Abstract
Purpose
The optimal management of pyogenic discitis is not agreed on. We conducted a retrospective, cross-sectional, observational study in which all patients with discitis who attended Hospital San Carlos Madrid from January 1999 to January 2009 were included.
Methods
We identified 108 consecutive adult patients with infectious discitis. There were 49 men and 59 women with an average age of 67,5 (+/- 16,89) years in the study group. Mean follow-up interval was 6,06 (12,5-2) years. 78 patients had spontaneous discitis and 30 patients had postoperative discitis. Inclusion criteria for the review were illness compatible with vertebral infection and / or evidence of spinal involvement on magnetic resonance imaging (MRI).
Results
In 56 percutaneous discal biopsy (52% patients) were positive in 28 cases. A single disc was infected in 100 patients. The segments involved were the cervical spine in four, the thoracic spine in 38 and the lumbar spine in 66. One or more comorbid diseases were present in 73 (68%) of 108 patients. Diabetes mellitus was the most common disease. Comorbid disease was rapidly fatal in four patients, ultimately fatal in seven patients, and nonfatal or not present in 97 patients (90 %).
Conclusion
Early diagnosis is a major challenge. Heightened awareness and the prompt use of MRI are necessary to avoid diagnostic delay. Prolonged antimicrobial therapy and the judicious application of timely surgical intervention are essential for an optimal outcome.
Introduction and epidemiology
The optimal management of pyogenic discitis is not agreed on. Little is known about the risk factors, clinical features, diagnosis, optimal treatment, or management outcomes of adults with spontaneous discitis. Few authors have evaluated prognostic factors, and relapse has received scant attention [1–6]. Our study was undertaken to review the clinical features of discitis in a large number of patients. We sought to identify the factors associated with poor outcome and relapse. We report a retrospective study of 108 patients with vertebral discitis who had adequate follow-up.
Clinical material and methods
We conducted a retrospective, cross-sectional, observational study in which all patients with discitis who attended our Centre from January 1999 to January 2009 were included. Records were obtained from the files of the Departments of Infectious Diseases and from files coded in the medical records in our Centre with a discharge diagnosis of vertebral discitis infection. Medical records and imaging studies were reviewed to obtain clinical data. Patients were considered to have a disc space infection on the basis of positive cultures, characteristic findings on pathology examination, or if the clinical and radiographic presentations were characteristic of the disease.
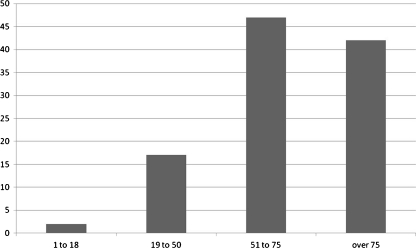
We identified 108 consecutive adult patients (older than 16) with infectious discitis There were 49 men and 59 women with an average age of 67.5 (±16.89) years in the study group (Fig. 1). Mean follow-up interval was 6.06 years (range, 2–12.5). Inclusion criteria for the review were illness compatible with vertebral infection and evidence of spinal involvement on MRIs. The MR findings to define the infection were bone marrow oedema, reduction in disc height, spinal cord changes and/or paravertebral collections. Eleven patients with tuberculosis were seen during the study period and were included. The severity of underlying non-infectious disease(s) was classified according to the following categories of McCabe and Jackson [1, 2]: rapidly fatal disease, ultimately fatal disease, nonfatal disease, or no underlying disease. Patients with compatible clinical presentation and radiographic findings in the absence of a history of surgery on the spine or adjacent regions were considered to have spontaneous discitis, while those with a history of spine surgery within five years of diagnosis were considered to have postoperative discitis [3]. By these criteria, 78 patients had spontaneous discitis and 30 patients had postoperative discitis.
Fig. 1.
Population per age included in the study
Statistical methods
Categorical factors, according to outcome (i.e., adverse outcome or recovery), were compared by use of the χ² test or Fisher’s exact test.
