Abstract
Objective
To test a new program’s effectiveness in reducing depression’s work burden.
Methods
A brief telephonic program to improve work functioning was tested in an early-stage randomized controlled trial (RCT) involving 79 Maine State Government employees who screened-in for depression and at-work limitations (treatment group=59; usual care group=27). Group differences in baseline to follow-up change scores on The Work Limitations Questionnaire (WLQ), WLQ Absence Module and PHQ-9 depression severity scale were tested with analysis of covariance.
Results
While there were no baseline group differences (p≥.05), by follow-up the treatment group had significantly better scores on every outcome and differences in the longitudinal changes were all statistically significant (p=.0.27 to .0001).
Conclusions
The new program was superior to usual care. The estimated productivity cost savings are $6041.70 per participant annually.
INTRODUCTION
Working-age adults with depression experience higher than average rates of job loss, job turnover, premature retirement, work absences, and impaired work performance,(1–4) harming employees and their families and resulting in billions of dollars annually in lost productivity.(5–9) Clinical trials have shown that depression treatment can improve symptoms and reduce work productivity loss.(10–13) These studies have helped make the “business case” for high-quality depression treatment. However, treatment remains primarily symptom-focused, leaving work difficulties receiving considerably less attention.
Despite the secondary work benefits of high quality treatment, it is not enough to overcome the significant work disruption depression often causes.(14, 15) Workers can face difficulties both when symptomatic and after symptoms subside. Their ability to function effectively can be sabotaged by residual symptoms and incomplete recovery, suboptimal treatment efficacy or adherence, stigma, difficulty reestablishing good work habits after an episode, and organizational barriers to modifying work arrangements.
Taking cues from the care of chronic health problems such as musculoskeletal pain, in which return to effective functioning is regarded as an important goal, we considered that employees with depression may also benefit from work-focused care addressing the medical, psycho-social and environmental dimensions of functioning. Research has suggested several strategies.(16)
For example, studies of collaborative care (17–22) have shown that patient clinical outcomes are better when care is organized to support provider-patient teams with care manager involvement.(20, 23) Similarly, occupational medicine and disability research has shown that work injured or disabled employees return to work more quickly when medical providers, workplace managers and the employee collaborate.(16, 24) Together, these results imply that coordinated care involving mental health providers, the employee and other professionals closer to the work situation, such as employee assistance program (EAP) counselors or on-site health clinic staff, may bridge the gap between the medical and work domains.
Additionally, an extensive literature demonstrates the effectiveness of cognitive-behavioral therapy (CBT) in improving mental health and functioning. Because CBT can be provided as a brief intervention through in-person, telephonic or electronic modalities, it offers the flexibility to reach workers from a variety of occupations and industries.(13, 25, 26)
Finally, studies of supported employment for severely and chronically mentally ill adults and other persons with disabilities offer insights into the importance of achieving a “fit” between the person and the work environment. Methods of enhancing this fit have included job coaching, providing social supports and/or targeted work modifications (e.g., flexible scheduling).(27, 28)
Based on these and similar observations, a novel multi-component work-focused care program, named the Work and Health Initiative (WHI), was developed for employees with depression. An initial pilot-test (29) was conducted in a national aeronautics manufacturing firm, using a quasi-experimental pre-test post-test design with an external comparator. The results indicated that employees in the WHI program had statistically significant improvements in work performance and productivity.(14) The present study is an early-stage randomized control trial (RCT) of the WHI involving a public sector employer. It tests the hypothesis that compared to usual care for employees with depression the WHI will result in greater improvements in work performance and work productivity.
METHODS
Study Design & Participants
This study involved State Government in Maine and was conducted between October, 2007 and April, 2008. Email and print advertisements were distributed at work to attempt to reach approximately 13,000 employees, many of whom are dispersed throughout the state in a variety of work locations. Employees were invited to take a brief, anonymous eligibility screening survey for which they would receive immediate feedback about their health. The number of employees with a computer at the work location was estimated to be 10,400, which does not reflect actual accessibility during the workday.
Several precautions were taken to protect employee privacy. When employees were notified about the study, they were given the study website’s URL and invited to access it from a computer at work or home. On the website, the following additional privacy protections were described: the website was not integrated with existing websites operated by the employer or its vendors (e.g., medical insurance company); the website did not collect computer IP addresses; no attempt would be made to find out the identity of anyone accessing the website; and the protocol was reviewed and approved by the institutional review board overseeing from the academic medical center-based research team. Prior to taking the anonymous screener, each employee was asked to read and endorse a brief informed consent statement.
Upon receiving screener results electronically, eligible employees viewed an invitation to enroll in the RCT. Eligible employees were 18 to 62 years old and employed ≥15 hours per week, and fulfilled the criteria for current major depressive disorder (MDD) and/or dysthymia. MDD was indicated by five out of nine symptoms at qualifying levels on the Patient Health Questionnaire depression scale (PHQ-9) and no recent bereavement.(30, 31) The PHQ-9 was adapted from the clinician-administered PRIME-MD and has been shown to have sensitivity of 75% and specificity of 90%.(31, 32) Dysthymia was indicated by two qualifying symptoms on the validated PC-SAD.(33) Eligibility also required an at-work productivity loss of 5% or more in the past two weeks, as measured by the Work Limitations Questionnaire (WLQ) short-form.(34, 35) The WLQ items assess the degree of health-related difficulty experienced in the past two weeks performing specific job tasks. The WLQ was designed to elicit reports of limitations in ability to perform work tasks that are common to many jobs and are sensitive to the effects of many different types of health problems. These functional limitations are related statistically to objectively-measured work productivity.(35) This relationship is expressed in the scoring algorithm of the WLQ Productivity Loss Score. This empirically-based algorithm imputes at-work productivity loss from WLQ responses concerning impaired ability to perform work tasks. The minimum productivity loss score of 5% is consistent with an impaired ability to work approximately 20% of the time over two weeks.(36)
The study exclusions were: planning to retire within two years; receiving work disability benefits; active alcoholism or drug-abuse based on the five-item CAGE;(37) pregnant or six months postpartum; schizophrenia or bipolar disorder; non-English speaking and/or reading; and/or diagnosed with one or more of 12 medical conditions that have symptoms that potentially interfere with working (e.g., angina, congestive heart failure, stroke, diabetes, chronic obstructive lung disease).(38)
Eligible employees were provided with information about the study on the website and a toll-free study phone number was provided in case there were additional questions. Employees interested in enrolling could endorse the informed consent form and complete the baseline questionnaire on the website. Consenting employees then were allocated by electronic randomization to either the WHI treatment group or usual care group. Based on the previous study’s results, randomization was set at a 2:1 ratio for treatment vs. usual care providing the study with 70% power to detect effects on the primary work outcomes and 85% power to find effects for depression symptom severity.
