Fig. 5.
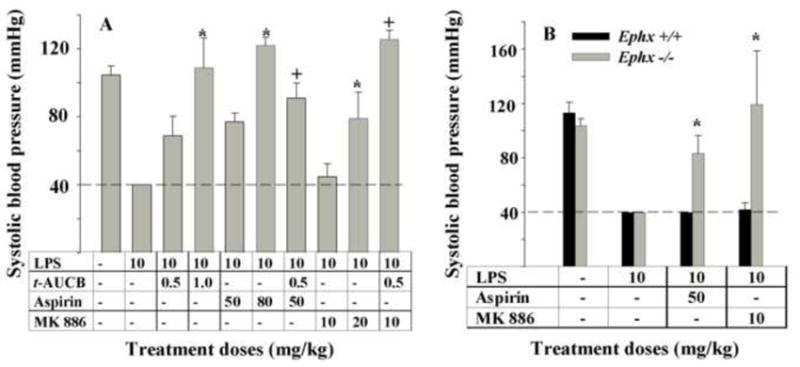
Selective modulation of branches of the AA cascade during a murine model of inflammation results in unexpected anti-hypotensive effects. Animals were treated as detailed in Fig.2 and systolic blood pressure was monitored 4 h after LPS administration. (A) LPS administration led to a profound decrease in blood pressure that was lower than the detection limit (40 mm Hg) of the instrument used (dashed line). Both doses of t-AUCB, and aspirin significantly reversed LPS-induced hypotension but MK 886 was effective only at a high dose. However, co-administration of the low doses of t-AUCB and MK 886 led to a synergistic reversal of blood pressure. Similarly, co-administration of t-AUCB and aspirin resulted in stronger reversal of hypotension. *Significantly different from its lower dose alone (P > 0.05) and † significantly different from the individual inhibitors alone as determined by ANOVA followed by Tukey’s posthoc comparison test. (B) The baseline systolic blood pressure of wild-type (black bar, n = 6) and Ephx2-null (gray bar, n = 4) mice were not different and LPS administration led to a similar decrease in both strains of mice. Aspirin or MK886 administration both led to reversal of hypotension only in the Ephx2-null mice but not in wild-type conspecifics. * Significantly different from Ephx2 wild mice control (P > 0.05) determined by by ANOVA followed by Tukey’s posthoc comparison test.