Results
Sites of involvement
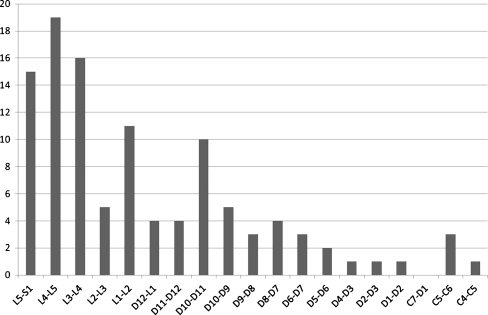
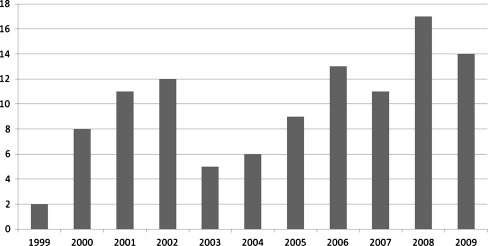
A single disk was infected in 100 patients. Two disks were infected in six patients and three in two patients. The segment involved was the cervical spine in four, the thoracic spine in 38, and the lumbar spine in 66. The discitis was after disc surgery in 30 (27.78%) patients. The location of lesions is shown in Fig. 2. The number of cases per year is shown in Fig. 3.
Fig. 2.
Vertebral levels affected in 108 patients included. Only one level was affected in 100 patients. Two levels were affected in six patients and three in two patients
Fig. 3.
Incidence of patients diagnosed as spondylodiscitis after meeting our inclusion criteria during the study period (1999–2009)
Comorbidity
One or more comorbid diseases were present in 56 (52%) of 108 patients. Seventeen patients presented two comorbidities and one patient had three of the comorbidities listed below. Diabetes mellitus was the most common disease which occurred in 18 patients (16.6%); also, there were ten cases of end-stage renal disease (9.25%), two injection drug abusers, five immunodeficiency cases, three cases of vascular access sites (Porth-A-Cat), and valvular cardiac prosthesis in five cases.
Clinical
Moderate to severe back pain was the initial manifestation in 97 cases (89.8%); 21 (19.4%) patients had a nerve root compression as the main clinical symptom; six patients had compressive myelopathy at the time of diagnosis. Eight patients presented with fever higher than 38°C.
Aetiology
Thirty patients were identified as developing the infection after spine surgery. This group of patients had undergone simple discectomy in the five years prior to the diagnosis. A total of 78 patients were classified as spontaneous discitis. The most common site of primary infection was the urinary tract, which affected 24 patients (30.8%); infection at a vascular access site was identified in six patients (7.7%); immunodeficiency was thought to be responsible for five infections (6.4%); intestinal infection was responsible for four discitis (5.1%); bacteraemia due to endocarditic disease affected four patients (5.1%); and sepsis after prostatic biopsy was responsible for two cases (2.6%). In 33 patients (42%) the primary infection was not identified, and because these patients had not undergone spine procedures they were classified as spontaneous disease.
Microbiology findings
Fifty-six (52% patients) percutaneous discal biopsies were perform to identify the micro-organism. Of these biopsies, 28 were positive (50%). Blood cultures were taken in 11 patients and were positive in only six cases. Other microorganisms were assumed to be the aetiology of the vertebral discitis because of concomitant infection and were identified by other methods, as urinary culture.
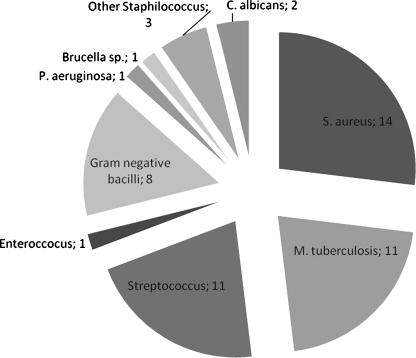
None of the patients with a negative biopsy had positive blood cultures. The total number of identified organisms were as follows: Staphylococcus aureus (n = 14; 28.6% of the positive cultures); Mycobacterium tuberculosis (n = 11; 22.4%); Streptococcus sp (n = 11; 12.2%); Enterococcus sp (n = 1); Gram-negative bacillus (n = 8); Pseudomonas aeruginosa (n = 1); Brucella (n = 1), Candida albicans (n = 2); other Staphylococcus (n = 3) (Fig. 4).