Four months post-baseline, employees in both groups completed a follow-up survey on the study’s website (or in hard-copy, by request). Employees were offered a monetary incentive of $10 for completing each questionnaire. The Tufts Medical Center/Tufts University Institutional Review Board approved the study protocol.
Outcome Measures
The study’s primary outcomes were the pre-test (baseline) to four-month (post-test) changes in at-work performance as measured by the WLQ (25-item version). The WLQ is a validated self-report survey tool for assessing the impact of health problems, including depression, on at-work performance and productivity (“presenteeism”).(34, 35) The WLQ generates four at-work performance scale scores reflecting the percentage of time in the prior two weeks emotional and/or physical health problems limited ability to perform specific job tasks. The WLQ scales measure four dimensions of performance: time management and performance of physical tasks, mental-interpersonal tasks and output tasks (e.g., handling the workload and finishing work on time). Scores range from 0% (limited none of the time) to 100% (limited all of the time). A fifth outcome was the WLQ at-work Productivity Loss Score. The Productivity Loss score, the weighted sum of the four scale scores, indicates the percentage reduction in at-work productivity relative to a healthy benchmark group.
The WLQ Work Absence Module measured self-reported time missed from work in the past two weeks due to health or medical care. Absence-related productivity loss was the ratio of time missed in the past two weeks to time usually spent working.
A secondary outcome was the change in depression symptom severity as measured by the PHQ-9.(30, 31)This measure was used for subjects with depression and/or dysthymia.
Independent Variables
The major independent variable was treatment group (WHI treatment group = 1; usual care group = 0). Demographics included employee age in years, gender (male=1; female=0), race/ethnicity (White=1; Non-White=0), marital status (married =1; other =0) and years of education. Annual job earnings (in dollars) was measured using questions from the Panel Study of Income Dynamics, modified for self-administration.(39) Also included was the number of jobs held since age 18, type of position (four open-ended questions that we coded into the Bureau of the Census occupational categories)(40), years in current position, weekly work hours, and permanent or contract employment. Health measures included the presence or absence of various non-excluded chronic medical conditions, history of taking psychoactive medications including antidepressants, other current medications, hospital visits in the past year, and care received for emotional problems in the past four months.
WHI Intervention
The WHI is provided over the phone by EAP counselors trained in its methods. The program lasts for eight weeks with one-hour visits occurring every two weeks. The WHI aims to optimize functional outcomes using vocational, medical and psychological strategies (see Case Vignette.)
Work Coaching and Modification interventions target specific job performance difficulties related to depression, guiding the employee to change modifiable aspects of work methods and/or work conditions.
Care Coordination involves outreach by the counselor to the employee and his or her primary care physician (PCP) or other prescribing professional to promote adherence to already prescribed antidepressants and the use of evidence-based depression treatment (including clinical follow-up for inadequate antidepressant response). Counselors provide psycho-education about the impact of depression on work, medical treatment options including antidepressants and adherence and, with employee permission, send monthly updates to the medical provider of PHQ-9 and WLQ short-form results.
Cognitive-Behavioral Therapy (CBT) Strategies uses an adapted version of the workbook, Creating a Balance(41) to help employees change behaviors and cognitions that accompany depression and may interfere with functioning.
In the WHI, the counselor and employee co-create a care plan for dealing with each functional problem and review specific assignments and progress at each session. A motivational enhancement approach is utilized to promote and solidify change.
Throughout the study, the WHI counselors received training and ongoing supervision from the investigators. Care was documented on the study’s clinical website and monitored continually. For this RCT, treatment was provided by Maine State Government’s EAP provider, AllOne Health (formerly Health Resources of Natick, MA). Seven counselors volunteered to participate and the study compensated the EAP for their time. Employees assigned to either the treatment or usual care groups received electronic feedback and their depression and advised to seek care. All employees regardless of group were free to use other primary care, specialty care, behavioral health programs and/or standard EAP services. To minimize the threat of contamination the study subjects contacting the EAP for services were assigned to non-study counselors and study counselors were required to follow strict confidentiality procedures and not share study information.
Statistical Analysis
Prior to testing the study hypothesis, the quality of the study design was evaluated. To examine the recruitment procedure, screener results for eligible employees who enrolled in the study were compared to results for eligible employees who did not enroll. To assess the randomization, baseline data were compared for the WHI treatment group vs. the usual care group. Bias due to study attrition was evaluated by comparing subjects who dropped out prior to follow-up with those who completed it, and by doing a sensitivity analysis of results including subjects who dropped out using last observation carry-forward (LOCR). Differences were tested with t-tests, ANOVA or chi-square as appropriate.
Descriptive statistics including means and their standard deviations (SD), medians and the inter-quartile ranges (IQRs) and percentages were generated for each variable. These statistics were generated for each group separately and for the total sample. Cross-sectional group differences were tested.
