Abstract
Background & objectives:
Adherence to ART is a patient specific issue influenced by a variety of situations that a patient may encounter, especially in resource-limited settings. A study was conducted to understand factors and influencers of adherence to ART and their follow ups among patients attending ART centres in Maharashtra, India.
Methods:
Between January and March 2009, barriers to ART adherence among 32 patients at three selected ART centres functioning under national ART roll-out programme in Maharashtra, India, were studied using qualitative methods. Consenting patients were interviewed to assess barriers to ART adherence. Constant comparison method was used to identify grounded codes.
Results:
Patients reported multiple barriers to ART adherence and follow up as (i) Financial barriers where the contributing factors were unemployment, economic dependency, and debt, (ii) social norm of attending family rituals, and fulfilling social obligations emerged as socio-cultural barriers, (iii) patients’ belief, attitude and behaviour towards medication and self-perceived stigma were the reasons for sub-optimal adherence, and (iv) long waiting period, doctor-patient relationship and less time devoted in counselling at the center contributed to missed visits.
Interpretation & conclusions:
Mainstreaming ART can facilitate access and address ‘missed doses’ due to travel and migration. A ‘morning’ and ‘evening’ ART centre/s hours may reduce work absenteeism and help in time management. Proactive ‘adherence probing’ and probing on internalized stigma might optimize adherence. Adherence probing to prevent transitioning to suboptimal adherence among patients stable on ART is recommended.
Keywords: ART adherence, barriers, beliefs, counselling, financial barriers, India, stigma, service delivery
Provisional estimates show that there are 2.27 million people living with HIV/AIDS (PLWHA) in India by the end of 2008 with an estimated adult HIV prevalence of 0.29 per cent1. National AIDS Control Programme III (NACP III) of the National AIDS Control Organization (NACO) seeks to halt and reverse the epidemic in India by integrating programmes for prevention, care, support and treatment. The goal of the Programme is to provide anti-retroviral therapy (ART) to 3,00,000 adults and 40,000 children by March 2012 and achieve high level of adherence to ART and minimize the number of patients lost to follow up2.
Sustained adherence requires a consistent supply of medications along with education and support3. Government of India has tried to remove the structural barriers for accessing ART by its free ART roll-out programme and a network of link centres4. Many studies have provided evidence that adherence of 95 per cent and above is required for viral suppression, with 80 per cent of near-perfect adherers maintaining an undetectable viral load over six months5. The goal of national ART programme in India is also to attain >95 per cent individual drug adherence rate6. But adherence to ART is difficult, and suboptimal ART regimens may result in rapid development of drug resistance7,8. In real life situation, adherence to medication is a patient related behaviour where he/she has to follow instructions of the health care provider for taking medicines along with diet and lifestyle modifications. However, a patient could face many barriers to adhere to drugs or drug regimen. For example, although overall treatment adherence among sub-Sahara African patients has been high, yet 40 per cent of the HIV infected patients in 33 cohorts in 13 African countries were not retained optimally in care after two years3. The potentially high attrition rates suggested the need for a better understanding of how PLWHA integrate ART and care seeking behaviour in the context of their daily lives to support adherence to treatment and retention in the programme. Thus the definition of adherence has been expanded to include retention in care, which includes attending regular follow up visits9.
In India, of the 179 ART centres, all patients from 15 ART centres showed the ART adherence rate of 95 per cent. Since the inception of National ART programme in 2004, NACO has reported 7 per cent loss to follow up cases and 3 per cent patients who had missed treatment at some point of time10. An assessment of ART centres where exit interviews of the beneficiaries were conducted shows distance from ART centres and economic factors as major reasons for not visiting the centre regularly11. Considering a large number of patients on ART in India, whose disease will progress if adherence or retention in programme is suboptimal, research is urgently needed to determine patient-level barriers to these issues12.
