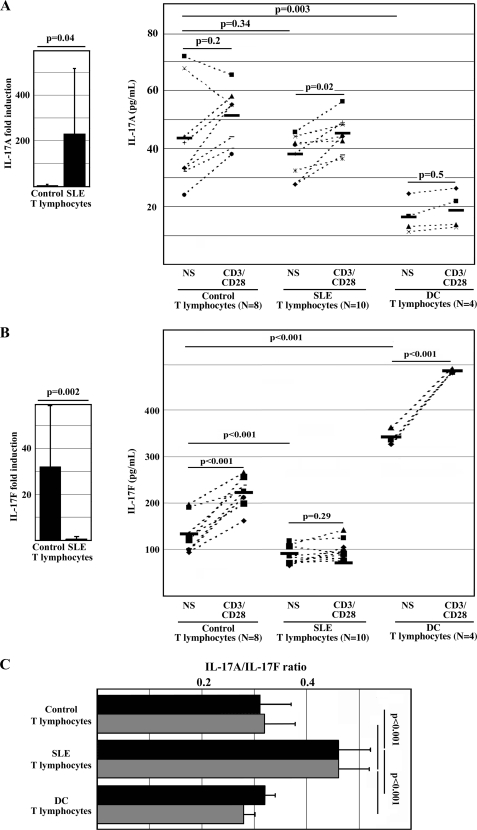
FIGURE 1.
Activated T lymphocytes from SLE patients fail to produce IL-17F. Primary T lymphocytes from healthy control individuals, SLE patients, and control individuals with other autoimmune diseases (DC; rheumatoid arthritis and psoriatic arthritis) were cultured in the presence or absence (not significant; NS) of anti-CD3 and anti-CD28 antibodies. After 72 h, cells were harvested and subjected to qRT-PCR; supernatants were subjected to IL-17A and IL-17F ELISA. A, T lymphocytes from SLE patients express significantly more IL-17A mRNA in response to stimulation with anti-CD3/CD28 antibodies when compared with T lymphocytes from healthy controls (left). T lymphocytes from healthy controls and SLE patients produce comparable amounts of IL-17A protein in response to T cell activation (72 h), whereas resting and activated T lymphocytes from DC patients produce lower amounts of IL-17A (right). B, T lymphocytes from SLE patients express significantly lower amounts of IL-17F mRNA in response to stimulation with anti-CD3/CD28 antibodies when compared with T lymphocytes from healthy controls (left). T lymphocytes from healthy controls and DC patients produce significantly more IL-17F in response to T cell activation, whereas resting and activated T lymphocytes from SLE patients fail to produce IL-17F (right). C, failure to express IL-17F protein results in an increased IL-17A/IL-17F (protein) ratio of SLE T lymphocytes when compared with healthy control and autoimmune disease control T cells. Black bars, IL-17A/IL-17F ratio in unstimulated cells; gray bars, cells after stimulation with anti-CD3/CD28 antibodies for 72 h. Error bars, S.D.