In a series of regressions (one for each outcome) the differences between the WHI treatment group and usual care group were computed. First, the average pre-post difference was determined for each outcome within each group. Since a higher value on each variable signifies a worse outcome, a negative change score indicated an improvement from baseline. Second, the pre-test post-test changes for each subject were regressed on a treatment group indicator (WHI treatment group=1, usual care group=0). Regressions adjusted for employee age, gender, occupation (white collar=1; other =0) and the baseline score of the dependent variable. A result was considered statistically significant if it had a p-value ≤ .050 or a confidence interval excluding zero.
To summarize model results, the effect size for the baseline to four-month follow-up change in each outcome variable was computed. Effect size was defined as the average change within group divided by the pooled standard deviation. An effect size of 0.8 or more was considered large—large enough to be observable for each subject - whereas an effect size less than 0.2 was defined as small.
To quantify the marginal impact of the WHI in terms of the amount of productivity cost saved, the change in productivity cost in the treatment group was compared to the change in cost in the usual care group. To determine the change in productivity cost, the mean change in productivity loss (for at-work productivity and absences separately) was multiplied by $33,841.60. This figure is the 2010 median hourly wage for workers in the United States (US) annualized ($16.27 × 2080 full-time hours).(42) The US median wage is somewhat higher than this sample’s actual median annual income ($30,991) but provides a stable estimate of earnings.
We report both the unadjusted difference in productivity cost and the adjusted difference. Unadjusted cost differences are reported for each group separately. These are based on the unadjusted changes in productivity for each group shown in Table 3. The adjusted difference in productivity cost is used to compare the marginal savings in productivity costs due to the WHI over usual care. The adjusted productivity loss changes are shown in Table 3 (“Difference Between Change Scores”). Both the adjusted and unadjusted productivity loss change figures were multiplied by the annualized US median wage. The difference between the WHI and usual care groups was obtained for at-work productivity and absence costs respectively and the differences were summed to generate the total productivity cost savings.
Table 3.
Post-Intervention Comparison of the Work and Health Initiative (WHI) Treatment Group and Usual Care Group
| WHI Treatment | Usual Care (N=27) | Difference Between Change Scores | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (N=52) | Follow-up (N=47) | Change | Baseline (N=27) | Follow-up (N=25) | Change | |||||||||||||
| Mean | SD | Mean | SD | Mean | Effect Size | DF | Mean | SD | Mean | SD | Mean | Effect Size | DF | Δ | Effect Size | P-Value | DF | |
| WLQ Scores | ||||||||||||||||||
| Time Management | 45.6 | 20.8 | 27.5 | 19.0 | −18.1 | −0.87 | 1,49 | 43.7 | 17.6 | 42.7 | 16.5 | −0.9 | −0.05 | 1,26 | −15.4 | −0.73 | 0.005 | 1,62 |
| Physical Tasks | 23.3 | 21.2 | 12.4 | 15.4 | −10.9 | −0.51 | 1,49 | 18.3 | 22.1 | 16.2 | 17.6 | −2.0 | −0.09 | 1,26 | −11.7 | −0.54 | 0.027 | 1,64 |
| Mental-Interpersonal Tasks | 37.3 | 15.8 | 25.5 | 17.0 | −11.8 | −0.75 | 1,50 | 38.5 | 14.6 | 36.8 | 16.4 | −1.6 | −0.11 | 1,26 | −9.5 | −0.59 | 0.017 | 1,64 |
| Output Tasks | 40.7 | 23.2 | 26.5 | 23.5 | −14.2 | −0.61 | 1,51 | 39.1 | 22.8 | 40.1 | 22.1 | 1.0 | 0.04 | 1,26 | −13.9 | −0.70 | 0.006 | 1,64 |
| % At-Work Productivity Loss | 10.3 | 4.3 | 6.8 | 4.3 | −3.5 | −0.81 | 1,48 | 10.1 | 3.8 | 9.8 | 4.0 | −0.3 | −0.08 | 1,26 | −2.9 | −0.78 | 0.002 | 1,61 |
| Absences | ||||||||||||||||||
| Days Missed Per Two Weeks | 1.7 | 1.7 | 1.0 | 1.2 | −0.8 | −0.47 | 1,50 | 1.1 | 1.4 | 2.2 | 2.6 | 1.1 | 0.79 | 1,26 | −1.7 | −0.87 | 0.001 | 1,65 |
| % Productivity Loss due to Absence | 16.6 | 14.6 | 9.5 | 12.1 | −7.1 | −0.49 | 1,50 | 11.9 | 14.2 | 20.9 | 23.8 | 9.0 | 0.63 | 1,26 | −15.0 | −0.90 | 0.001 | 1,61 |
| PHQ-9 Symptom Severity | 13.1 | 5.1 | 7.7 | 5.8 | −5.4 | −1.06 | 1,51 | 12.2 | 5.6 | 12.8 | 6.4 | 0.6 | 0.11 | 1,26 | −6.8 | −1.09 | 0.001 | 1,66 |
DF = degrees of freedom
Statistically significant change scores and change differences at the P≤.05 level are indicated in bold
The effect sizes for the difference between the change scores were calculated by dividing the change difference by the pooled standard deviations of the change scores for both the Usual Care and the treatment group change.