The influence of culture has been evident on how people behave, seek care, and react to health promoting/compromising messages13. While studying patients’ adherence to ART, side effects, inadequate time during consultations, lack of follow up and counselling, forgetfulness and stigma were some of the factors affecting adherence to ART in Zambian and Peruvian patients14,15. It is evident that adherence models inconsistent with local values and practices are bound to fail16. Hence, adherence to treatment and follow up are dependent on patients’ own will and health seeking behaviour which needs to be studied within their own socio-cultural context.
Optimizing adherence and minimizing loss to follow up are two major challenges for the ART roll-out programme in India17. Taking lessons from African scenario3and current situation in the country, a qualitative study was conducted to understand barriers to adherence to ART and follow up visits among patients who were registered or enrolled at government ART centres in Maharashtra State in India.
Material & Methods
Between January and March 2009, an exploratory study was conducted by National AIDS Research Institute (NARI), Pune, India, among patients enrolled at selected three ART centres operated under national ART roll-out programme in Maharashtra, India. The study was reviewed and approved by the Ethics committee of the institute. In a joint meeting of the research team at NARI and Maharashtra State AIDS Control Society (MSACS), three sites were selected to study the barriers to ART adherence. Site I, established in 2004, was situated in an urban location in ‘Vidarbha’ region of Maharashtra. This ART centre had a record of reported loss to follow up of 19-20 per cent. Site II, established in 2005 was situated in a small town of ‘Marathwada’ region of Maharashtra. Site III, a comparatively new centre, was also situated in ‘Marathwada’ region and it was the only rural center in Maharashtra.
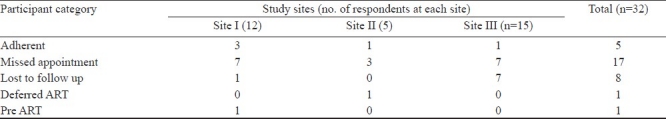
Identification of study participants: A purposive sampling technique was utilized to identify patients (N = 32) in the following categories: (1) Missed appointment (n1 = 17): Patients who had missed follow up, either a clinical or drug pick-up appointment at least by one month. (2) Lost to follow up (LTFU) (n2 =8) : Patients alive and on ART but did not return to the ART centre for 3 continuous months (90 days) and they were, therefore, declared lost to follow up. In addition, other categories of patients were identified as follows: Adherent patients (n3 =5), Patients deferring ART (n4 =1), Patient registered as Pre-ART patient (n 5 = 1). ART centre counsellors or community care coordinators fixed appointments with the identified patients telephonically. Either these patients came for the interview at the centre or the patient gave permission to the study team to visit them at a convenient confidential location of their choice. Due to confidentiality reasons, location of the sites has not been disclosed and the sites have been assigned numbers as I, II and III. The middle numeral in the respondent identification number refers to the site number.
Data collection: In-depth interview guides were developed by the study investigators and modified and finalized in consultations with MSACS. On-site data collection was done by trained researchers. Interviews were conducted in local language and were audio taped. Interviews were transcribed verbatim and translated into English language subsequently.
Data analysis: Data were entered and analyzed in NuD*IST software version 6.0. Constant comparison, conceptualization and categorizing of data using grounded theory approach of Strauss and Corbin18 was used. Codes were compared constantly and grouped into similar categories. Finally emerging relationships between various categories were derived to determine concepts for barriers to ART adherence and follow ups.
Results
A total of 5300 patients were on ART at site I, around 1300 patients at site II and 1600 patients at site III, respectively at the time of data collection. Daily patient load at site I was 200 - 250, while at sites II and III, it was 80-100 and 100-150, respectively. Community c0 are c0 entre with hospice facility was available only at Site I.
Overall, 26 men [mean age 38.69 yr (SD±8.91 yr)] and 6 women [mean age 38.83 yr (SD±11.35 yr)] were interviewed. About half of the participants (15/32) were educated up to secondary school level and nine were illiterate. Eighteen participants (12 men and 6 women) were on ART for less than one year while 12 were on ART for ≥1 yr. One patient was registered as pre-ART and one patient was advised to initiate ART but he was deferring it. The Table describes distribution of patients interviewed for the study at each site. There was no refusal for interview at any of the three centres.