Fig. 4.
Distribution of the microbiological findings after percutaneous disc biopsies or blood cultures
Treatments used
Antibiotic therapy was given intravenously in all cases. The duration of intravenous therapy was 5.22 (±1.43) weeks. A combination of two antibiotics was initially used in 72 (66.67%) patients. The most common antibiotics used were vancomicyn (n = 24 cases; 22.23%); quinolone (n = 24; 22.2%), rifampicin (n = 14; 13%); linezolid (n = 8); gentamycin (n = 6); cephalosporin (n = 6); carbapenem (n = 5); cloxacillin (n = 4); other (n = 14); and tuberculostatic combination therapy (n = 14; 13%).
Operative management
Surgical treatment was performed for 27 (25%) of 108 patients. The most frequent indications were drainage of abscesses, relief of compression of the spinal cord, and spinal stabilisation. Other indications included debridement and excision of sinuses. Eight patients of those 30 patients with a history of spine surgery required further surgical treatment (26.67%).
Comorbid disease was rapidly fatal in four patients, ultimately fatal in seven patients, and nonfatal or not present in 97 patients (89.81%) (McCabe and Jackson Classification) [1, 2].
Patient outcomes
Six months after treatment, 11 patients had died, 62 (57.40%) had recovered with residual abnormalities, 35 (32.40%) had recovered fully.
Risk factors for adverse outcome
Fatal outcome was not found significantly associated with the age or sex of patients, the causative organism, bacteraemia, the location of spinal lesions, severity of comorbid diseases, and the rate of complications. For the five patients with valvular cardiac prosthesis, four died although significant association was not found either. Mortality in the eight patients with Gram-negative bacillus was 0% but again significant association was not found. Of the patients with fatal progression (11 cases), four suffered from diabetes mellitus and three had had previous spine infection. We could not find an association, although p value was close to 0.5 between diabetes and fatal illness or previous spine infection and death (p = 0.84).
Discussion
Infectious spondylodiscitis is not an uncommon disease. The annual incidence of the disease ranges from 0.5 to 2.5 cases per 100,000 inhabitants. Although rare, spondylodiscitis is the main manifestation of haematogenous osteomyelitis in patients aged over 50 years [4, 5] and represents 3–5% of all cases of osteomyelitis. In our series 82% of our patients were older than 50 years (Fig. 1) with a mean age of nearly 67 years.
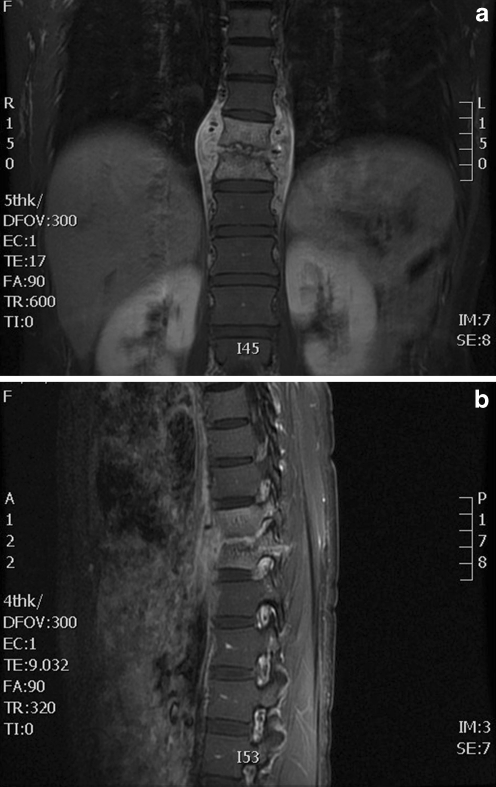
As previously reported in other studies [6–8], MRI is the most sensitive (93–96%) and specific (92.5–97%) modality for early detection of spondylodiscitis. It can differentiate between pyogenic discitis, neoplasia and tuberculosis, providing better definition of paravertebral and epidural spaces (Fig. 5). It also allows optimal assessment of any compression of neural elements [9, 10]. In our study, it was performed in 88 of the patients, subsequently leading to a correct diagnosis.