The difference between change scores between groups were adjusted by baseline score, age, gender and types of occupation (white collar vs. blue collar)
RESULTS
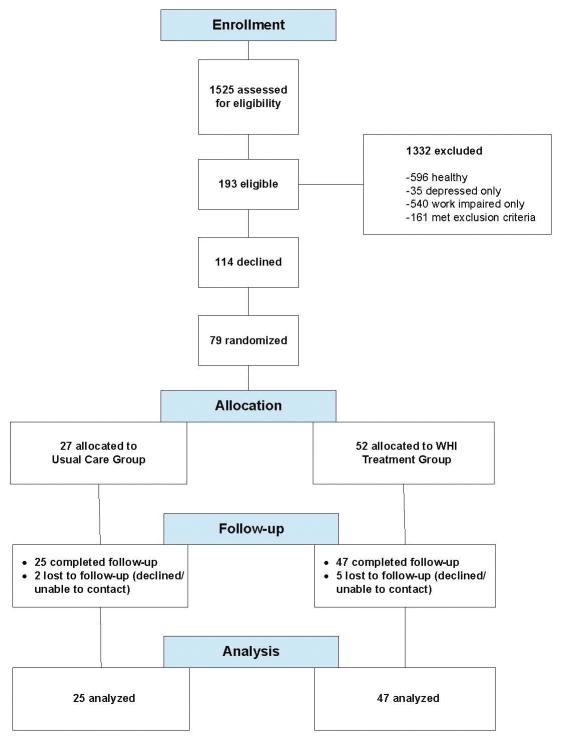
During the six-month recruitment period, the study website received 3,531 hits (33.9% hit rate for 10,400 employees). A total of 1,525 (43.2%) completed the screener, of which 1,332 (87.3%) were ineligible and 193 (12.6%) were eligible (Figure 1). Of the 1,332 ineligible employees, 596 (44.7%) neither had depression nor met the required productivity loss minimum score of 5%. Another 540 (40.5%) met the productivity loss criterion but did not have depression.
Figure 1.
Study Enrollment
Of the 193 eligible employees, 79 (40.9%) enrolled. There were no differences at screening between the eligible employees who enrolled and those that did not enroll (data not shown). One-third of the 79 eligible employees were randomly assigned to a usual care group (n=27) and two-thirds were assigned to the WHI treatment group (n=52). At baseline, there were no statistically significant group differences on clinical, demographic or occupational characteristics (Table 1).
Table 1.
Baseline Characteristics of the Work and Health Initiative (WHI) Treatment Group and Usual Care Group
| Characteristic | Total (N=79)
|
WHI Treatment (N=52)
|
Usual Care (N=27)
|
P-Value
|
DF
|
|||
|---|---|---|---|---|---|---|---|---|
| Age in Years | Mean | SD | Mean | SD | Mean | SD | ||
| 45.6 | 9.4 | 45.5 | 9.8 | 45.9 | 8.6 | |||
| Median | IQR± | Median | IQR± | Median | IQR± | |||
| Income ($/year) | 30,991 | 21,059 | 35,500 | 23,570 | 29,400 | 19,570 | 0.13 | (1,64) |
| N | % | N | % | N | % | |||
| Male | 17 | 21.5 | 12 | 23.1 | 5 | 18.5 | 0.65 | (1,77) |
| White | 76 | 98.7 | 50 | 100.0 | 26 | 96.3 | 0.18 | (1,75) |
| Married | 37 | 47.4 | 24 | 47.1 | 13 | 48.1 | 0.93 | (1,76) |
| Profess., Technical, Managerial Occup. | 51 | 64.6 | 33 | 63.5 | 18 | 66.7 | 0.78 | (1,77) |
| Sales, Support, Service Occup. | 32 | 40.5 | 23 | 44.2 | 9 | 33.3 | 0.36 | (1,77) |
| Repairs, Construction, Production, Transportation, Other Occup. | 1 | 1.3 | 1 | 1.9 | 0 | 0.0 | 0.48 | (1,77) |
| Major Depression | 20 | 25.6 | 15 | 28.8 | 5 | 19.2 | 0.37 | (1,76) |
| Dysthymia | 37 | 46.8 | 25 | 48.1 | 12 | 44.4 | 0.76 | (1,77) |
| Double Depression | 21 | 26.6 | 12 | 23.1 | 9 | 33.3 | 0.33 | (1,77) |
| On Antidepressant in Past Month | 45 | 57.0 | 29 | 55.8 | 16 | 59.3 | 0.77 | (1,77) |
| Currently on Antidepressant | 43 | 54.4 | 29 | 55.8 | 14 | 51.9 | 0.74 | (1,77) |
| Co-morbidity | 62 | 78.5 | 42 | 80.8 | 20 | 74.1 | 0.50 | (1,77) |
| Hospitalization for emotional problems | 5 | 6.4 | 5 | 9.8 | 0 | 0.0 | 0.10 | (1,76) |
| Visited PCP for emotional problems | 36 | 45.6 | 26 | 50.0 | 10 | 37.0 | 0.28 | (1,77) |
| Visited psychiatrist | 10 | 12.8 | 6 | 11.8 | 4 | 14.8 | 0.71 | (1,76) |
| Contacted EAP | 12 | 15.4 | 9 | 17.6 | 3 | 11.1 | 0.45 | (1,76) |
IQR = inter-quartile range
DF = degrees of freedom
Five (9.6%) employees in the WHI treatment group and 2 (7.4%) of the usual care group did not complete the follow-up questionnaire and were considered dropouts. Within the WHI treatment group, there were no significant baseline differences between employees completing the study and drop-outs on the demographic variables, co-morbid conditions, PHQ-9 scores and WLQ scores (data not shown).
At baseline (Table 1), the sample had a mean age was 45.6 years (SD=9.4). Males comprised 21.5% (n=17) and 78.5% was female (n=62). Most were White (98.7%, n=76). The majority (64.6%, n=51) had professional, technical or managerial occupations, 40.5% (n=32) were in sales, service and support positions and 1.3% (n=1) were in occupations such as repairs, production, construction, and transportation. The median annual earnings was $30,000 (IQR=25,185).
With regard to current depression at baseline and depression history (Table 1), 25.6% (n=20) met criteria for MDD, 46.8% (n=37) met screening criteria for dysthymia, and 26.6% (n=21) met criteria for both (known as double depression; DD); (Table 1). The average PHQ-9 depression symptom severity was moderate at 12.8 (SD=5.2); (Table 2). More than half (57.0%; n=45) had a history of antidepressant medication use and 54.4% (n=43) were being prescribed an antidepressant at baseline. More than three-fourths (78.5%; n=62) had a co-morbid condition. Almost half (45.6%; n=36) visited a primary care physician for an emotional problem in the three months prior to baseline.