Table.
Site-wise distribution of patients enrolled in the study
Majority (n=25) of the patients reported more than one barrier to ART adherence (78.12%). The main barrier for ART adherence emerged as ‘not having the medicines’ with them. This was a result of not being able to replenish the stock of antiretroviral (ARV) days because of ‘missing a visit’ or ‘not coming to the ART centre at all’. The patients belonged to low socio-economic strata and they mentioned travelling from distant places for reaching to ART centre. It was difficult for them to manage money to come to the centre on appointed day. They also cited reasons such as marriage, funeral or festival for missing visit. Consequently, money and need to attend social functions/duties were reported by patients for missing a visit partially or completely. Hence financial and socio-cultural barriers emerged as themes for missing a visit or becoming LTFU. Patients also shared that they did not want to take their tablets in front of anyone as they were afraid of being stigmatized, indicating that socio-cultural barriers affected ART adherence.
Patients talked about their experiences at the ART centre such as fear of health care providers, long waiting hours as reasons for their reluctance to visit the centre any more. Some of them talked of hours of waiting period. Taking loans to reach the centre on ‘monthly scheduled visit’ was also reported as a reason because there was no provision of dispensing stock of ARVs for more than one month or to the relatives. Some patients said that they wanted to check what happens if they do not take medicine once or twice; some were plainly irritated and some revealed that they did not like to take medicines. Hence a patient related barrier of patients’ attitude and behaviour emerged as barrier to adhere to ART.
Barriers to ART adherence were classified as (i) Financial barriers, (ii) socio-cultural barriers, (iii) patients’ belief, attitude and behaviour, and (iv) experience at facility.
Financial barriers: More than 50 per cent of the participants (18 of 32) reported financial constraint as a barrier for ART adherence attributed to depletion of stock due to missed visits. This barrier was reported by almost equal proportion of the participants from each of the study sites. The reasons for missing scheduled visits to ART centre reported were having nothing for food, no money for travelling, reallocation of money meant for health into purchasing essential commodities, or fulfilling social responsibilities and to repay loans.
Socio-cultural barriers: Attending family ceremonies pertaining to the near/extended families and kith and kin were major social obligations executed by the patients. This culminated into failure to adhere to advised follow up schedule leading to non-adherence, and LTFU. Commitment of attending social functions leds to traveling expenditure. Patients reported fulfilling multiple obligations to effectively utilize money and time spent by extending their visit which resulted in missing ART.
Experience of stigma by relatives and community or fear of being stigmatized if they took medicine or went to ART centre was found as an individual related socio-cultural barrier among the patients.
Patients’ belief, attitude and behaviour: Meaning of ‘adherence’ was understood differently by different patients. One patient reported taking tablets only once a day instead of twice a day which was sub-optimal dose and he felt that he was adherent. Missing ‘few doses’ was common among the patients. They were casual to an extent of experimenting and challenging the very concept of ‘ART adherence’. Patients’ attitude and behaviour towards medication/treatment also influenced their adherence. Patients’ experience of side effect of ART seemed to be an important contributing factor for suboptimal adherence.
Experience at ART centre: Patients from all the three centres (16 of 32) stated experiencing problems pertaining to long waiting hours at ART centre, doctor-patient relationship, working hours and delivery of services at the centre. Patients reported facing problems right from the ART initiation stage when they had to make frequent visits for various tests for ART initiation till they were stable on ART. Patients faced problems for CD4 count tests. They were called several times. It was difficult to manage because they could neither afford the cost of repeat visits nor they had stamina to go to the centre repeatedly.
Another reason for the missed visit was fear of retribution due to missing a visit. Defaulting patients also shared feeling of being scared of facing the health care providers at the centre after missing scheduled visits and out of fear they missed more.