Fig. 5.
a T-2 weighted coronal magnetic resonance images of the spine demonstrating classic appearance of a disc space infection at D12-L1. b T-1 weighted sagittal magnetic resonance of infection D12-L1
The value of percutaneous biopsy as a safe and minimally invasive intervention is well established. Some experts recommend a second percutaneous biopsy if the first one is negative [11–15]. Friedman [16] reported positive initial percutaneous biopsy cultures for 50% of 24 patients with spontaneous spondylodiscitis, a frequency that improved to 79% on repeat biopsy. Other investigators would consider a negative percutaneous biopsy result as an indication for surgical biopsy, especially if the clinical condition is unsatisfactory [17].
In our series 52% percutaneous discal biopsies were performed to identify the micro-organism. Of these biopsies, we obtained a positive culture in half, in common with previous reports. Blood cultures were taken in 11 patients and were positive in only six cases.
Other authors continue to advocate early biopsy when blood culture is negative [11–15]. Disc space biopsy is associated with minimal morbidity and, for cases in which microbial identification is successful, aids in the selection of appropriate antibiotic therapy.
In our review 78 patients had spontaneous discitis and 30 patients had postoperative discitis (20 in lumbar levels). Not surprisingly, postoperative disc space infections in the lumbar region correspond to the higher ratio of procedures performed on this sector (66 cases) compared to the thoracic or cervical spine. Spontaneous discitis was more evenly distributed among lumbar, thoracic, and cervical disc spaces, although the lumbar disc spaces were still the most frequently involved.
We observed moderate to severe back pain in 97 cases (89.8%); 21 (19.4%) patients had a nerve root compression; six patients had compressive myelopathy. The proportion of patients with neurological manifestations was higher than in earlier studies [2, 18].
Pathogens can infect the spine via three routes: by haematogenous spread, by direct external inoculation, or by spread from contiguous tissues. The haematogenous arterial route is predominant, allowing seeding of infection from distant sites into the vertebral column [6]. Thirty of our cases had undergone previous spinal surgery and 78 were by haematogenous spread. The association of spontaneous discitis with concurrent infection of another organ system in our series supports the argument for haematogenous spread (18 cases presented with a confirmed concurrent infection).
Diabetes and end-stage renal disease were the most significant risk factors for the development of discitis in our experience. Diabetes mellitus was the most common disease occurring in 18 patients (16.6%) followed by ten (9.25%) end-stage renal disease. Other large series have also substantiated the role of diabetes mellitus as a risk factor for the development of spinal infections [19–21]. Systemic illness and infections at other sites were also associated with spontaneous disc space infections
One or more comorbid diseases were present in 56 (51.8%) of 108 patients. Seventeen patients presented two comorbidities and one patient had three comorbidities.
Although a wide range of organisms have been associated with spondylodiscitis (bacterial, mycobacterial, fungal and parasitic), it remains primarily a monomicrobial bacterial infection. S. aureus is the predominant pathogen, occurring in 28% of all positive cultures in our Centre, similar to that reported in the current literature [19–21]. Pseudomonas aeruginosa is an uncommon cause of spondylodiscitis. In a series of 61 patients from 1969–79 with a predominantly intravenous drug user population, P. aeruginosa topped the list of pathogens and was isolated in 48% of cases [22]. This finding has not been replicated in our series with only one case, probably related to the low intravenous drug user population.