Table 2.
Baseline Characteristics of the Work and Health Initiative (WHI) Treatment Group and Usual Care Group Work Limitations Questionnaire and PHQ-9 Scores
| Characteristic | Total (N=79)
|
WHI Treatment (N=52)
|
Usual Care (N=27)
|
P-Value | DF | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||
| Depression by PHQ-9 (SD) | 12.8 | 5.2 | 13.1 | 5.1 | 12.2 | 5.6 | 0.45 | (1,77) |
| WLQ Scores | ||||||||
| Time Management | 44.9 | 19.7 | 45.6 | 20.8 | 43.7 | 17.6 | 0.69 | (1,74) |
| Mental-Interpersonal Tasks | 37.7 | 15.3 | 37.3 | 15.8 | 38.5 | 14.6 | 0.75 | (1,76) |
| Physical Tasks | 21.5 | 21.5 | 23.2 | 21.2 | 18.3 | 22.1 | 0.34 | (1,75) |
| Output Tasks | 40.1 | 22.9 | 40.7 | 23.2 | 39.1 | 22.8 | 0.77 | (1,77) |
| Percentage At-Work Productivity Loss | 10.2 | 4.1 | 10.3 | 4.3 | 10.1 | 3.8 | 0.86 | (1,73) |
| Absences | ||||||||
| Days Missed Per Two Weeks | 1.5 | 1.6 | 1.7 | 1.7 | 1.1 | 1.4 | 0.12 | (1,76) |
| Percentage Productivity Loss due to Absence | 15.0 | 14.6 | 16.6 | 14.6 | 11.9 | 14.2 | 0.18 | (1,74) |
Mean percentage of time in the prior two weeks health problems limited ability to perform tasks listed in scale
DF = degrees of freedom
Both the WHI treatment and usual care groups had similar levels of baseline at-work performance and work absences (p > .05) on four WLQ scales scores, the productivity loss score, work absences and productivity loss due to absences (Table 2). In the total sample, ability to perform tasks related to time management was impaired an average of 44.9% (SD=19.7%) of the time in the prior two-week period. Ability to perform mental and interpersonal job tasks was impaired an average of 37.7% (SD=15.3%) of the time in the past two weeks. Ability to perform physical job tasks was impaired an average of 21.5% (SD=21.5%) of the time in the past two weeks. Ability to perform tasks related to managing output was impaired 40.1% (SD=22.9%) of the time on average. At-work productivity was reduced by an average of 10.2% (SD=4.1%) in the two-week period prior to baseline. On average, employees missed 1.5 (SD=1.6) workdays due to health problems in the two weeks prior to baseline for an average productivity loss of 15.0% (SD= 14.6); (Table 2).
By follow-up (Table 3), all eight outcomes improved significantly (p<.01) in the WHI treatment group. Outcomes in the usual care group were either worse compared to baseline or not significantly improved. Also, the magnitude of the change (improvement) in all eight outcomes was significantly larger in the WHI treatment group than in the usual care group (p<.01). All of the improvements in the WHI treatment group represented moderate to large effects (Table 3).
Within the WHI treatment group, at-work performance improved an average of 18.1 points for time management, 10.9 points for physical job tasks, 11.8 points for mental-interpersonal job tasks and 14.2 points for output tasks. These represent between 20% and 50% of the initial WLQ scale average. At-work productivity loss for the WHI treatment group declined from 10.3% (SD=4.3) to 6.8% (SD=4.3), for an average improvement of 3.5 percentage points (p < .01).
Absence days in the WHI treatment group improved from 1.7 (SD=1.7) to 1.0 days (SD=1.2); (p < .01). Productivity loss due to absences improved 7.1% (p < .01).
In the usual care group, the mean change in at-work performance measured by the WLQ scales ranged from an improvement of 2% for the WLQ physical tasks scale to a deterioration of 1% for the WLQ output tasks scale. Mean at-work productivity loss improved by 0.3%. Absence days increased on average by 1.1 days.
At follow-up, PHQ-9 depression severity scores also significantly improved in the WHI treatment group (Table 3). Mean scores improved from 13.1 (SD=5.1) to 7.7 (SD=5.8); (p<.001). The change in usual care group mean scores was not significant (p ≥.05). The magnitude of the change was significantly higher in the WHI treatment group, indicating more symptom reduction (p < .001).
Sensitivity analyses including the seven employees that were lost to follow-up (last observation carried forward) confirmed the results.
The unadjusted mean at-work productivity cost savings in the WHI group was $1182.70 annually per participant vs. $96.10 annually per participant in usual care. For absences, the unadjusted mean savings was $2395.90 annually per participant in WHI treatment vs. a $3043.30 annual per participant cost increase for usual care. The total unadjusted annualized mean productivity cost savings from WHI treatment was $3578.60 per participant vs. a cost increase of $2947.20 per participant in usual care.
Comparing the WHI and usual care groups, the adjusted mean total productivity cost savings from the WHI was $6041.70 per participant. This reflects an adjusted estimated per participant savings in at-work productivity for the WHI of $979.70 and an adjusted estimated savings per participant in absence costs of $5062.00
DISCUSSION
The WHI program had moderate to large positive effects on multiple indicators of functioning including at-work performance, at-work productivity loss, work absences and productivity loss due to missed work time. Additionally, the WHI had a large effect on depression symptom severity. While the small sample sizes contributed to confidence intervals spanning a range of effect sizes, the results support the WHI’s impact. The WHI was superior to usual care in helping employees with depression function more effectively and productively.
In the WHI group, at-work productivity loss declined 34% on average compared to 3% in the usual care group. Productivity loss related to absenteeism improved an average of 43% for the WHI group and worsened an average of 100% for the usual care group. Depression severity improved by an average of 41% in the WHI group and worsened by 5% on average in the usual care group.
