaction of occupational therapists: supervisors and managers versus direct service staff. Occup Ther J Res. 1988;8(3):155–63. [Google Scholar]
- 19.Moore K, Cruickshank M, Haas M. Job satisfaction in occupational therapy: a qualitative investigation in urban Australia. Aust Occup Ther J. 2006;53(1):18–26. [Google Scholar]
- 20.Thornton M, Melis EH, Pham B. Development, implementation and results of a survey to identify factors affecting motivation in an acute care physiotherapy setting. Physiother Can. 1999;51(4):251–8. [Google Scholar]
- 21.Randolph DS. Predicting the effect of extrinsic and intrinsic job satisfaction factors on recruitment and retention of rehabilitation professionals. J Healthc Manag. 2005;50(1):49–60. discussion 60. Medline:15729907. [PubMed] [Google Scholar]
- 22.Davis GL, Bordieri JE. Perceived autonomy and job satisfaction in occupational therapists. Am J Occup Ther. 1988;42(9):591–5. doi: 10.5014/ajot.42.9.591. Medline:3189490. [DOI] [PubMed] [Google Scholar]
- 23.Denham LA, Shaddock AJ. Recruitment and retention of rural allied health professionals in developmental disability services in New South Wales. Aust J Rural Health. 2004;12(1):28–9. doi: 10.1111/j.1440-1584.2004.00546.x. Medline:14723778. [DOI] [PubMed] [Google Scholar]
- 24.Solomon P, Salvatori P, Berry S. Perceptions of important retention and recruitment factors by therapists in northwestern Ontario. J Rural Health. 2001;17(3):278–85. doi: 10.1111/j.1748-0361.2001.tb00965.x. Medline:11765892. [DOI] [PubMed] [Google Scholar]
- 25.Parker-Taillon D Associates. Moving forward with next steps in occupational therapy human resource planning [Internet]. Report. Ottawa (ON): Canadian Association of Occupational Therapists; 2004. Mar, [cited 2011 Jun 23]. Available from: http://www.caot.ca/pdfs/CAOT%20HHR%20Summary%20Report%20Final.pdf. [Google Scholar]
- 26.Parker-Taillon D. Physical therapy human resource planning and the regulatory role. Edmonton: College of Physical Therapists of Alberta; 2005. Background paper. [Google Scholar]
- 27.Canadian Association of Speech-Language Pathologists and Audiologists (CASPLA) Gap analysis: a study into the availability and accessibility of data to support long-term human resources planning for speech-language pathologists and audiologists [Internet]. Report. Ottawa (ON): The Association; 2004. Available from: http://www.caslpa.ca/PDF/CASLPA%20Gap%20Analysis%20%20March%202004%20v2.pdf. [Google Scholar]
- 28.Tran D, McGillis Hall L, Davis A, et al. Identification of recruitment and retention strategies for rehabilitation professionals in Ontario, Canada: results from expert panels. BMC Health Serv Res. 2008;8:249. doi: 10.1186/1472-6963-8-249. doi: 10.1186/1472-6963-8-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ministry of Health and Long-Term Care (MOHLTC) Health services in your community: hospital locations and classifications by region [Internet] Toronto: MOHLTC; 2006. [cited 2006 Nov 6]. Available from: http://www.health.gov.on.ca/english/public/contact/hosp/hosploc_mn.html. [Google Scholar]
- 30.Ontario Association of Community Care Access Centres (OACCAC) Listing of contracts and services operated by individual LHINs [Internet] Toronto (ON): The Association; [cited 2006 Nov 6]. Available from: http://www.ccac-ont.ca/OACCAC/Contracts.aspx?EnterpriseID=15&LanguageID=1&MenuID=78. [Google Scholar]
- 31.Harnett L, Coady R. Recruitment and retention in the health system [Internet]. Discussion paper. Newfoundland & Labrador Human Resource Planning Steering Committee, Health and Community Services Human Resources Sector Study; 2002. Jun 13, [cited 2011 Jun 23]. Available from: http://www.nlhba.nl.ca/hr/documents/recruit.pdf. [Google Scholar]
- 32.Fitch K, Berstein SJ, Aguilar MD, et al. The RAND/UCLA appropriateness method user's manual. Los Angeles (CA): RAND; 2001. [Google Scholar]
- 33.Leurer MD, Donnelly G, Domm E. Nurse retention strategies: advice from experienced registered nurses. J Health Organ Manag. 2007;21(3):307–19. doi: 10.1108/14777260710751762. Medline:17713190. [DOI] [PubMed] [Google Scholar]
- 34.Sherry D, Walsh K. The use of physical therapist assistants in home health care agencies in New York. Home Health Care Manage Pract. 1996;8(2):65–72. [Google Scholar]
- 35.Noh S, Beggs CE. Job turnover and regional attrition among physiotherapists in northern Ontario. Physiother Can. 1993;45(4):239–44. Medline:10130907. [PubMed] [Google Scholar]
- 36.Beggs CE, Noh S. Retention factors for physiotherapists in an underserviced area: an experience in northern Ontario. Physiother Can. 1991;43(2):15–21. Medline:10110595. [PubMed] [Google Scholar]
- 37.Polatajko H, Quintyn M. Factors affecting occupational therapy job site selection in underserviced areas. Can J Occup Ther. 1986;53(3):151–8. doi: 10.1177/000841748605300307. Medline:10277425. [DOI] [PubMed] [Google Scholar]
- 38.Smith P, Schiller MR, Grant HK, et al. Recruitment and retention strategies used by occupational therapy directors in acute care, rehabilitation, and long-term-care settings. Am J Occup Ther. 1995;49(5):412–9. doi: 10.5014/ajot.49.5.412. Medline:7598156. [DOI] [PubMed] [Google Scholar]