In the national ART roll-out programme, all patients who are on ART need to make ‘monthly visits in person’ for collecting monthly quota of drugs. Finding time and money to reach ART clinic every month was voiced as a problem. Patients requested for medicines for 2-3 months so that they need not make monthly visits, save money and reduce traveling when they are sick or have work.
HIV concordant couples face double burden because there are ‘two’ patients to be managed. Each person has to come for monthly visits which costs money. The problem aggravates further because one partner can be on second line regimen while other on the first line. The programme provides second line treatment at certain centres only and in case of HIV concordant couples the burden is additional.
Patients felt they were not getting adequate time with the health care providers because they were busy in documentation and information provided on how and when to takes medicine was inadequate. Shift to other systems of medicine seemed to occur because of complicated regimen and it was another reason cited for ART interruption.
Discussion
In this study, concerns related to maintenance of optimal adherence to ART among HIV infected patients receiving free ART under ART roll-out programme of Government of India are reported. The patients enrolled in this study provided information on lack of control over adherence due to various factors. The actual access and coverage need to be understood in the context of ART being available ‘free of cost’ in India. The striking finding was lack of financial resources among the patients to access the centre where free ART is available because they could not afford travel cost. On the other hand, social responsibilities appeared to be the major priority for the patients and cost of travelling in such cases did not seem to be a deterrent. This is perhaps a reflection of existing socio-cultural norm of family structure in India where many of the urban households are really offshoots of rural extended or joint families19and thus the members become responsible for numerous social obligations in the family. Although India has free ART roll-out programme, optimal utilization of this programme needs to be carefully planned in context of socio-cultural norms and expected role of an individual in the society. Proper referral and tracking to link ART4centre is the key. These link centres should be better utilized by the patients when patients are unable to visit their primary ART centre because they might be attending social functions or temporarily migrated for seasonal jobs at other places outside the village/city of residence. Link ART centers can also facilitate non absenteeism from their work.
Empowering patients by providing skills to prioritize taking ART over other socio-cultural obligations becomes an imperative for public health. In addition, list of the link centres should be provided to the patients for utilization of the ART services as per patients’ convenience. Efforts should be made to prevent the patient returning without availing services and prevent losing faith in the system. Since this is an operational issue of ART centre, the ART centre team may ensure that every patient who was turned back should get priority appointment and services at the next visit where a coupon system might be of use. Keeping ART centre staff on shift duties or maintaining morning and evening OPDs is recommended so that patients can better manage their time and avoid taking leave from work.
Sometimes patients’ own beliefs and behaviour may lead to missed visits or treatment interruptions. Side effects also deter patient from adhering and if not intervened, it can lead to non-adherence. Patients’ belief and shift to other traditional systems of medicines emerged as another issue of concern as observed in African settings20. In India, traditional medicine practice is common21. Sensitizing alternative medicine practitioners, about ART roll-out programme and importance of adherence to ART would be essential. The effectiveness of ART programme would increase through periodic specialized ART-related training of practitioners of modern and indigenous medicine working in both private and public sectors in India17.
Perceived stigma and patient's own attitude towards pills and treatment also influence adherence to ART. Our study showed that ‘feeling ill’ and ‘being ill’ are two different things. The former is patients’ own experience which drives him or her to seek treatment and be adherent while the latter perception leads to ART interruption. ‘Attitudinal non adherent’ patients should be identified by the counsellors from the beginning by using measurable indicators. Such patients should be given a continuous flow of information on impact of non-adherence on viral load and drug resistance.
Stigma in diverse form was prevalent among the patients. Fear of disclosure of HIV/AIDS status on being seen taking medicines has been a known barrier to ART adherence12,22,23. Regular health check-ups are not a routine practice in India and hence patients avoid going to ART centre on routine basis out of fear of identification. The programme managers may need to work out strategy to change the ‘routine periodicity’ which might also help patients to manage their own travel plans/work schedule without being constricted by the schedule of follow ups at ART centre. An alternative solution would be to mainstream ART dispensing.