The WHI program did not have any discernable adverse impact on employees. For example, there were no reports of job loss related to participating in the program. Part of this success may be attributed to the extensive efforts made to protect employee privacy. Privacy protection was addressed at all levels of study operations, including the design and execution of the information system and in the training and supervision of the WHI counselors. In addition, the screening campaign did not target only those employees who thought they might be depressed. All employees were invited to take the health assessment. In addition, the WHI did not seem to have any negative effects on the employee-physician relationship. In both the WHI and usual care groups, there were no significant changes in the number of visits in the prior four months either to primary care physicians, psychiatrists or other mental health providers.
The annualized total productivity cost savings in the WHI group of $6041.70 per participant is an indicator of the program’s potential value. This result mainly reflects the cost of increased work absence in the usual care group. While this estimate did not include additional employer costs such as employee fringe benefits and overhead, the savings could be overstated if the treatment effect was not sustained. Future studies will benefit from longer periods of observation and additional data necessary to perform a more comprehensive cost-benefit analysis.
These results are promising but several caveats apply. First, utilization of usual care was left up to the employee, which may have diluted its impact. Additionally, the sample was too small to determine whether all of the WHI interventions were equally useful and provided at appropriate levels of intensity and duration. Another design limitation was the brief follow-up period. It is impossible to know whether the observed effects of the WHI would have lasted longer. Additionally, while appropriate to this stage of research, the use of a single public-sector employer (with a predominantly rural White employee population), and the use of a single EAP, both limit external validity. Finally, while the work outcome measures have been validated in both healthy and depressed samples,(35, 43) the study may have benefited from work performance and productivity data from other sources.
Study strengths included the detailed conceptual model for the WHI program, the study’s randomized design, tracking and comparison of bias, use of validated measurement tools that are administered extensively in work settings and careful monitoring and documentation of the treatment protocols.
Guideline-concordant treatment of depression is necessary for symptom remission and the WHI may provide another tool for ensuring that working-age people with depression are able to participate fully and effectively in the labor market. However, more research is needed. It will be valuable to test the costs and benefits of the WHI relative to other interventions. However, finding appropriate comparators is not straightforward. Conceivably it could be compared to evidence-based treatment such as collaborative care, psychiatric care, and/or usual EAP care. Additionally, while the program uses an available resource, the EAP, and could be adapted for behavioral health programs, additional studies focusing on WHI dissemination, implementation and engagement are necessary.
This study suggests that the WHI, which shifts care from a strictly biomedical to a functional paradigm, may be a step in the right direction. It addresses a significant personal, public health and economic problem and is aligned with the growing trend to help employees improve their health and wellness.(44)
WHI CASE VIGNETTE
Mr. A is a mid-level administrator in a wholesale products company whose baseline survey responses were consistent with major depression and dysthymia and multiple deficits in ability to function at work. At his first of eight telephonic sessions with his study counselor, Ms. B, she described the Work and Health Initiative (WHI) program, highlighting its emphasis on improving functional effectiveness at work by addressing features of the work environment, medical care and coping issues. The WHI program’s three components are discussed below.
Work Coaching/Modification
Ms. B engaged Mr. A in a discussion of the specific difficulties he was having performing his job, basing this discussion on his responses to the Work Limitations Questionnaire (WLQ). Mr. A was struggling most with concentration, which was interfering with the most important part of his job—making a high volume of customer phone calls. Ms. B elicited additional information from Mr. A so she could understand specifically the nature of his job’s demands for customer contact and service and how his poor concentration interfered with his ability to meet those demands. She also elicited information about the social and physical organization of his work to identify potentially relevant environmental barriers and resources. Mr. A reported that he makes customer calls in a cubicle, where he has little privacy from the larger office area. Additionally, during certain work hours there is a lot of activity in the area, which makes it noisy and visually distracting. She also determined that Mr. A’s call output was closely monitored but he had flexibility to structure his time and approach to customer service. To determine whether there were better or worse times of the day to make calls, Mr. A. was asked to keep a diary of the time of day and work conditions when he had the most and least difficulty making calls. Next, Mr. A and Ms. B collaboratively developed behavioral experiments to help Mr. A take advantage of the quieter, less distracting times and avoid the noisier more distracting ones. Ms. B. coached Mr. A on becoming more effective in using his time. She helped Mr. A conceptualize his work in three phases: preparation; the call; and call follow-up. With her help, Mr. A created a schedule and task list to follow for each phase. Mr. A practiced and monitored this new approach for several sessions and worked with Ms. B to fine-tune the changes to optimize his ability to perform this task. Mr. A experienced increased ability to focus on this important work task and felt that these modifications helped him initiate and complete more calls and to feel more effective.
Care Coordination
Ms. B helped Mr. A understand that some of his work difficulties, especially fatigue and poor concentration, were related to his depression and could potentially respond to medical treatment. Mr. A disclosed an internal barrier preventing him from accessing medical treatment—that he was ashamed to be taking an antidepressant. Ms. B addressed this barrier openly and helped Mr. A understand depression in a medical framework. Ms. B also coached Mr. A through his reluctance to tell his primary care physician (PCP) that he had stopped taking a previously prescribed antidepressant due to side effects. Consistent with the WHI protocol, Ms. B obtained permission from Mr. A to send his PCP the results of baseline assessments of depression symptom severity and work impairments, highlighting his difficulty concentrating. She also reported on Mr. A’s medication adherence problem and concern about side effects. Ms. B continued to coach Mr. A about how to effectively communicate his concerns to his PCP. Mr. A made a follow-up appointment with his PCP, communicated his concerns about side effects and was started on a new antidepressant. Ms. B continued to update Mr. A’s PCP about his progress. After medication adjustments, Mr. A. reported a 50% improvement in depression symptoms, better adherence and fewer side effects. He committed to a minimum additional six-month medication trial and to discuss concerns directly with his PCP.