Brucellosis, the most common zoonosis in endemic areas, can account for 21–48% of spinal infections, representing the predominant cause in some series from the Mediterranean Basin and the Middle East [6, 23]. Infection occurs secondary to consumption of unpasteurised contaminated dairy products or contact with infected animals. Our population, although framed in the Mediterranean Area, is mainly of urban origin which accounts for the presence of only one case of Brucella.
We reserve operative debridement for patients who need drainage of abscesses, relief of compression of the spinal cord and spinal stabilisation. Other indications included debridement, excision of sinuses and removal of infected hardware. Using this approach, the vast majority of patients went on to resolution of the infection.
Severity of comorbid illness was not an independent risk factor for adverse outcome, we could not find an association between diabetes and fatal illness or previous spine infection and death (p = 0.084). This is possibly because of the relatively small number of patients with rapidly or ultimately fatal underlying diseases (only 11 cases), but these two comorbidities were the closest to a significant statistical correlation.
Whilst initial antimicrobial therapy is almost always administered parenterally, its duration varies considerably. In a multicentre observational prospective study, the mean treatment duration was 14.7 weeks with minimum length ranging from six to 12 weeks according to the treating centre [24, 25]. In our Hospital the mean duration of the antibiotic therapy was over five weeks but this did not worsen the clinical results or increase mortality compared to other studies.
In conclusion, spondylodiscitis has evolved from an acute illness of young patients that had a high mortality rate to a more indolent illness of elderly individuals that has a lower mortality. Early diagnosis is a major challenge. Heightened awareness and the prompt use of MRI are necessary to avoid diagnostic delay. Prolonged antimicrobial therapy and the judicious application of timely surgical intervention are essentials for an optimal outcome.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.McCabe WR, Jackson GG. Gram-negative bacteremia. I. Etiology and ecology. Arch Intern Med. 1962;110:847–855. doi: 10.1001/archinte.1962.03620240029006. [DOI] [Google Scholar]
- 2.McHenry MC, Easley KA, Locker GA. Vertebral osteomyelitis: long-term outcome for 253 patients from 7 Cleveland-area hospitals. Clin Infect Dis. 2002;34:1342–1350. doi: 10.1086/340102. [DOI] [PubMed] [Google Scholar]
- 3.Friedman JA, Maher CO. Spontaneous disc space infections in adults. Surg Neurol. 2002;57:81–86. doi: 10.1016/S0090-3019(01)00681-4. [DOI] [PubMed] [Google Scholar]
- 4.Jensen AG, Espersen F, Skinhoj P, et al. Increasing frequency of vertebral osteomyelitis following Staphylococcus aureus bacteraemia in Denmark 1980–1990. J Infect. 1997;34:113–118. doi: 10.1016/S0163-4453(97)92395-1. [DOI] [PubMed] [Google Scholar]
- 5.Espersen F, Frimodt-Moller N, Thamdrup Rosdahl V, et al. Changing pattern of bone and joint infections due to Staphylococcus aureus: study of cases of bacteremia in Denmark, 1959–1988. Rev Infect Dis. 1991;13:347–358. doi: 10.1093/clinids/13.3.347. [DOI] [PubMed] [Google Scholar]
- 6.Cottle L, Riordan T (2008) Infectious spondylodiscitis. J Infect 56:401–412 [DOI] [PubMed]
- 7.Khan IA, Vaccaro AR, Zlotolow DA. Management of vertebral diskitis and osteomyelitis. Orthopedics. 1999;22(8):758. doi: 10.3928/0147-7447-19990801-07. [DOI] [PubMed] [Google Scholar]