Suboptimal ART adherence is known to result in the rapid development of drug resistance24. There is a need to develop processes to maintain a continuum of supply of ARVs to the patients by preventing missed visit which triggers the vicious cycle of treatment interruptions, sickness, and lack of stamina among patients to make a visit to ART centre. Rehearsal of how to procure money to travel to ART centre on schedule as part of adherence counselling could be initiated among patients registered at ‘pre ART’ itself. The key message should focus on maintaining stock of ARV drugs and minimizing disadvantages of missed visits.
Our study also shows that cost and time doubles or sometimes trebles if more than one family member is on ART. Moreover, additional cost occurs if members of a family are on different ART regimens. This means their primary centres are differently located. To ensure uninterrupted supply of ARVs, another strategy could be dispensing drugs to the family members for their sick or working relatives. Proper assessment of the problem or certification by competent person or patient could be useful in case of dispensing drugs to someone other than the patient. In this study, missed visits and LTFUs were primary reasons for missing ART. Barriers to adherence/missed visit/ LTFU need to be overcome by using novel strategies in counselling. We propose ‘adherence probing’ as an addition to standard adherence counselling. Adherence probing should include addressing issues of ‘possibility of side effects’, unconditional assurance of no reprimand if the patient comes back after a missed visit and discussing plans for traveling at each visit. An innovative strategy could be to provide small travel pill kit with stock of ARV for a few days. Further studies need to be conducted to evaluate impact of interventions suggested.
In conclusion, a broad range of barriers have been identified for ART non-adherence in this study. The major barriers to adherence were at individual level and socio-cultural. Adherence counselling focusing on events when a patient may fail to come for follow up due to various attitudinal, financial, socio-cultural and service delivery reasons needs to be probed and intervened at every visit. Mainstreaming HIV and drug dispensing, flexible visit schedules and suitable OPD hours at ART centres could enhance patient retention under care and treatment continuum of India's free ART roll-out programme.
References
- 1.Department of AIDS Control, Ministry of Health and Family Welfare. Annual report 2009-2010. [accessed on August 13, 2011]. Available from: http://www.nacoonline.org/upload/AR%202009-10/NACO_AR_English%20corrected.pdf .
- 2.National AIDS Control programme III, National AIDS Control Organization, Ministry of Health and Family Welfare (2006) Goals and objectives. [accessed on June 8, 2010]. Available from: http://www.nacoonline.org/National_AIDS_Control_Program/
- 3.Rosen S, Fox MP, Gill CJ. Patient retention in antiretroviral therapy programs in Sub-Saharan Africa: A systematic review. PLoS Med. 2007;4(10):e298. doi: 10.1371/journal.pmed.0040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Operational Guidelines for Link ART Centers. National AIDS Control Organization, Ministry of Health and Family Welfare, Government of India. 2008. [accessed on June 13, 2010]. Available from: http://nacoonline.org/Divisions/CST/Link_ART_Centers/
- 5.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squire C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 6.Antiretroviral therapy guidelines for HIV-infected adults and adolescents including post-exposure prophylaxis. Ministry of Health and Family Welfare, Department of AIDS Control. 2007. May, [accessed on September 30, 2011]. Available from: http://www.nacoonline.org/
- 7.Wang X, Yang L, Li H, Zuo L, Liang S, Liu W, et al. Factors associated with HIV virologic failure among patients on HAART for one year at three sentinel surveillance sites in China. Curr HIV Res. 2011;92:103–11. doi: 10.2174/157016211795569122. [DOI] [PubMed] [Google Scholar]
- 8.El-Khatib Z, Katzenstein D, Marrone G, Laher F, Mohapi L, Petzold M, et al. Adherence to drug-refill is a useful early warning indicator of virologic and immunologic failure among HIV patients on first-line ART in South Africa. PLoS One. 2011;6:e17518. doi: 10.1371/journal.pone.0017518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel A, Hirschhorn L, Fullem A, Ojikutu B, Oser R. Adult aherence to treatment and retention in care. Arlington, VA: USAID | AIDSTAR-ONE PROJECT, Task Order 1; 2010. [Google Scholar]
- 10.CMIS Bulletin, (April 2008 to Sept 2008). National AIDS Control Organization, Department of AIDS Control, Ministry of Health and Family Welfare, Government of India. [accessed on April 13, 2011]. Available from: http://www.nacoonline.org/upload/Care%20%20Treatment/ functional%20LAC%20centers%20July%202010.pdf .