Cognitive Behavioral Therapy (CBT) Strategies
Ms. B introduced Mr. A to the program’s coping skills workbook, which is designed to address maladaptive behavioral and cognitive patterns that often accompany depression and interfere with performing activities of daily living including working. Ms. B explained the rationale for this approach, which involved adopting an “experimental attitude” to try out different ways of behaving and thinking in everyday life and noting the impact of these changes on depression symptoms and functioning. In each session, Ms. B guided Mr. A through cognitive and behavioral therapy concepts and he completed homework assignments between his sessions. Through this process, Mr. A identified specific barriers to effectively coping with life and work, including behavioral patterns of avoiding social situations and activities he had previously enjoyed and cognitive patterns of negative, overly critical self-talk that increased when he felt under pressure at work. The workbook concepts helped Mr. A to understand that these behavioral and cognitive patterns were roadblocks to feeling better and effectively performing his job. Behavioral strategies, customized to address Mr. A’s specific difficulties, included increasing positive activities, taking a 30-minute walk before work and noticing its impact on concentration and work performance and engaging in muscle relaxation before making customer phone calls. In the latter stage of the intervention, Mr. A refined his use of coping strategies to manage negative thoughts. He learned to identify specific patterns of negative self-talk (“I can’t do anything right”, “I’m so stupid”, “I’ll never get through all these phone calls.”) and used thought stopping techniques to decrease them. With decreased negative self-talk, Mr. A noticed that he was better able to focus on the task at hand and did not experience a decrease in energy and mood when faced with work challenges.
By the end of the intervention, Mr. A demonstrated significant improvement in depression symptoms and functioning at work and felt much more effective in managing his symptoms and work performance.
Acknowledgments
Source of Funding: This study was sponsored by the National Institute of Mental Health 1 R34 MH072735-01A1.
Footnotes
Conflicts of Interest: There are no competing interests for any of the authors.
Reference List
- 1.Lerner DJ, Henke RM. What does research tell us about depression, job performance and work productivity? JOEM. 2008;50(4):401–410. doi: 10.1097/JOM.0b013e31816bae50. [DOI] [PubMed] [Google Scholar]
- 2.Woo JM, Kim W, Hwang TY, Frick KD, Choi BH, Seo YJ, Kang EH, Kim SJ, Ham BJ, Lee JS. Impact of Depression on Work Productivity and Its Improvement after Outpatient Treatment with Antidepressants. Value in Health. 2011;14(1):475–482. doi: 10.1016/j.jval.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Barber C, Birnbaum HG, Frank RG, Greenberg PE, Rose RM, Simon GE, Wang P. Depression in the workplace: effects on short-term disability. Health Aff(Millwood) 1999;18(5):163–171. doi: 10.1377/hlthaff.18.5.163. [DOI] [PubMed] [Google Scholar]
- 4.Conti DJ, Burton WN. The cost of depression in the workplace. Behav Health Tomorrow. 1995;4(4):25–27. [PubMed] [Google Scholar]
- 5.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA. 2003 Jun 18;289(23):3135–3144. doi: 10.1001/jama.289.23.3135. [DOI] [PubMed] [Google Scholar]
- 6.Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, Corey-Lisle PK. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry. 2003;64(12):1465–1475. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- 7.Pignone MP, Gaynes BN, Rushton JL, Burchell CM, Orleans CT, Mulrow CD, Lohr K. Screening for Depression in Adults: A Summary of the Evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2002;136(10):765–776. doi: 10.7326/0003-4819-136-10-200205210-00013. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Akiskal HS, Ames M, Birnbaum H, Greenberg P, RMA, Jin R, Merikangas KR, Simon GE, Wang PS. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. Am J Psychiatry. 2006;163(9):1561–1568. doi: 10.1176/appi.ajp.163.9.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Birnbaum HG, Kessler RC, Kelley D, Ben-Hamadi R, Joish VN, Greenberg PE. Employer burden of mild, moderate, and severe major depressive disorder: mental health services utilization and costs, and work performance. Depress Anxiety. 2010;27(1):78–89. doi: 10.1002/da.20580. [DOI] [PubMed] [Google Scholar]
- 10.Rost K, Smith JL, Dickinson M. The effect of improving primary care depression management on employee absenteeism and productivity. A randomized trial. Med Care. 2004;42(12):1202–1210. doi: 10.1097/00005650-200412000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rost K, Fortney J, Coyne J. The relationship of depression treatment quality indicators to employee absenteeism. Ment Health Serv Res. 2005;7(3):161–169. doi: 10.1007/s11020-005-5784-3. [DOI] [PubMed] [Google Scholar]
- 12.Schoenbaum M, Unutzer J, McCaffrey D, Duan N, Sherbourne C, Wells KB. The effects of primary care depression treatment on patients’ clinical status and employment. Health Serv Res. 2002;37(5):1145–1158. doi: 10.1111/1475-6773.01086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang PS, Simon GE, Avorn J, Azocar F, Ludman EJ, McCulloch J, Petukhova MZ, Kessler RC. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA. 2007;298(12):1401–1411. doi: 10.1001/jama.298.12.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lerner D, Adler DA, Hermann RC, et al. Depression and Work Performance: The Work and Health Initiative Study. In: Schultz IZ, Rogers E, editors. Work Accomodation and Retention in Mental Health. New York: Springer; 2011. pp. 103–120. [Google Scholar]