- 8.Varma R, Lander P, Assaf A. Imaging of pyogenic infectious spondylodiscitis. Radiol Clin North Am. 2001;39(2):203. doi: 10.1016/S0033-8389(05)70273-6. [DOI] [PubMed] [Google Scholar]
- 9.Hopkinson N, Stevenson J, Benjamin S. A case ascertainment study of septic discitis: clinical, microbiological and radiological features. Q J Med. 2001;94:465. doi: 10.1093/qjmed/94.9.465. [DOI] [PubMed] [Google Scholar]
- 10.An HS, Seldomridge JA. Spinal infections. Clin Orthop Relat Res. 2006;444:27. doi: 10.1097/01.blo.0000203452.36522.97. [DOI] [PubMed] [Google Scholar]
- 11.Chew FS, Kline MJ. Diagnostic yield of CT-guided percutaneous aspiration procedures in suspected spontaneous infectious diskitis. Radiology. 2001;218:211–214. doi: 10.1148/radiology.218.1.r01ja06211. [DOI] [PubMed] [Google Scholar]
- 12.Hadjipavlou AG, Kontakis GM, Gaitanis JN, et al. Effectiveness and pitfalls of percutaneous transpedicle biopsy of the spine. Clin Orthop Relat Res. 2003;411:54–60. doi: 10.1097/01.blo.0000068184.83581.86. [DOI] [PubMed] [Google Scholar]
- 13.Rankine JJ, Barron DA, Robinson P, et al. Therapeutic impact of percutaneous spinal biopsy in spinal infection. Postgrad Med J. 2004;80:607–609. doi: 10.1136/pgmj.2003.017863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Enoch DA, Cargill JS, Laing R, et al. Value of CT-guided biopsy in the diagnosis of septic discitis. J Clin Pathol. 2008;61:750–753. doi: 10.1136/jcp.2007.054296. [DOI] [PubMed] [Google Scholar]
- 15.Kornblum MB, Wesolowski DP, Fischgrund JS, et al. Computed tomography-guided biopsy of the spine. A review of 103 patients. Spine (Phila Pa 1976) 1998;23:81–85. doi: 10.1097/00007632-199801010-00018. [DOI] [PubMed] [Google Scholar]
- 16.Friedman JA, Maher CO, Quast LM, et al. Spontaneous disc space infections in adults. Surg Neurol. 2002;57:81–86. doi: 10.1016/S0090-3019(01)00681-4. [DOI] [PubMed] [Google Scholar]
- 17.Sapico FL, Montgomerie JZ. Vertebral osteomyelitis. Infect Dis Clin North Am. 1990;4:539–550. [PubMed] [Google Scholar]
- 18.Eismont FJ, Bohlman HH, Soni PL, Goldberg FM, Freehafer AA. Pyogenic and fungal osteomyelitis with paralysis. J Bone Joint Surg Am. 1983;65:19–29. [PubMed] [Google Scholar]
- 19.Kulowski J. Pyogenic osteomyelitis of the spine: an analysis and discussion of 102 cases. J Bone Joint Surg. 1936;18:343–364. [Google Scholar]
- 20.Ross PM, Fleming JL. Vertebral body osteomyelitis: spectrum and natural history: a retrospective study of 37 cases. Clin Orthop. 1976;118:190–198. [PubMed] [Google Scholar]
- 21.Collert S. Osteomyelitis of the spine. Acta Orthop Scand. 1977;48:283–290. doi: 10.3109/17453677708988770. [DOI] [PubMed] [Google Scholar]
- 22.Patzakis MJ, Rao S, Wilkins J, et al. Analysis of 61 cases of vertebral osteomyelitis. Clin Orthop Relat Res. 1991;264:178–183. [PubMed] [Google Scholar]
- 23.Colmenero JD, Jimenez-Mejias ME, Sanchez-Lora FJ, et al. Pyogenic, tuberculous, and brucellar vertebral osteomyelitis: a descriptive and comparative study of 219 cases. Ann Rheum Dis. 1997;56:709. doi: 10.1136/ard.56.12.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Legrand E, Flipo R-M, Guggenbuhl P et al (2001) Management of nontuberculous infectious discitis. Treatments used in 110 patients admitted to 12 teaching hospitals in France. Joint Bone Spine 68:504–509 [DOI] [PubMed]
- 25.Cheung WY, Luk KD (2011). Pyogenic spondylitis. Int Orthop. Oct 28 [Epub ahead of print] [DOI] [PMC free article] [PubMed]