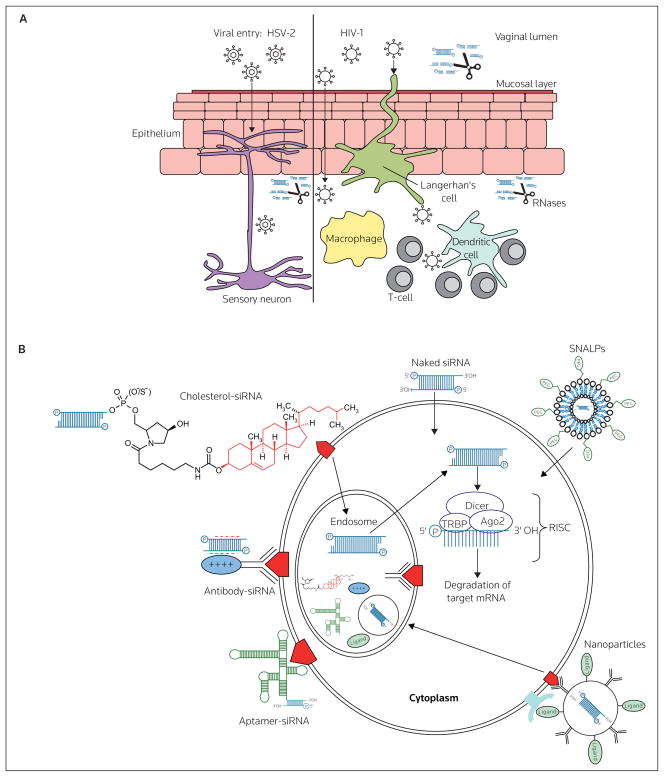
Figure 2. Routes of viral entry across vaginal mucosal epithelium and barriers to effective siRNA delivery following intravaginal administration.
(A) Local innate immune factors, including the acidic pH of the vaginal lumen and the presence of secreted proteins and a mucous layer contribute to preventing viral transmission. HSV-2 primarily infects epithelial cells and sensory neurons, whereas the initial targets of HIV-1 are dendritic cells, macrophages and CD4+ T-cells. To be effective, siRNA-based microbicides must be stable under acidic conditions, must be resistant to protease and RNase acitivity and must be able to gain access to the appropriate cell types to prevent viral transmission. (B) Having gained access to the appropriate cells in the vaginal mucosa, the route of cellular uptake by siRNA will likely determine the efficacy of gene knockdown. siRNAs must gain access to the RNA-induced silencing complex (RISC), which is located in the cytoplasm, but siRNAs may enter cells via endosomal uptake (eg, as antibody-, aptamer- and cholesterol-siRNAs and antibody-coated nanoparticles). Alternatively, naked siRNAs (either lipid-complexed or non-complexed) and liposomal particles (eg, stable nucleic acid-lipid particles [SNALPs]), may enter the cytoplasm directly following membrane fusion, or through, as yet undetermined, channels or receptors. Ago2 Argonaute 2, TRBP TAR RNA binding protein