- 15.Bee PE, Bower P, Gilbody S, Lovell K. Improving health and productivity of depressed workers: a pilot randomized controlled trial of telephone cognitive behavioral therapy delivery in workplace settings. Gen Hosp Psychiatry. 2010;32(3):337–340. doi: 10.1016/j.genhosppsych.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 16.Costa-Black KM, Loisel P, Anema JR, Pransky G. Back pain and work. Best Pract Res Clin Rheumatol. 2010;24(2):227–240. doi: 10.1016/j.berh.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 17.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002 Oct 9;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 18.Wagner EH. The role of patient care teams in chronic disease management. BMJ. 2000 Feb 26;3207234:569–572. doi: 10.1136/bmj.320.7234.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006 Nov 27;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 20.Unutzer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Arean PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002 Dec 11;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 21.Katon WJ. The Institute of Medicine “Chasm” report: implications for depression collaborative care models. Gen Hosp Psychiatry. 2003;25(4):222–229. doi: 10.1016/s0163-8343(03)00064-1. [DOI] [PubMed] [Google Scholar]
- 22.Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA. 2003;289(23):3145–3151. doi: 10.1001/jama.289.23.3145. [DOI] [PubMed] [Google Scholar]
- 23.Katon W, Unutzer J, Wells K, Jones L. Collaborative depression care: history, evolution and ways to enhance dissemination and sustainability. Gen Hosp Psychiatry. 2010;32(5):456–464. doi: 10.1016/j.genhosppsych.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shaw W, Hong Q, Pransky G, Loisel P. A literature review describing the role of return-to-work coordinators in trial programs and interventions designed to prevent workplace disability. J Occup Rehabil. 2008;18(1):2–15. doi: 10.1007/s10926-007-9115-y. [DOI] [PubMed] [Google Scholar]
- 25.Brewin CR. Theoretical foundations of cognitive-behavior therapy for anxiety and depression. Annu Rev Psychol. 1996;47(1):33–57. doi: 10.1146/annurev.psych.47.1.33. [DOI] [PubMed] [Google Scholar]
- 26.Simon GE, Ludman EJ, Rutter CM. Incremental benefit and cost of telephone care management and telephone psychotherapy for depression in primary care. Arch Gen Psychiatry. 2009;66(10):1081–1089. doi: 10.1001/archgenpsychiatry.2009.123. [DOI] [PubMed] [Google Scholar]
- 27.Handler Jeffrey, Doel Kelley, Henry Alexis, Lucca Anna. Rehab Rounds: Implementing Supported Employment Services in a Real-World Setting. Psychiatr Serv. 2003 Jul 1;54(7):960–962. doi: 10.1176/appi.ps.54.7.960. [DOI] [PubMed] [Google Scholar]
- 28.Lehman AF, Goldberg R, Dixon LB, McNary S, Postrado L, Hackman A, McDonnell K. Improving employment outcomes for persons with severe mental illnesses. Arch Gen Psychiatry. 2002;59(2):165–172. doi: 10.1001/archpsyc.59.2.165. [DOI] [PubMed] [Google Scholar]
- 29.Rubio DMG, Schoenbaum EE, Lee LS, Schteingart DE, Marantz PR, Anderson KE, Platt LD, Baez A, Esposito K. Defining translational research: Implications for training. Acad Med. 2010;85(3):470–475. doi: 10.1097/ACM.0b013e3181ccd618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999 Nov 10;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 32.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22(11):1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rogers WH, Wilson IB, Bungay KM, Cynn DJ, Adler DA. Assessing the performance of a new depression screener for primary care (PC-SAD) J Clin Epidemiol. 2002;55(2):164–175. doi: 10.1016/s0895-4356(01)00430-9. [DOI] [PubMed] [Google Scholar]
- 34.Lerner D, Amick BC, III, Rogers WH, Malspeis S, Bungay K, Cynn D. The Work Limitations Questionnaire. Med Care. 2001;39(1):72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Lerner D, Amick BC, III, Lee JC, Rooney T, Rogers WH, Chang H, Berndt ER. Relationship of employee-reported work limitations to work productivity. Med Care. 2003;41(5):649–659. doi: 10.1097/01.MLR.0000062551.76504.A9. [DOI] [PubMed] [Google Scholar]
- 36.Lerner D, Adler DA, Rogers WH, Chang H, Lapitsky L, McLaughlin T, Reed J. Work Performance of Employees with Depression: The Impact of Work Stressors. Am J Health Promot. 2010;24(3):205–213. doi: 10.4278/ajhp.090313-QUAN-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD. Screening for alcohol abuse using the CAGE questionnaire. Am J Med. 1987;82(2):231–235. doi: 10.1016/0002-9343(87)90061-1. [DOI] [PubMed] [Google Scholar]
- 38.Tarlov Alvin R, Ware John E, Jr, Greenfield Sheldon, Nelson Eugene C, Perrin Edward, Zuboff Michael The Medical Outcome Study. An Application of Methods of Monitoring the Results of Medical Care. JAMA. 1989;262(7):925–930. doi: 10.1001/jama.262.7.925. [DOI] [PubMed] [Google Scholar]
- 39.University of Michigan. Panel Study of Income Dynamics. [Accessed 2011.];Wave 37 Questionnaire. Available at: ftp://ftp.isr.umich.edu/pub/src/psid/questionnaires/q2011.pdf.
- 40.U.S. Department of Labor. Standard Occupational Classification System (SOC), US Bureau of Labor Statistics. Washington, D.C: 2000. [Google Scholar]
- 41.Simon G, Ludman E, Tutty S. Creating A Balance: A Step by Step Approach to Managing Stress and Lifting Your Mood. Victoria, B.C: Trafford Publishing (copyright, Group Health Cooperative); 2006. [Google Scholar]
- 42.United States Department of Labor. Bureau of Labor Statistics. [Accessed 2011.];National Occupational Employment and Wage Estimates. 2010 May; Available at: http://www.bls.gov/oes/current/oes_nat.htm#00-0000.
- 43.Sanderson K, Tilse E, Nicholson J, Oldenburg B, Graves N. Which presenteeism measures are more sensitive to depression and anxiety? J Affect Disord. 2007;101(1–3):65–74. doi: 10.1016/j.jad.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 44.Linnan L, Bowling M, Childress J, Lindsay G, Blakey C, Pronk S, Wieker S, Royall P. Results of the 2004 national worksite health promotion survey. Am J Public Health. 2008;98(8):1503–1509. doi: 10.2105/AJPH.2006.100313. [DOI] [PMC free article] [PubMed] [Google Scholar]