- 11.Sogarwal R, Bachani D. Assessment of- ART centers in India: client perspectives. J Indian Med Assoc. 2009;107:276–80. [PubMed] [Google Scholar]
- 12.Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, et al. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Med. 2006;3:e438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaturvedi S, Arora N K, Dasgupta R, Patwari AK. Are we reluctant to talk about cultural determinants? Indian J Med Res. 2011;133:361–3. [PMC free article] [PubMed] [Google Scholar]
- 14.Sanjobo N, Frich JC, Fretheim A. Barriers and facilitators to patients’ adherence to antiretroviral treatment in Zambia: a qualitative study. SAHARA J. 2008;5:136–43. doi: 10.1080/17290376.2008.9724912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curioso WH, Kepka D, Cabello R, Segura P, Kurth AE. Understanding the facilitators and barriers of antiretroviral adherence in Peru: a qualitative study. BMC Public Health. 2010;10:13. doi: 10.1186/1471-2458-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sankar A, Golin C, Simoni JM, Luborsky M, Pearson C. How qualitative methods contribute to understanding combination antiretroviral therapy adherence. J Acquir Immune Defic Syndr. 2006;43(Suppl 1):S54–68. doi: 10.1097/01.qai.0000248341.28309.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sahay S, Ghate M, Mehendale S. Managing HIV Therapy literacy in resource- limited settings. HIV Ther. 2009;3:339–44. [Google Scholar]
- 18.Strauss A, Corbin JM. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, California: Sage; 1990. [Google Scholar]
- 19.Singh JP. Problems of India's changing family and state intervention. [accessed on April 29, 2011]. Available from: http://www.un.org/esa/socdev/family/docs/egm09/Singh.pdf .
- 20.Dahab M, Charalambous S, Hamilton R, Fielding K, Kielmann K, Churchyard GJ, et al. “That is why I stopped the ART”: patients’ & providers’ perspectives on barriers to and enablers of HIV treatment adherence in a South African workplace programme. BMC Public Health. 2008;8:63. doi: 10.1186/1471-2458-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pandikumar P, Chellappandian M, Mutheeswaran S, Ignacimuthu S. Consensus of local knowledge on medicinal plants among traditional healers in Mayiladumparai block of Theni District, Tamil Nadu, India. J Ethnopharmacol. 2011;134:354–62. doi: 10.1016/j.jep.2010.12.027. [DOI] [PubMed] [Google Scholar]
- 22.Kumarasamy N, Safren SA, Raminani SR, Pickard R, James R, Krishnan AK, et al. Barriers and facilitators to antiretroviral medication adherence among patients with HIV in Chennai, India: a qualitative study. AIDS Patient Care STDs. 2005;19:526–37. doi: 10.1089/apc.2005.19.526. [DOI] [PubMed] [Google Scholar]
- 23.Nachega JB, Knowlton AR, Deluca A, Schoeman JH, Watkinson L, Efron A, et al. Treatment supporter to improve adherence to antiretroviral therapy in HIV-infected South African adults.A qualitative study. J Acquir Immune Defic Syndr. 2006;43(Suppl 1):S127–33. doi: 10.1097/01.qai.0000248349.25630.3d. [DOI] [PubMed] [Google Scholar]
- 24.Reynolds SJ, Bartlett JG, Quinn TC, Beyrer C, Bollinger RC. Antiretroviral therapy where resources are limited. N Engl J Med. 2003;348:1806–9. doi: 10.1056/NEJMsb035366. [DOI] [PubMed] [Google Scholar]


